MOJ
eISSN: 2575-9094


Case Report Volume 2 Issue 5
1Department of Physical Therapy, Hungkuang University, Taiwan
2Department of Physical Medicine and Rehabilitation, Taichung Veterans General Hospital, Taiwan
Correspondence: Shin-Tsu Chang, Department of Physical Medicine and Rehabilitation, School of Medicine, National Defense Medical Center, No.161, Sec. 6, Minquan East Road, Neihu District, Taipei, Taiwan; Department of Physical Medicine and Rehabilitation, Taichung Veterans General Hospital, 1650Taiwan Boulevard Section 4, Taichung, Taiwan, Tel: +886-4-23741350
Received: September 17, 2018 | Published: October 3, 2018
Citation: Fang-Chuan K, Shin-Tsu C. Fade-out of perioral tremor after administration of L-DOPA: role of thalamus in pathophysiology of post-stroke rabbit syndrome. MOJ Drug Des Develop Ther. 2018;2(5):193-196. DOI: 10.15406/mojddt.2018.02.00061
Rabbit syndrome is an extrapyramidal side effect that has been linked with chronic antipsychotic therapy. We report herein a rare case of rabbit syndrome that occurred withoutin administration of a neuroleptics naive patient. A 90‒year old female exhibited a perioral tremor movement disorder resembling rabbit syndrome, although she the patient revealed no previous psychiatric history and had never taken antipsychotic medication. Single photon emission computed tomography (SPECT) revealed increased perfusion of the right basal ganglia and left thalamus. Treatment with L‒DOPA Madopar faded out resolved the movement disorder, and the second reevaluation by SPECT showed that basal ganglia/thalamus perfusion had returned to baseline. Rabbit syndrome is an extrapyramidal side effect that has been linked with chronic antipsychotic therapy. We present a rare case of rabbit syndrome in a patient naive to antipsychotics that was associated with increased perfusion of the basal ganglia. The underlying cause of the movement disorder and altered perfusion in this case is unknown. However, standard treatment antiparkinsonian treatment for antipsychotic induced rabbit syndrome was effective in this case indicating involvement of the dopaminergic or cholinergic system.
Keywords: perioral tremor, rabbit syndrome, single photon emission computed tomography, basal ganglion, antipsychotic
Rabbit syndrome, termed for the resemblance to a rabbit chewing, is characterized by regular movements of the oral and masticatory musculature at a frequency of 4 to 6Hz without involvement of the tongue.1 Most commonly, rabbit syndrome is associated with prolonged exposure to antipsychotics and has a prevalence of 2‒5% among these patients.2 Because the symptoms are associated with drug treatment, rabbit syndrome is described as an extrapyramidal side effect of antipsychotics that is seen most often in middle‒aged to elderly patients. In addition, rabbit syndrome has been described in a limited number of cases to arise in antipsychotic patients without administration of antipsychoticsnaive patients, although in all of these cases, rabbit syndrome was secondary to a brain structural abnormality or mood disorder.3‒5 Rabbit syndrome can be distinguished from tardive dyskinesia by the latter involving motion of the tongue while the former sparing the tongue, and this distinction is important because tardive dyskinesia worsens whereas rabbit syndrome improves with antiparkinsonian medication.1,2,5‒7 The mechanism responsible for antipsychotic‒induced rabbit syndrome is thought to involve dopamine receptor blockade in the basal ganglia.7 Furthermore, one study showed decreased basal ganglia perfusion by single photon emission computed tomography (SPECT) in a patient displaying rabbit syndrome.8 Here, we report a case of rabbit syndrome in an antipsychotic naïve naive patient with increased basal ganglia/thalamus perfusion during symptoms.
