MOJ
eISSN: 2374-6939


Case Report Volume 16 Issue 5
1Department of Medical Education and Research, Kaohsiung Veterans General Hospital, Kaohsiung 813414, Taiwan
2School of Medicine, National Defense Medical Center, Taipei, Taiwan
3School of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
4Department of Physical Medicine and Rehabilitation, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
5Department of Physical Medicine and Rehabilitation, Tri-Service General Hospital, School of Medicine, National Defense Medical Center, Taiwan
Correspondence: Shin-Tsu Chang, Department of Physical Medicine and Rehabilitation, Kaohsiung Veterans General Hospital, Tri-Service General Hospital, School of Medicine, National Defense Medical Center, Taipei, No. 386, Dazhong 1st Rd., Zuoying Dist., Kaohsiung 813414; No. 161, Section 6, Minquan East Road, Neihu District, Taipei 114201, Taiwan, Tel 886-7-3422121; 886-935605578
Received: December 15, 2024 | Published: December 31, 2024
Citation: Yung-Cheng C, Yu-Jing K, Ling-Chun S, et al. A rare case of cavitated Schmorl’s node in the cervical spine: imaging features of bone scan and magnetic resonance. MOJ Orthop Rheumatol. 2024;16(5):278-281. DOI: 10.15406/mojor.2024.16.00686
Schmorl’s node is formed when the nucleus pulposus of an intervertebral disc herniates upward or downward an adjacent vertebral endplate or subchondral trabeculae. Some Schmorl’s nodes may present as big cystic lesions, differing significantly from the typical form. This study reports a rare case of Schmorl’s node with cavitation, a presentation distinct from both classic and cystic Schmorl’s nodes. We present a case of a 44-year-old male with neck pain and restricted cervical motion, whose skeletal scintigraphy showed a cavitated Schmorl’s node, which might be caused by upward nucleus pulposus of the intravertebral disc into a cervical vertebra, presumed by magnetic resonance images. This report describes a rare case of cavitated Schmorl’s node and highlights its unique imaging characteristics. It demonstrates that conservative treatment can be an effective approach for managing cavitated Schmorl’s nodes.
Keywords: Schmorl’s node, cystic lesion, Schmorl’s node with cavitation, herniated disc, intravertebral hernia, spinal disc, scintigraphic rehabilitation
Neck pain is a common symptom with numerous causes, including muscle strain, tears, compression or irritation of the spinal nerves, and degeneration or damage to the bones and joints.1ss However, Schmorl’s node cannot be ignored, which is an intravertebral hernia of the spinal disc (nucleus pulposus) into the vertebral endplate or into subchondral trabeculae. Clinically, most cases are asymptomatic, but some patients may present with back pain.2 Typical Schmorl’s node is relatively straightforward to diagnose on imaging and is often characterized by indiscretions of the vertebral contour or minute radiolucent lesions surrounded by reactive sclerosis.3
Interestingly, some Schmorl’s nodes may present as big cystic lesions, which are markedly different from the typical form and pose significant diagnostic challenges, which formation is thought to be similar to that of subchondral cysts, often resulting from trabecular bone fractures, local hemorrhage, or disruption of blood supply caused by trauma or mechanical stress.4 This report describes a rare case of Schmorl’s node with cavitation, a unique presentation distinct from both typical and cystic forms. The aim of this study is to characterize the radiological characteristics of this lesion using traditional radiography, bone scan, and MRI, and to explore the potential mechanisms underlying the cavitation formation.
A 44-year-old male presented with neck pain, ulnar-sided left wrist pain, and left shoulder pain accompanied by an inability to lift the shoulder. In June 2024, he visited the emergency department due to neck pain and restricted rightward cervical rotation (approximately 45°); however, his symptoms did not fully resolve. In September 2024, after a fall, he experienced worsening left wrist and shoulder pain, with complete inability to lift the arm, significantly impacting his daily life. His past medical history included right-sided pneumothorax caused by trauma.
