MOJ
eISSN: 2381-179X


Case Report Volume 11 Issue 1
1Department of Otorhinolaryngology, People’s Hospital of Ordos Dongsheng District, China
2Department of Neurology& Neurosurgery, People’s Hospital of Ordos Dongsheng District, China
3Beijing Ivheart Health Management Co., LTD, China
Correspondence: Chunhui Yang, Beijing Ivheart Health Management Co., LTD, China
Received: December 10, 2020 | Published: January 5, 2021
Citation: Han Y, Zhang J, Yang C. Tympanic membrane perforation, otitis media and labyrinthitis caused by otomycosis confirmed by intravenous gadolinium 1.5 tesla MRI—a case report. MOJ Clin Med Case Rep . 2021;11(1):1-3 DOI: 10.15406/mojcr.2021.11.00369
Otomycosis is a fungal ear infection, mostly a superficial mycotic infection of the outer ear canal. The infection may be either subacute or acute but chronic form is around 10%. The characteristic of otomycosis are discharge, pruritus, or more severe discomfort. Here we report a 46-year-old Asian woman presented with vertigo and was diagnosed as otomycosis with the complications of tympanic membrane perforation, otitis media and labyrinthitis of inner ear which was confirmed by IV-Gd 1.5 T MRI. This case is a chronic otomycosis related to cerumen removal two year before this onset.
Our study supported the suggestion that otomycosis should include fungal infections of the middle and inner ear, furthermore the infection of the inner ear may be included as labyrinthitis with the symptom of vertigo.
Keywords: otomycosis, tympanic membrane (TM) perforation, labyrinthitis, intravenous gadolinium (IV-Gd) inner ear 1.5 tesla MRI
In a general otolaryngology clinic setting, Otomycosis is a common illness and its prevalence is around7% in the patients with signs and symptoms of otitis externa.1-22 In 1840s,Dr. Andral, Gavarret and Mayer first described fungal infections of the external auditory canal and later Dr. Virchow recommended the term ‘otomycosis’.23-25 It has been well known that Aspergillus and Candida species are the most recognized fungal pathogens in otomycosis.5,9,14 In about 75% cases of otomycosis, Aspergillus species alone stands the participating mediator.2,5,21,23
The risk factors involved trauma to the ear, chronic skin conditions, having diabetes mellitus, swimming in the contaminated water. In addition, the arrangement of the ear, long-term treatment with topical antibiotics / steroid preparations, wearing hearing aids are all the risk factors.3,12 Dry skin, mild discharge in the ear canal are the common findings for an otomycosis. In addition, hearing loss followed by pruritis, otalgia and TM perforation are common discoveries as well.2,5,7,9,10
There are rare reports that otomycosis can invade further than the outer ear and pierce the eardrum or travel to place that may include the inner ear.14,21 Here we report a case of otomycosis with vertigo except that the common findings of otomycosis. On examination, TM perforation, otitis media and labyrinthitis were confirmed. Our study not only supported the suggestion that otomycosis should include fungal infections of the middle ear, but also gave rise to a new advice that chronic otomycosis should be treated thoroughly to prevent the inner ear from the damage.
A 46-year-old Asian woman presented to our hospital with persistent dizziness with spinning for 2 days. Two days ago, when she woke up in the morning, vertigo occurred. She felt spinning either closing or opening eyes. One week prior to this visit, her left ear presented pruritis and purulent substance, accompanied by mild bass tinnitus. Two years ago, the patient visited a local hospital due to discomfort in her left ear. The examination revealed her left ear was filled with cerumen, then the procedure of cerumen removal was completed. After that, she had intermittently experienced leakage of fluid from the external auditory canal of the left ear. However, she did not have any other symptoms. She did not receive any treatment. Her past medical history did not display hypertension, diabetes, or Meniere’s disease. On Physical examination, sustained right nystagmus and high pitch hearing loss in left ear were observed. Ear endoscopy revealed grayish white debris with black fuzzy growth confined to the walls of the external auditory canal and a well circumscribed area of granulation tissue on the tympanic membrane, the watery and purulent discharge was existed as well.
Blood test shows the elevation of the count of WBC and neutrophil, while the count of lymphocyte was decreased. In addition, ESR and CPR were elevated.
Acoustic immittance was normal. Intravenous Gadolinium (IV-Gd)1.5 T MRI showed the features of labyrinthitis in the left ear (Figure 1).