A 90‒year‒old, right‒handed female visited the gastrointestinal (GI) department of our hospital on October 28, 2005 with complaints of poor appetite and low grade fever. The patient was admitted to the GI ward under the impressions of ileus and pyuria. On November 18, 2005, the patient developed poor muscle power, right hemiplegia, and disturbed consciousness. Magnetic resonance imaging (MRI) of the brain revealed acute left side cerebral infarction Figure 1(A‒B) and an old lacunar infarction on the right side Figure 1(C‒D) Inpatient rehabilitation was arranged for neurological recovery. On December 21, 2005, the patient's caregiver noted prominent involuntary movement around the mouth similar to a rabbit's behavior. Upon inquiry, the patient revealed no previous psychiatric history and had never taken antipsychotic medication. On examination, a rhythmic lip‒oral movement was observed, and the frequency was measured to be 4 to 5Hz. However, the frequency of movement increased when she was stressed or distracted and decreased during voluntary activities such as talking. There was no involvement of the tongue, and lip‒oral movements were absent during the patient's sleep. We observed no abnormal movements anywhere else on the body. Based on these symptoms, a diagnosis of rabbit syndrome was made. An MRI study (on November 21) of the patient's brain produced unremarkable findings aside from the previous lesions. To further investigate the syndrome, the regional cerebral perfusion scan with an ethyl cysteinate dimer (ECD) single photon emission computed tomography (SPECT) SPECT scan of the patient's brain was performed, which revealed increased perfusion of the right basal ganglia and left thalamus Figure 1A & Figure 2A. The patient was prescribed the antiparkinsonian medication Madopar (levodopa/benserazide), 250mg bid (January 2‒9). After 7 days, the abnormal oral motions faded outré solved, the hemiplegia was mildly improved, and the other symptoms resolved resolved. Upon fade‒outre solution of the patient's symptoms after 7days, Madopar was discontinued, and one week later (January 23) we repeated the SPECT scan to reevaluate perfusion of the basal ganglia. Findings from the SPECT scan indicated that basal ganglia perfusion had returned to normal. Furthermore, the scans indicated decreased uptake in the left thalamus Figure 1F & Figure 2B. Once the patient exhibited relative recovery of muscle strength of her right limbs, she was discharged on January 23, 2006.
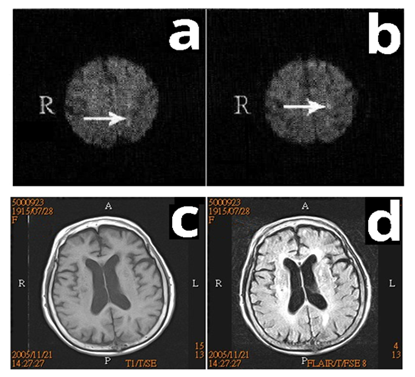
Figure 1 In our a 90‒year‒old female patient, brain magnetic resonance imaging showed 2‒3multiple small acute infarctions in the left frontoparietal lobes in DWI (A‒B), old infarctionts in the left paracentral gyri (not shown) and right periventricular white matter in T1‒weighted images (A‒C) and FLAIR images (C‒D). No obvious lesions were found in the basal ganglion or thalamus.
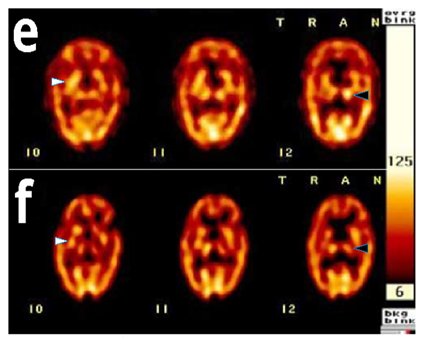
Figure 2 Brain single photon emission computed tomography images showed obtained during and after rabbit syndrome in our patient. A Iincreased uptake in the right basal ganglia (while arrow head) and left thalamus (black arrow head) during presentation of the rabbit syndromedisorder (E), and later after fade‒out, there were n. B. Normal uptake in the right basal ganglia and decreased uptake in the left thalamus were noted after resolution of the condition (F).
