MOJ
eISSN: 2381-179X


Case Report Volume 11 Issue 5
1Seth GS medical college & KEM Hospital, India
2Pacific Institute of Medical Sciences, India
Correspondence: Rajaram Sharma, Assistant professor, Radiodiagnosis, Pacific Institute of Medical Sciences (PIMS), India
Received: September 10, 2021 | Published: October 11, 2021
Citation: Patil S, Sharma R, Thakkar H, et al. Twin reversed arterial perfusion (TRAP) sequence in a monochorionic triplet pregnancy. MOJ Clin Med Case Rep. 2021;11(5):142-144. DOI: 10.15406/mojcr.2021.11.00401
Twin reversed arterial perfusion syndrome is the most severe form of complication of a monozygotic twin pregnancy. Although not fully understood, the accepted theory of aetiology is an abnormal vascular connection between the vessels of the twins inside the placenta. The donor twin is a normally developed twin, also known as pumping twin, which supplies the blood supply to the mal developed twin. The mal developed twin is a mass of unorganised tissue; however, sometimes, little morphological differentiation can be observed. As the pumping twin has the supply of blood to the mal developed twin also, the risk of cardiac failure runs high in the pumping twin. As a result, most of these pregnancies result in an adverse outcome. Due to advancements in imaging and treatment, these cases are salvageable now, provided these are detected earlier. We are presenting a previously unreported case of triplet pregnancy with one normal fetus and two fetuses with TRAP physiology.
Keywords ultrasound, twin pregnancy, twin reversed arterial perfusion
TRAP, twin reversed arterial perfusion ; USG, ultrasound
The incidence of the TRAP sequence is estimated as 1% of monozygotic twins, affecting 1/35,000 to 1/50,000 births.1 Most of the cases of TRAP sequence are seen in twins, with only 8% in triplets. The risk increases with multiple pregnancies of higher order.2 Twin reversed arterial perfusion (TRAP sequence) represents a syndrome characterized by partial or complete lack of cardiac development in one of the twins and abnormal vascular communication in the placenta.3 In our case, we had monochorionic triplets with TRAP physiology, which is very rare (Figure 1).
37-year-old multi-gravida came in OPD for her first ANC scan. She was having a Triplet pregnancy with a single anterior placenta.
Two amniotic sacs were clearly visualized.
Left amniotic sac: Fetus-A with absent calvarium and mildly organized brain tissue above orbits (probably suggestive of exencephaly).Abdominal Circumference – 12 cm, corresponding to 18 wks.
Right amniotic sac: 2 fetuses ( B, C ), no intervening membrane was clearly visualized.
Fetus B: No anomaly was visualized. -BPD, FL corresponding to 18 wks.
Fetus C: The thoracic and abdominal parts of the tissue were crudely developed and the lower extremity appeared fused.
-This tissue measured – 6.6.x3.4x4.5cm i.e. 53cc.
-No heart, skull or upper extremity was visualized.
-Single Umbilical artery was seen entering the abdomen with the rate 156 of bpm.
No other complications were present in the mother.
The patient was advised selective fetal reduction as there were higher chances of failure of pregnancy. However, the patient refused, and unfortunately, preterm delivery happened at 28 weeks. All three fetuses were expelled and were not viable. No post-partum complication to mother, and she is healthy as of now.
In the TRAP sequence associated with twins, the normal twin ‘pumps’ blood to the abnormal twin, called the ‘recipient’ twin, through abnormal artery-to-artery and venous-to-venous communications in the placenta. This is in conjunction with the vascular anastomosis, which takes place in TRAP syndrome.4 (Figure 2 - Figure 7).
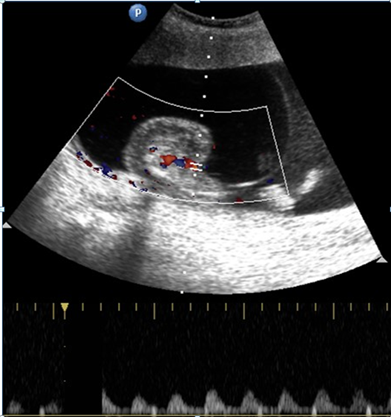
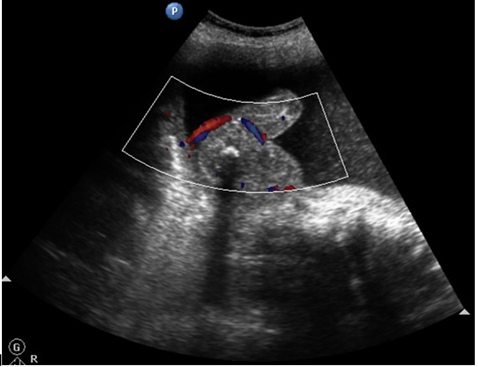
Figure 2,3 Trans-abdominal USG shows an abnormal fetus with grossly formed lower torso and lower limbs without any discernible visceral organs and an echogenic structure casting a distal acoustic shadow, probably representing the spine of the abnormal fetus (white arrow).
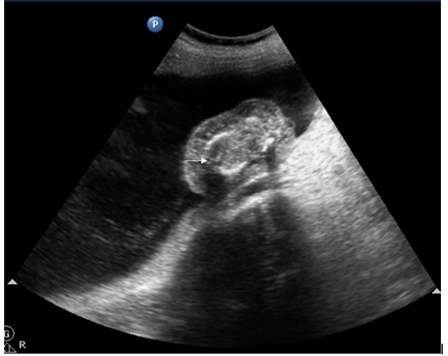
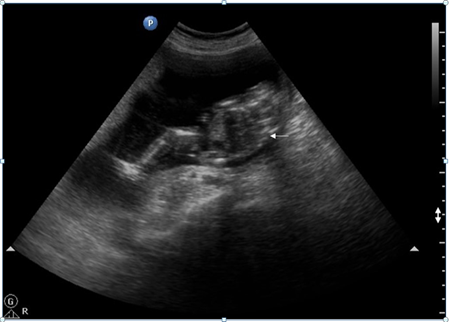
Figure 4,5 Pulsed Doppler of the umbilical artery of the abnormal fetus shows reversal of flow on the spectral waveform.
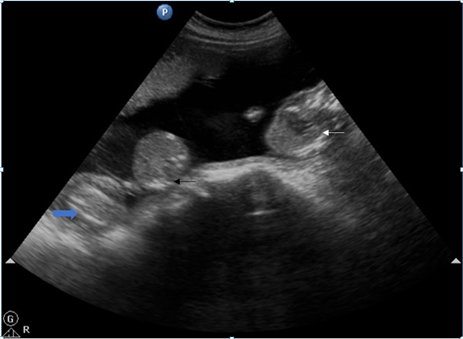
Figure 6 Trans-abdominal USG shows abnormal acardiac fetus with normal pumping twin and part of umbilical cords of both twins separately.