Clinical examination revealed tenderness confined to the neck and upper back, as well as tenderness in the lower back and sacroiliac joints. Cervical rightward rotation and left shoulder elevation were restricted. Laboratory tests showed a mildly elevated eosinophil count (8.0%). Imaging studies, including cervical spine AP and lateral X-rays, demonstrated C5-C7 intervertebral space narrowing and retrolisthesis. Tc-99m methylene disphosphonate (MDP) whole body bone scan with whole-body imaging was arranged, and localized imaging with single-photon emission computed tomography (SPECT)-CT for cervical-thoracic spines confirmed increased radiotracer uptake in the C6 vertebra, identifying a 0.7 cm cystic lesion (Figure 1). On T1-weighted images, the intervertebral disc was clearly seen herniating into the C6 vertebra, with the herniated portion connecting to the cavitated lesion (Figure 2A). Another image (Figure 2B) demonstrated the C7 vertebra compressing the intervertebral disc upward, causing partial rupture. On T2-weighted images, the cavity appeared hypointense (Figure 3A & 3B), and a distinct ring of sclerosis surrounds the cavity (Figure 3B), which is characteristic of Schmorl's cyst.4 Based on axial images (Figure 3C), it is suggested possible prior communication with cerebrospinal fluid. Furthermore, degenerative disc disease (DDD) was noted at C3-C4 and C4-C5, while C5-C6 and C6-C7 showed DDD with grade I retrolisthesis.
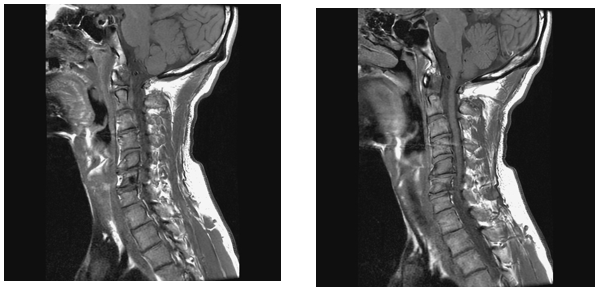
Figure 2 On T1-weighted images, the intervertebral disc was clearly seen herniating into the C6 vertebra, with the herniated portion connecting to the cavitated lesion (Figure 2A). Another image (Figure 2B) demonstrated the C7 vertebra compressing the intervertebral disc upward, causing partial rupture.
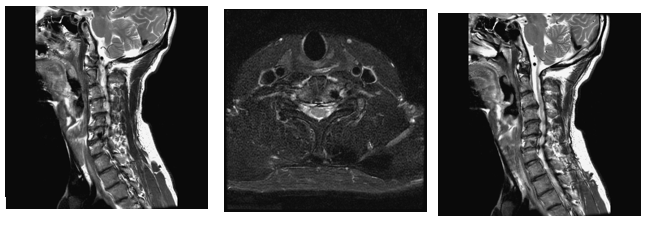
Figure 3 On T2-weighted images, the cavity appeared hypointense (Figure 3A, B), and a distinct ring of sclerosis surrounds the cavity (Figure 3B). On (Figure 3C) images suggested possible prior communication with cerebrospinal fluid..
The imaging findings excluded malignancy or metastatic lesions in the C6 cyst, leading to a diagnosis of Schmorl’s node with cavitation. Thus, no further pathological biopsy was performed. Based on the imaging evidence of increased radiotracer uptake in C6, the treatment plan included oral non-steroid anti-inflammatory drug Diclofenac (Meitan) 25 mg QID and muscle relaxant Phenprobamate (Mocolax) 400 mg QID to alleviate symptoms and stabilize the lesion. Additionally, interferential current combined with laser therapy was used to address neck and upper back pain, while infrared and transcutaneous electrical nerve stimulation were applied to manage acute wrist and shoulder pain. After three months of treatment, the patient showed significant improvement in neck pain, with cervical rotation increasing from 45° to 80°. The acute pain and restricted joint mobility in the left wrist and shoulder also resolved. The patient has since returned to normal work and remains active.
This patient presented neck pain and restricted range of motion, and showed two significant findings: increased uptake and cavitation at the C6 vertebra on the bone scan, and disc rupture upward with invasion into the C6 vertebral body on MRI. We will discuss this case in terms of its radiologic features, differential diagnosis, pathophysiological mechanisms, and clinical implications. To our knowledge, this is the first case to show such interesting findings.
