MOJ
eISSN: 2374-6939


Although the volume of total knee Arthroplasties (TKAs) performed around the world continues to increase, recent studies on patient satisfaction as the primary outcome measure have shown that up to 30% of the patients remain unsatisfied. Especially in younger individuals, TKAs are associated with higher rates of revision and with decreased patient satisfaction. Because of these reports, several manufacturers have implemented specific design modifications and have increased the modularity of their systems. However, little is known of the safety and functionality of these newer designs. This editorial note highlights recent advances in TKA implant designs, focusing on the reported outcomes of high-flex and extremely modular new primary TKA designs.
Keywords: Total knee arthroplasty, TKA, Implant design, Total joint, High-flex, Modularity
TKA, Total Knee Arthroplasty; ROM, Range-Of-Motion; PS, Posterior-Stabilized; KSS, Knee Society Score; PCL, Posterior Cruciate Ligament; ML, Medio-Lateral; AP, Antero-Posterior
Total knee arthroplasty (TKA) continues to be very effective in providing pain relief and improved function since the early 1970s when Insall and Coventry introduced the total condylar prosthesis. In this timeframe, the number of primary total knee replacements performed in the United States outside from Federal Hospitals reached 719,000 in 2010.1 If the number of TKA performed continues to growth at the current rate, the demand for primary TKA is projected to reach 3.48 million procedures by 2030.2 Although the results of classic TKA designs have been previously reported as excellent with a 93% survival rate at 15 years.3 recent studies focusing on patient satisfaction as the primary outcome measure have been less encouraging, with the Ontario Joint Registry showing that only 70% of patients met their expectations one year after TKA.4 This “un-satisfaction” rate is also higher in younger individuals requiring early intervention because of severe knee osteoarthritis: Parvizi et al.5 reported only 66% of young patients (< 60 years) indicating their knees feeling normal at 1 to 4 years after primary TKA. Because of these reports, in recent years, several manufacturers have implemented specific design modifications in the attempt to improve patient outcomes: between those modifications, high-flexion femoral components and increased modularity (femoral, tibial, polyethylene thickness and patellar sizes) have captured particular attentions by many designers. In this editorial note, we evaluate the evidence concerning the introduction of these two device technologies (high-flexion femoral components and increased implants modularity) in primary TKA.
High-Flexion Designs
Surgeons have traditionally emphasized knee flexion as a hallmark of clinical success.6 As a result, in the last ten years, manufacturers have introduced novel designs with specific features targeting high flexion. Design features include a reduced posterior femoral condylar radius with thickened posterior femoral condyles when compared with traditional femoral components (Figure 1) to improve the physiological femoral postero-lateral rollback during range-of-motion (ROM) activities. In addition, manufacturers have attempted to improve implants kinematics by altering the radius of curvature of the femoral component: currently, two main variations exist: the single-radius (Figure 2) and multi-radius/J curve designs (Figure 3). Although many daily activities are known to require up to 120° of flexion and up to 19° of axial rotation.7 numerous studies, including from the Author’s own experience, have demonstrated postoperative knee flexion to rarely exceed 120°.8 raising questions about the ability of modified implants to reproduce the normal “in vivo” knee biomechanics.
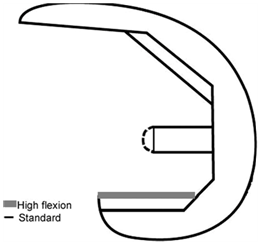
Figure 1 Femoral component of a posterior-stabilized (PS) TKA system: design differences between a standard and a high-flex design.

Figure 2 Left Knee: GMK Sphere TKA system (Medacta, Castel S. Pietro, Switzerland). The femoral component is characterized by a single radius of curvature.
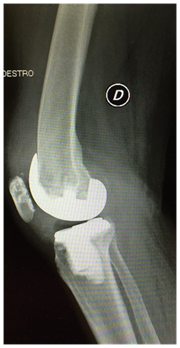
Figure 3 Right Knee: lateral x-ray. The femoral component is characterized by a J curve design (Persona, The Personalized Knee System, Zimmer, Warsaw, USA).
Unfortunately, in current time, numerous studies have failed to demonstrate significant improvements in clinical outcomes or survivorship with high-flex designs. A recent systematic review of mid-term and long-term follow-up studies.9 showed no statistically significant improvement in postoperative flexion when standard TKA designs were compared with their high flexion replacements. At the same time, no relevant increase in classic postoperative outcome measures (Knee Society Score and Hospital for Special Surgery Score), or better survivorship were reported when analyzing the results of more modern high-flex TKA designs. Nunley et al.10 in a 2015 study, found no differences between high-flex and 10-year old CR designs with regard to patient satisfaction and residual symptoms in patients younger than 60 years. Thomsen et al.11 in a double-blind randomized study testing a standard and an high-flex design in opposite knees in the same patient, questioned the clinical relevance of improved ROM after TKA, since patients showed no differences in satisfaction scores between the two implants. Kim et al.12 compared survivorship and osteolysis in a series of 100 patients who had undergone bilateral knee replacements. Each patient had one standard posterior-stabilized implant, with the other side being a high-flexion type implant. At a minimum 10-year follow-up, no differences were found in survivorship, functional outcome, range of motion, or degree of osteolysis between the two groups.