Figure 7 Post-delivery image of exencephaly fetus (white arrow), abnormal a cardiac mass (black arrow) and normal pumping fetus from left to right (blue arrow). All three umbilical cords are separately visualized (star).
Video Trans-abdominal ultrasound showing intrauterine monochorionic diamniotic gestation with single anterior wall placenta. Normal pumping twin (white arrow) and abnormal a cardiac mass (black arrow) in the amniotic cavity on the right side and fetus with exencephaly in the amniotic cavity on the left with intervening amniotic membrane (red arrow).
In one case report, there is an association of TRAP with Vertebral anomalies, Anal atresia, Cardiac defects, Tracheo-esophageal fistula and/or Esophageal atresia, Renal & Radial anomalies and Limb defects (VACTERL) which indicates a defect in early embryogenesis.5
Congenital anomalies are present in about 9% of pump twins. The overall perinatal mortality of pump twins is 50-55%. This is generally due to either polyhydramnios leading to premature delivery or secondary to congestive cardiac failure developing due to the increased cardiac output secondary to the abnormal inter-fetal circulation. 4,6
Prenatal diagnosis by ultrasound is suspected when there is discordance, and bizarre malformations suspected in a twin gestation presents with retrograde blood flow in acardiac twin demonstrated by pulsed/colour flow Doppler.7,8
Prenatal treatment involves occlusion of blood flow to the acardiac twin by endoscopic (fetoscopic) ligation or laser coagulation of the umbilical cord, bipolar cord cauterization, or intrafetal radiofrequency ablation.9
In the case of multiple gestations with TRAP physiology, earlier diagnosis is required as complication rate in the normal fetus increases with advancing gestational age, and fetal intervention for selective fetal reduction like laser coagulation can be performed.
None.
None.

©2021 Patil, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.