In view of radiologic evaluation, proper image provided critical insights into the pathology. X-ray imaging revealed that the vertebral contour remained intact, with no evidence of aggressive bone destruction (not shown). On the bone scan, there was increased radiotracer uptake in the C6 vertebra (Figure 1), consistent with the first scintigraphic findings in Schmorl’s node.5 MRI images showed the intervertebral disc herniating into the C6 vertebra, with the herniated portion connecting to the cavitated lesion (Figure 2A & 2B), and the C7 vertebra compressing the intervertebral disc upward, causing partial rupture. Also, the cavity of C6 appeared hypointense (Figure 3A & 3B), with a distinct ring of sclerosis surrounds the cavity (Figure 3B), which is characteristic of Schmorl's cyst.4 MRI findings further clarified the pathology of Schmorl’s node, which typically appears a small bony notch filled with herniated disc material in the upper or lower endplate of a vertebral body.6
With respect to differential diagnoses for spinal cysts or cavities, the pathology of simple bone cyst (SBC), aneurysmal bone cyst (ABC), brown tumor, infection, and giant cell tumor should be considered. For SBC and ABC, both lesions typically exhibit high T2 signal intensity due to their fluid content.7 However, SBCs arise within the bone and do not exhibit features of nucleus pulposus of intravertebral hernia, as clearly observed in Fig. A. On the other hand, ABCs often have a multilobulated contour and demonstrate fluid-fluid levels on imaging,8,9 features that are not observed in this case. Regarding brown tumor and giant cell tumor, these lesions frequently cause expansible bone destruction and mass effects, and demonstrate fluid levels or internal septations.10–13 However, the MRI findings in our case showed no signal enhancement, effectively excluding these neoplastic lesions. For infection, infectious lesions typically present with surrounding soft tissue edema and T2 hyperintensity.14–16 In this case, these features were not present, and clinical data did not support infection. Although SPECT-CT revealed increased radiotracer uptake, there were no additional findings to suggest an infectious process, which was not considered as well.
In the field of scintigraphic rehabilitation, bone scan together with SPECT-CT can be utilized as the first line to detect pathology, particularly useful in the localization of the exact site of pain/tender area.17–31 for instance, early inspection of cavitation in the C6 vertebra with increased uptake, like our case. After all, images with function are far better than images with only structure. What's more, SPECT-CT has both functional and structural images, which will prevent clinicians from misdiagnosing.
On the subject about the mechanism of the formation of cystic lesions, it is hypothesized to be similar to that of subchondral cysts which result from trabecular bone fractures, local hemorrhage, or disruption of blood supply caused by trauma or mechanical stress, and these processes lead to bone necrosis, followed by fibroblast proliferation and degeneration of connective tissue, ultimately forming a cyst.4 A similar process may occur at the disc-vertebral junction, owing to its synovial joint-like structure, which consists of cartilage-covered endplates, surrounding fibrous tissue, and a nucleus pulposus that resembles synovial fluid.4 With respect to the mechanism of cavitation formation of this case, the upward intravertebral hernia of the spinal disc through the endplate and its connection to the cavity suggests that the cavitation likely originated from a Schmorl’s node. It is hypothesized that mechanical stress or trauma initially led to the configuration of a Schmorl’s cyst at the disrupted endplate. Over time, fluid resorption within the cyst resulted in the development of the observed cavitation. Based on imaging findings and after excluding other differential diagnoses, this sequence of events, we presumed, provides a plausible explanation for the observed cavitary lesion.
Regarding the treatment and prognosis, medication and physical therapy can effectively manage his cavitated Schmorl’s nodes. The patient’s symptoms improved significantly within three months, and imaging showed no further progression. Invasive treatment can be avoided in similar cases once malignancy has been excluded. For clinical implication, the patient’s symptoms of neck pain and restricted motion were likely associated with local inflammation or bone remodeling. SPECT-CT findings of increased radiotracer uptake in C6 further support the hypothesis of ongoing inflammatory or reparative processes. However, the potential impact of the cavitated Schmorl’s node on long-term vertebral stability remains unclear and warrants further investigation.
This case highlights a rare Schmorl’s node with cavitation, distinct from both typical and cystic forms. His symptoms of neck pain and restricted motion were likely due to localized inflammation and bone remodeling. SPECT-CT findings of increased radiotracer uptake further supported the diagnosis in scintigraphic rehabilitation, so SPECT-CT as an add-on for precise diagnosis in clinical practice. In this case enhances the existing literature by serving as a reference for the diagnosis and management of similar lesions. However, the long-term effects of Schmorl’s node cavitation on vertebral stability remain uncertain and require further investigation.
None.
The authors declare that there are no conflicts of interest.

©2024 Yung-Cheng, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.