MOJ
eISSN: 2381-179X


Case Report Volume 4 Issue 5
1Department of Microbiology, Lokmanya Tilak Municipal Medical College & General hospital, India
2Department of Orthopaedics, LokmanyaTilak Municipal Medical College & General hospital, India
Correspondence: Uma Tendolkar, Professor, Department of Microbiology, Lokmanya Tilak Municipal Medical College & General hospital, Sion, Mumbai 400 022, India, Tel 91-22-24076381
Received: December 31, 2015 | Published: July 21, 2016
Citation: Tendolkar U, Sheth B, Baveja S, et al. Unusual presentation of Madurella mycetomatis mycetoma in a paediatric patient in India. MOJ Clin Med Case Rep. 2016;4(5):109-111. DOI: 10.15406/mojcr.2016.04.00103
Eumycetoma due to Madurella mycetomatis is of worldwide occurrence. It usually presents with signs of tumefaction, sinuses and grains which are the hallmarks in diagnosis of the disease. The present case was an eight year old boy admitted with moderate swelling of the forearm with a discharging sinus. The swelling had developed over a four month period. He gave history of trauma one year back to the site. He also had fever for two months. Imaging studies showed large cystic lesions in the bone. On surgical exploration it was observed that a large mass of compacted black grains (5cmX4cm) was filling the space between the radius and ulna bones. A mycological examination of the black grains revealed fungal hyphae and culture showed growth of Madurella mycetomatis. An extensive surgical debridement and voriconazole treatment for 6weeks relieved the clinical symptoms but there was little radiological improvement. This case represents a rare presentation of mycetoma with a rapid progression of the disease over a few months, not commonly seen with eumycotic agents. The young age of the patient and the site were unusual findings. The external signs were mild and disproportionate to the extensively destructive disease seen underneath. These findings highlight the importance of an early diagnosis to prevent the devastation caused by this relentless infection which may be especially challenging in cases like this which present with unusual features.
Keywords: mycetoma, eumycetoma, madurella mycetomatis, fungal mycetoma, voriconazole, subcutaneous mycosis, sinus
Mycetoma is a chronic subcutaneous infection caused by actinomycetes (actinomycetoma) or fungi (eumycetoma). It evokes a chronic granulomatous inflammatory response in the deep dermis and subcutaneous tissue and can extend to the underlying bone. It is characterized by tumefaction, sinuses and grains. Actinomycetoma are generally fast growing than eumycetomas. In both the types of mycetomas, foot is the commonly involved site. Forearm involvement is rarely seen. This infection is also very uncommon below 15years of age. The present pediatric case is an unusual one due to the site of mycetoma which was the forearm, the rapid progression and the deceptive lesion with comparatively mild signs of the disease on the exterior skin which were disproportionate to the devastating disease underneath.
The patient was a young boy of 8years age who hailed from Siddharthnagar area of Uttar Pradesh state in India. He presented with pain, swelling and draining sinus in the right forearm for 4months. He had history of fever for 2months. He also gave a history of trauma to the forearm one year back with breach of skin and probably abscess formation which was treated with incision and drainage at his native place. The patient was symptomless for about 8months. Thereafter he developed swelling over the forearm and there were no external signs of inflammation. Local examination showed tenderness, swelling and a seropurulent discharge from a sinus at the drainage site. The supination-pronation movement of the forearm was greatly restricted. General examination did not reveal any abnormality. Hematological investigations revealed mild leukocytosis (WBC count 15000/mm3) and raised ESR (60mm at the end of 1hour). Other haematological parameters were within normal limits. Ray of the forearm revealed extensive bone destruction (Figure1A). The ultrasonography was suggestive of Infective osteomyelitis with a collection of 3.7x4.7cm. The MRI study showed soft tissue collections in proximal forearm between radius and ulna (Figure 1B).The patient then underwent surgical exploration which revealed cavity between radius and ulna which was full of a black mass. The mass was composed of abundant black grains which may have been discharged in the bony cavity from the surrounding soft tissues. The cavity was further being expanded by the growing mass of fungal grains. Black grains were also observed interspersed in the surrounding tissue. (Figures 2A) (Figure 2B). The debrided material was received for fungal culture. When observed in 10% potassium hydroxide, it showed plentiful brown cementing material interspersed with fungal hyphae (Figure 2C). On culture, a slow growing mould was observed on Sabouraud’s dextrose agar at both 260C and 370C, which was tan at first becoming brownish later. A diffusible brown pigment was observed in the agar and the fungus was identified as Madurella mycetomatis (Figures 3A) (Figure 3B).1
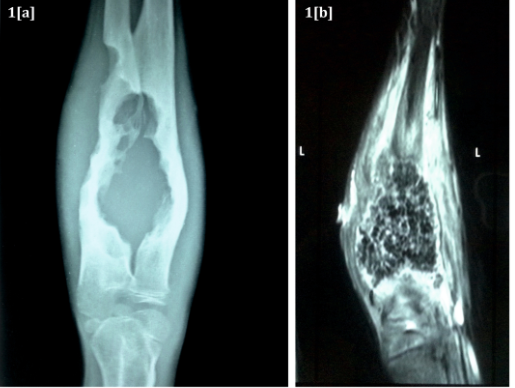
Figure 1A X ray of forearm showing extensive bone destruction with cortical irregularity and sclerosis.
Figure 1B MRI showing massive soft tissue collection between radius and ulna.
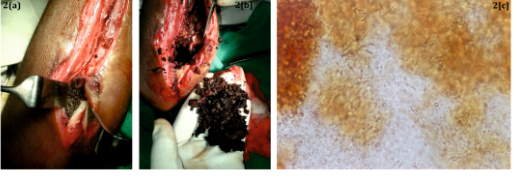
Figure 2 A. Intra operative view of the collection of black grains between the bones
B. Black grains debrided from the tissues.
C. The grains observed microscopically in 10% KOH. Few fungal hyphae embedded in abundant brown cementing amorphous material. X100.