Since novel implants cost more, it is mandatory to demonstrate superior outcomes compared to older designs before their widespread use. Unfortunately, the recent literature has failed to demonstrate overall significant improvements when high-flex designs have been utilized: to date, reservations regarding their clinical utility may still remain.
TKA Implants Modularity
Today’s most popular TKA designs follow two basic approaches: functional and anatomic. Functional approaches gained widespread popularity because of their simplified knee kinetics. Anatomical approaches, on the other side, attempt to recreate normal knee motion decreasing contact stresses. The small inventory needed of functional knee designs ultimately lead to their overwhelming success and market dominance. The large library of anatomic implants sizes needed has brought on their failure to achieve widespread production.
At the same time, in our modern times, TKA systems are intended for use on the global population. Popular functional knee designs were originally characterized by 2 symmetric condyles mimicking the individual condylar J-curve and a single piece tibial tray with a centered peg for cement fixation.13,14 Later on, John Insall and Al Burstein worked together to improve the posterior-stabilized (PS) design of the tibial plates in order to obtain a more posterior contact point of the condyles on the tibial tray with increased flexion: in this matter, a cam and post mechanism, which allowed progressive femoral rollback with flexion replacing the function of the posterior cruciate ligament (PCL), was developed and introduced to the market.15 In the last few decades, the development of functional designs revealed the addition of more implant size options (“increased modularity”) to accommodate the large range of knee sizes and geometries. In fact, numerous morphologic studies have demonstrated high variability in the size and shape of the human knee, especially of the distal femur.16 While left and right throclear flanges were added early to functional designs, a larger range of femoral medio-lateral (ML) and antero-posterior (AP) options, an increased number of tibial symmetric and asymmetric designs and an increased number of tibial insert thicknesses have been recently introduced by the major orthopaedic manufacturers. It remains unclear whether the increasing number of implants size options is cost effective and especially beneficial to patients.
In a digital three-dimensional model study using knee CT reconstructions, Dai et al.17 investigated component fit in six contemporary femoral component design families, showing that contemporary femoral component designs characterized by extreme modularity (12 femoral sizes, 9 tibial sizes, 6 patellar sizes and 8 different poly thicknesses for every tibial poly size) resulted in improved femoral component fit across various ethnicities.
In the clinical setting, things might be different. Nunley et al.10 reported the impact of modern designs with an improved modularity on patient satisfaction and functional outcomes in the most challenging patient population: patients younger than 60 years old. In their study, the authors found overall few differences between classic (cruciate retaining) and modern TKA designs, including gender specific with high modularity.
In a recent study (unpublished data), the current author aimed to assess for potential patient-reported functional benefits and report short-term outcomes of a newer extremely modular PS TKA design (Attune, De Puy-Synthes, Warsaw, USA) when compared with its predecessor (Sigma PS, De Puy-Synthes, Warsaw, USA). A consecutive group of 100 patients (Group 1) undergoing TKA using a classic cemented fixed-bearing PS TKA system (Sigma PS, De Puy-Synthes, Warsaw, USA) was matched by age, gender, BMI to 100 patients (Group 2) having the newer (Figure 4A & 4B) cemented fixed-bearing PS design (Attune, De Puy-Synthes, Warsaw, USA), both by the same manufacturer. Patients were assessed preoperatively, at 12 months and at 24 months minimum follow-up (range, 24-46) in a standard prospective fashion. The outcome assessments used were the Oxford Knee Score, the Knee Society Score (KSS), range-of-motion (ROM) and a satisfaction survey. A two-sample t-test comparing the two groups was performed.
At 2-year follow-up, differences in clinical and radiological KSS (p=0.09), Oxford Score (p=0.08) and overall satisfaction rate did not reach statistical significance. Implant group 2 showed a statistically significant decrease in postoperative anterior knee pain (p=0.006). At final follow-up, 16 % of group 1 knees achieved > 130° flexion compared with 37% in group 2 (p=0.0009). There were two revisions for any reason in group 1 and none in group 2. In that study, the current author showed that design modifications applied to the newer TKA system allowed greater flexion and lower anterior-mechanism complications but did not appear to achieve better overall clinical scores at final follow-up.
With the orthopaedic community and industry striving to improve outcomes following knee arthroplasty surgery, newer TKA implants with distinct design features have been introduced into the market. While improvements in perioperative pain management, computer assisted technologies, and polyethylene quality resulted in improved clinical results, the merits of high-flexion and extremely modular designs are still yet to be realized. Because newer implants cost more, it is mandatory to demonstrate superior outcomes compared to older designs before their widespread use.
None.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.