MOJ
eISSN: 2374-6939


Case Report Volume 14 Issue 3
Orthopedic Surgery, Valley Consortium for Medical Education, USA
Correspondence: Rex Saito, Valley Orthopedic Surgery Residency, 1400 Florida Ave, Modesto, California, USA, Tel (209) 573-6183
Received: June 11, 2022 | Published: June 30, 2022
Citation: Saito R, Beckett R, Frazier J. An aberrant palmaris brevis causing ulnar nerve comression at Guyon’s canal: An anatomic case report and literature review. MOJ Orthop Rheumatol. 2022;14(3):84-85. DOI: 10.15406/mojor.2022.14.00583
There have been reports of ulnar nerve compression due to anatomic variations at Guyon’s canal. Knowledge of certain variations at Guyon’s canal may help hand surgeons identify possible unconventional compression sites of the ulnar nerve. We present a case report of a patient with an aberrant palmaris brevis muscle belly that was found to cross over the proximal aspect of the ulnar tunnel neurovascular bundle potentially causing ulnar nerve symptoms. Surgical interventions with the release of the palmaris brevis muscle belly and transposition to the flexor carpi ulnaris tendon at the level of Guyon’s canal helped provide relief of the patient’s ulnar nerve symptoms.
Keywords anomalous muscles, palmaris brevis, guyon’s canal, ulnar nerve, ulnar tunnel syndrome
The ulnar nerve is a branch off the medial cord of the brachial plexus that traverses throughout the upper extremity and innervates the medial side of the forearm, ulnar side of the palm, little finger, and ulnar half of the ring finger. It’s motor branches innervates the flexor profundus of the little and ring fingers, flexor carpi ulnaris, hypothenar muscles, adductor pollicis brevis, and all the interossei and third and fourth lumbricals. Compression of this nerve can occur at multiple sites throughout the upper extremity causing ulnar neuritis. Ulnar Tunnel Syndrome is where the ulnar nerve is compressed at ulnar tunnel, also known as Guyon’s canal which was first described by DuPont et al. in 1965.1 Compression of the ulnar nerve at the wrist may be caused by factors such as ganglion cysts, lipomas, ulnar artery thrombosis, trauma, and anatomic anomalies. There have been reports of compression of the ulnar nerve by anomalous muscles at the level of the wrist.2–4 Anatomic anomalies of the wrist are not uncommon. Dodds et al. described a 22% incidence of anomalous muscles at Guyon’s canal during a series of cadaveric wrist dissections.5 Another study utilizing MRI of Guyon’s canal also found similar results with a 25% prevalence of anomalous muscles within the tunnel with 67% of these occurring bilaterally.6 Examples of anomalous muscles that have been reported include flexor digiti minimi, abductor digiti minimi, flexor carpi ulnaris, palmaris brevis profundus, accessory or reversed palmaris longus.7,8 We report a case report of an aberrant palmaris brevis muscle belly that was found to cross over the proximal aspect of the ulnar tunnel neurovascular bundle potentially causing ulnar nerve symptoms.
Our patient is a 33-year-old right hand dominant male with a pertinent surgical history of right carpal tunnel release and right cubital tunnel release with submuscular ulnar nerve transposition performed by a surgeon in the community two years prior to presentation. The patient complained of worsening of pain, weakness, tremors, loss of coordination, numbness and tingling in the right small and ring finger and wasting of his hand. Physical exam demonstrated a positive Tinel's sign at the carpal, cubital, and ulnar tunnel. A positive Froment’s sign, intrinsic fatigue and first web space and hypothenar atrophy was also observed. A needle electromyogram (EMG) was performed and demonstrated decreased conduction velocity of the right ulnar motor nerve. The ulnar sensory nerve also showed reduced amplitude. The right median nerve demonstrated decreased conduction velocity suggestive of carpal tunnel syndrome. MRI of the right brachial plexus was also performed and no abnormalities were identified. After discussion with the patient, a revision cubital tunnel, carpal tunnel, and primary ulnar tunnel release was offered.
Approximately two months after presentation, the patient was taken to the operating room. An extended curvilinear incision in line with the ulnar side of the fourth ray was carried across the forearm wrist crease of the right upper extremity. Starting proximally and working distally the antebrachial fascia of the forearm was released. At this point, an aberrant palmaris brevis muscle belly with origin from the hypothenar musculature was noted. The muscle belly was short oblique in nature. After extending the incision proximally, it was noted that the aberrant palmaris brevis inserted into the tendinous slip of the palmaris longus which crossed over the proximal aspect of the ulnar tunnel neurovascular bundle. The muscle belly was then released from the palmaris longus, transposed, and inserted onto the flexor carpi ulnaris tendon so that it was no longer crossing over the ulnar neurovascular bundle.
At the first post-operative appointment, the patient reported improvement with sensation in his arm. He was subsequently enrolled in occupation therapy and continued to improve in strength in his extremity with his last follow up visit being 3 months.
Ulnar tunnel syndrome arises from compression of the ulnar nerve at Guyon’s canal. Compression of the nerve may be caused by several factors including ganglion cysts, lipomas, giant cell tumors, ulnar artery aneurysms, and muscular anomalies. Trauma and fractures to this region leading to ulnar nerve compression has also been described.9 Shea and McClain first classified ulnar nerve compression into three zones which can produce different symptoms.10 Compression at Zone I occur proximal to Guyon’s canal just proximal to the bifurcation of the ulnar nerve into its motor and sensory branches. This causes both mixed motor and sensory deficit in the ulnar nerve distribution. Zone II is described to be at the distal aspect of Guyon's canal and affects the deep motor branch of the ulnar nerve causing motor deficits only. Zone III occurs at the distal end of Guyon's canal but affects only the sensory branch. In our case, the aberrant palmaris brevis was compressing the neurovascular bundle at Zone I just proximal to Guyon's causing a mixed motor sensory deficit (Figure 1 & 2).