In this report, we describe an antipsychotic without naive patient with rabbit syndrome that was associated with increased basal ganglia and thalamic perfusion, as measured by SPECT. Rabbit syndrome is most commonly associated with prolonged exposure to antipsychotics. In a limited number of reports, rabbit syndrome has been described to result from a brain dysfunction, such as structural lesion or dysfunction in processing,3‒5 which three reports assumed that.3,4 In both cases, rabbit syndrome resembles parkinsonism. It is and it is thought that altered dopamine function in the basal ganglia underlies rabbit syndrome.7‒9 For example, in patients chronically exposed to antipsychotics, dopamine D2 receptor blockade is thought to lead to rabbit syndrome, thereby explaining extrapyramidal effects.9,10 Therefore, antiparkinsonian medication, which acts to boost dopamine levels, effectively treats rabbit syndrome. The Table 1 compares findings in our patient displaying rabbit syndrome with patients reported by prior three articles.3‒5 In each of these threewo previous reports, rabbit syndrome was not effectively controlled with antiparkinsonian drugs. Of them specifically, showed that anticholinergics and Levadopa were ineffective at treating the oral symptoms.3 Likewise, showed anticholinergics to be ineffective at treating rabbit syndrome in a patient thought to display the syndrome due to generalized brain dysfunction. However, only low doses of the anticholinergic were administered in this study.4 The Our patient described in the current case report had never received neuroleptics before symptom presentation. Moreover, we observed dramatic improvement in rabbit syndrome symptoms following administration of antiparkinsonian drug Madopar, which acts to increase dopamine levels in the brain. Therefore, this is the first description to our knowledge of an antipsychotic without naive patient with rabbit syndrome who was effectively treated with antiparkinsonian drug, similar to the well‒known treatment regimen for antipsychotic induced rabbit syndrome.1,2,5‒7 Interestingly, our SPECT findings revealed increased uptake in the right basal ganglia during the onset of rabbit syndrome, which decreased once the oral movement disorder faded out resolved. Our report shows a strong relationship between the onset of rabbit syndrome and basal ganglionbrain perfusion. Several studies have demonstrated abnormal basal ganglia function in a variety of conditions, such as pain traumatic brain injury and various posture and movement disorders.11‒20 Extrapyramidal movement disorders, such as Huntington's chorea, Parkinson's disease and rabbit syndrome, have been described to involve decreased perfusion of the basal ganglia.21,22 In contrast, increased perfusion of the basal ganglia has been described in patients with schizophrenia, especially in those with auditory hallucinations,13 but it has never been described in patients with rabbit syndrome. To the best of our knowledge, this is the first report to describe increased uptake in the basal ganglia upon presentation of rabbit syndrome. However, these findings need to be corroborated by further case reports.
Authors initials of patient |
Age (years) |
Gender sex |
Diagnosis |
Priorevious parkinsonian symptoms |
Location of lesion (Findings of MRI* or SPECT†) |
Truong et al (1990)3 |
76 |
Female |
Brain meningioma |
None |
MRI: Left frontal cortex |
Kelvin et al (1993)4 |
76 |
Female |
Depression |
None |
None |
Park et al (2016)5 |
23 |
Male |
Medullary compression by vertebral artery dolichoectasia |
None |
MRI: markedly tortuous right vertebral artery compressing the ventral medulla |
Kuo & Chang (2018)1 |
90 |
Female |
Stroke |
None |
Right basal ganglion MRI: Multiple small acute infarctions in left frontoparietal lobes. Old infarctions in left paracentral gyri and right periventricular white matter. SPECT (1st): Uptake in right basal ganglion and left thalamus higher than usual. SPECT (2nd): Uptake in right basal ganglion is not unusual, but decreased uptake in left thalamus. |
Table 1 Characteristic list of reported cases of rabbit syndrome without administration of neuroleptics
The mechanism responsible for antipsychotic‒induced rabbit syndrome is thought to involve dopamine receptor blockade in the basal ganglia.8 Furthermore, one study showed decreased basal ganglia perfusion by SPECT in a patient displaying rabbit syndrome.23 In contrast, increased perfusion of the basal ganglia has been described in patients with schizophrenia, especially in those with auditory hallucinations,24 but it has never been described in patients with rabbit syndrome. To the best of our knowledge, this is the first report to describe increased uptake in the basal ganglia upon presentation of rabbit syndrome. Another interesting thing is the role of thalamus, the first SPECT findings revealed increased uptake in the left thalamus during the onset of rabbit syndrome, which decreased after administration of L‒DOPA. One of substructures of basal ganglion, substantia nigra pars reticulate, has been thought to be involved in the pathophysiology of rabbit syndrome.8 Animal studies have been confirmed a direct connection between substantia nigra pars reticulate and thalamus.25,26 A simple modulation of nigral activity may induce β‒band activity in the thalamus.26 We believe that the regional cerebral blood flows in thalamus positively responds to those of basal ganglion,27 e.g. simultaneously increasing or decreasing in both structures. However, these findings need to be corroborated by further case reports.
The occurrence of rabbit syndrome is rare in antipsychotic patients without antipsychoticsnaive patients. To our knowledge, report of an antipsychotic naïve naive patient with rabbit syndrome, and associated decrease in basal ganglia perfusion, that is responsive to antiparkinsonian treatment has not previously been documented in the literature. This report extends our understanding of parkinsonism‒related disorders and confirms the role of antiparkinsonian drugs in the treatment of the rabbit syndrome.
None.
None.

©2018 Fang-Chuan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.