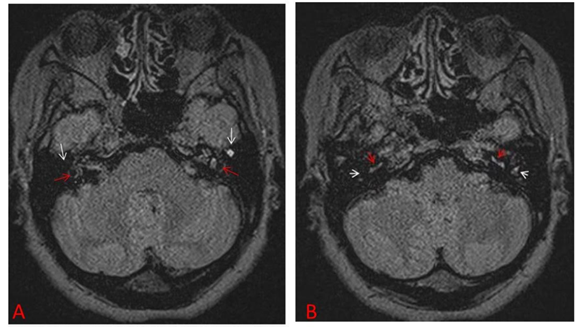
Figure 1 Findings on the IV-Gd1.5 T MRI.
(A)White arrow indicated the location of the middle ear and the red arrow pointed to the vestibular of the inner ear, both structures in the left side showing higher density in than those in the right ones. (B) White arrow pointed to the middle ear and the red arrow to the location of the base turn of cochlea, indicating both structures showing higher density in the left side than those in the right ones.
The biopsy with the lesion of the superficial epithelial masses of debris was performed. Microscopic examination showed the evidence of a fungal infection, tons of containing hyphae fungi were seen (Figure 2).
Combined the clinical signs and symptoms, as well as the imagine and the pathological findings, the diagnosis of otomycosis, otitis media and labyrinthitis were made.
In the treatment, first mechanical debridement of visible fungal elements in the external auditory canal was achieved, then empirical antifungal treatment with 1% clotrimazole ear drop was used in external ear canal and eardrum. One week later, the congestion and edema of the outer ear canal disappeared. However, the eardrum remained edematous and congested, so intraperitoneal clotrimazole injection started. During the local tympanic injection, fluid leakage above the posterior eardrum was found, suggesting TM perforation.
In addition, due to the sign of labyrinthitis on MRI and the increased CBC, ESR and CPR, the system treatment started with clotrimazole. Two weeks later, the vertigo and tinnitus gradually improved. CBC, ESR and CPR returned to the normal range. One month later, the eardrum did not reveal edematous and congested. The closure of the TM perforation was confirmed.
Although otomycosis is a superficial mycotic infection of the outer ear canal frequently confronted by otolaryngologist and can be diagnosed through clinical analysis.1-24 In acute otomycosis, fungal was overgrowth in the ear canal exposed to excess moisture.18,11,23 In this situation, the application of appropriate topical antifungal agents together with frequent routine debridement in less than two weeks usually results in prompt resolution of symptoms in most of cases.4,8,13,22 About 10% of otomycosis is chronic form.5,7,9 Our case became a chronic otomycosis probably due to her living in a very dry and cool climate and did not receive any treatment.
As the respect to the risk factors for otomycosis, some thought lack of cerumen may benefit to fungal growth.7,9,23 The otomycosis in our patient may be produced from cerumen removal two years ago.
The most common chief complaint for otomycosis is pruritis which has been frequently refer to as one of the characteristic symptoms up to 93% in some studies.5,7-10,16 In addition, ear pain and hearing loss are common.8,10 As for the treatment, the topical clotrimazole had good efficacy against both aspergillus and Candida species.8,19,20,22 But When TM perforation and inner ear infected existing, typically system antifungal treatment or surgical management are needed.
The pathophysiology of the TM perforation may be ascribed to avascular necrosis of the TM because of mycotic thrombosis in the adjacent blood vessels.1,6 Some reports indicated TM involvement is expected a consequence of fungal inoculation of the external canal or direct extension of the disease from adjacent skin.1,6,14 Although there were no clinical features foresighted TM perforation, Physicians need to have a high level of suspicion of otomycosis as a cause of persistent ear pain, because otalgia is a prominent feature as a concurrent perforation of the tympanic membrane.1,6,9 The TM perforation was observed to occur during treatment. Some reports suggested treatment strategy for closure of the perforation by surgical procedure after otomycosis had been well known. A natural closure of the TM perforation in our case was confirmed in the follow up one month later.
Through reviewing the literature, we found that otomycosis seldom involve inner ear and cause vertigo, although some authors suggested that this medical term should be expanded and include fungal infections of the middle ear and open mastoid cavities.6,9 Our patient presented significant vertigo and the labyrinthitis of the inner ear infected by fungal, which provided a strong evidence that labyrinthitis with vertigo could be attributable to otomycosis. It was assumed that the systemic antifungal agents were essential for the symptomatic relief in this situation.
The author declares no conflict of interest.
None.
None.

©2021 Han, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.