Figure 3A Culture of Madurella mycetomatis on Sabouraud’s dextrose agar. Flat mould with suede like texture and brown diffusible pigment.
Figure 3B Lactophenol cotton blue mount of M. Mycetomatis showing septate sterile hyphae.
A diagnosis of black grained mycetoma caused by Madurella mycetomatis was made based on the clinical and mycological findings. An extensive surgical debridement was done and the patient was started on intra venousvoriconazole 6mg/kg/day. Within six weeks of treatment, externally, the wound healed completely (Figure 4), however an ultrasound examination showed refilling of the lesion. No further intervention was unfortunately possible due to the request by the patient to return to his native place and he was discharged against medical advice. For the past one year, the patient has not followed up. Mycetoma, unless treated appropriately, is a relentless infection and often culminates in amputation of the limb. The very idea of amputation may be a deterrent for the patient to seek medical care.
Eumycetoma is a common but completely neglected disease even in recent times.2 It usually affects adult males. In children the disease is uncommon and foot is commonly involved site. In a retrospective study spanning 25years, out of 334mycetomas, only 2 cases of eumycetoma were encountered in children of 15years or younger (0.6), only 4.5% patients out of 3343 were in this age group and foot was affected in 66.6% of them. Both the eumycetomas in this study were caused by Madurella mycetomats. By far, the commonest agent of eumycetoma worldwide is M.mycetomatis. In India also it has been reported as the predominant agent of eumycetoma.4 It usually affects young adults between 20 to 40years age5 but no age is exempted. Mycetoma can affect any part of the body but foot is most commonly affected (70%), followed by hands (12%), then legs and knee joints.6 Very rarely, other body parts are affected.
Mycetoma is a slowly progressive disease presenting in early stages as a subcutaneous swelling. The first signs may appear quite late. In some patients with short history it may present with massive swelling, involvement of deeper tissues and bone and in contrast, others may present with few, long standing skin lesions with no substantial deeper tissue destruction. Mycetoma generally affects individuals who are otherwise normal but very rarely cases in immunocompromised patients are reported, like one in the foot of a recipient of an allogenic stem cell transplant but the course of the disease did not seem to be unusual in the patient7 and the disease responded to surgery and voriconazole treatment. Our case was a peculiar one with very few superficial signs of the disease but with massive deep tissue destruction. The progress of mycetoma depends on the site involved, the causative organism and probably the hosts defenses and the incubation time is not well defined.2 In our case, the patients ought tertiary health care facility attention only when the forearm became incapacitated with the deeper tissue destruction. The confirmatory diagnosis of mycetoma is by culture of the causative agent. Other methods of diagnosis are aspiration cytology, ultrasonography, histology and immuno diagnosis.8 Magnetic resonance imaging has been shown to be informative in the detection of mycetoma.9 Madurella mycetomatis is a slow growing fungus. The grains in tissues accumulate extracellular cement with melanin which acts as a barrier protecting the fungus from the host immunity and antifungal agents. The natural habitat of this fungus is still an enigma but its DNA has been detected in plant and soil.2 The most effective treatment is possible only when cases are diagnosed early in the course of disease. Surgery is effective in early encapsulated mycetomas especially when combined with antifungal drugs and when bone is not involved.6 The newer triazoles like voriconazole and posaconazole have been tried as potential agents for treatment for eumycetomas with some success.10
This case is of clinical and mycological interest because of several peculiarities. Its occurrence in a child, its sheer destructive nature which underlines the importance of a high degree of suspicion a clinician must have in diagnosing it at an early stage which would make it more easily manageable especially when the typical history and signs are misleading. The comparative mild external signs which belied the devastative lesions in deeper tissues. The sheer abundance of the grain formation was also remarkable.
None.
The author declares no conflict of interest.

©2016 Tendolkar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.