Figure 1 Aberrant palmaris brevis muscle belly originating from hypothenar muscles and attaching to the palmaris longus overlying Guyon's canal.
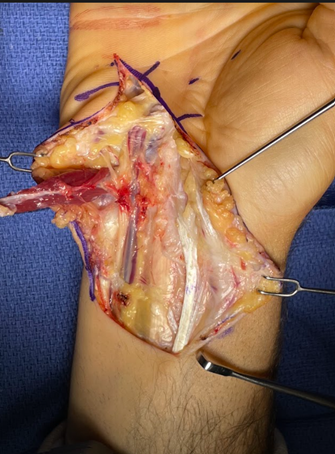
Figure 2 Palmaris brevis muscle released from palmaris longus demonstrating ulnar neurovascular bundle.
Anomalous muscles at the wrist have been described previously by many authors. Most times they are considered clinically insignificant. However, surgeons must be aware of these anomalies as they can potentially cause compression of neurovascular structures.2 Of anomalous hypothenar muscles, variations of the adductor digiti minimi are most frequent.11 Other anomalous hypothenar muscles include opponens and flexor digiti minimi, palmaris brevis profundus, and accessory or reversed palmaris longus.8 Many different anomalous variations of either the palmaris longus or palmaris brevis has been described. The reversed palmaris longus muscle was first described in 1916 as possessing a distal musculotendinous junction which may hypertrophy and potentially divide distally into 2 or 3 separate attachments. This anatomic variation has been reported to extend ulnarly and insert with the flexor carpi ulnaris onto the pisiform or traverse Guyon’s canal with the abductor digiti minimi.12 A case report by Regan and colleagues described ulnar nerve compression that was caused by a reversed bifid palmaris longus muscle.12 Tonkin and colleagues described an anomalous muscle as palmaris brevis profundus which caused ulnar nerve compression at the wrist. In their case they described the anomaly as a thick muscle belly that was parallel to, but separate from a more superficial, thin palmaris brevis muscle. This muscle in their report lay between the superficial and deep branches of the ulnar nerve causing compression.5
When treating patients with ulnar tunnel syndrome, the surgeon must be aware of all potential causes of compression, including anatomic anomalies. Most times, anomalous muscles are considered clinically insignificant and may be found incidentally. However, in cases of recalcitrant symptoms, surgeons should have a high index of suspicion for these anomalies as potential culprits. In our case, we believe that the aberrant palmaris brevis was causing recalcitrant ulnar nerve compression at Zone I.
None.
The Authors declare that there are no conflicts of interest.

©2022 Saito, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.