MOJ
eISSN: 2381-179X


Case Report Volume 5 Issue 1
1Department of Oral and Maxillofacial Surgery, DAPMRV Dental College and Hospital, India
2Department of Oral Medicine and Radiology, Saraswati Dhanwantari Dental College and Hospital, India
Correspondence: Abhishek Singh Nayyar, Department of Oral Medicine and Radiology, Saraswati Dhanwantari Dental College and Hospital and Post-Graduate Research Institute, Maharashtra, India, Tel 91-7350990780
Received: October 27, 2016 | Published: November 11, 2016
Citation: Rao SG, Mehta S, Nayyar AS. Swing mandibulotomy access to deep lobe parotid tumors case reviews. MOJ Clin Med Case Rep. 2016;5(1):183-188. DOI: 10.15406/mojcr.2016.05.00123
Introduction: To utilize Swing mandibulotomy approach for gaining access to the deep lobe parotid tumors and to evaluate the functional and esthetic results.
Case series: In the present case series, two patients were selected on standard criterion based on histological type, site, age, sex, clinical features, radiological evaluation, recurrence of the parotid tumors and surgical access to these tumors. Patients selected on eligibility criteria were evaluated and underwent, further, radiological evaluation and were surgically managed. Thereafter, long term follow-up was done clinically as well as radiologically. Successful surgical outcome was determined on the basis of functional and clinical recovery.
Conclusion: Selecting the best approach to maximize visibility, ensure complete removal of the tumor and to reduce morbidity is an important decision to be made. Mandibulotomy provides an excellent mandible sparing surgical approach to gain access to deep lobe parotid tumors which are otherwise not accessible without procedures which leave significant morbidity.
Keywords: adenoma pleomorphic, parotid tumors, swing mandibulotomy
Pleomorphic adenoma is the most common salivary gland tumor.1 Most of these tumors originate in the superficial lobe with few involving the deeper lobe with medial extensions in to the adjacent parapharyngeal space (PPS).2 These tumors are generally considered to be benign even if the lesion presents with varied histological features due to different components with myxoid or, chondroid components. The main characteristics include its high recurrence rate and not infrequent malignant transformation. Most cases present as asymptomatic swellings without involving the facial nerve until there is substantial growth and impingement of the facial nerve. Often, onset of a facial nerve deficit, changes in consistency, rapid growth, and pain are the signs for the malignant transformation of the lesion. The histological variation of the tumor along with its particular location poses difficulty in its accessibility for adequate removal of the tumor. Because of the difficulty involved in getting into the parapharyngeal space (PPS), different approaches have been described including the transcervical, the first approach, described by Morfit HM,3 transcervical-transparotid, the most widely used, helpful in PPS tumors originating in the parotid deep lobe, transpalatal or, transoral, described by Ehrlich H2 and limited to small non-vascular tumors, transmandibular with mandibular osteotomy being described as a complement to the other approaches in order to improve and increase access to the parapharyngeal space (PPS), Ariel et al.,4 were the first to propose opening the jaw to enter the PPS with numerous variations in the procedure being described later,5,6 and lastly, the orbito-zygomatic approach to the middle cranial fossa described by Fisch U7 to give access to PPS tumors affecting the temporal bone or, relatively larger tumors reaching the base of skull. Thus, it becomes of utmost significance to select the right surgical approach for such kind of cases balancing maximum exposition and complete and safe removal of the tumor with minimal functional and esthetic morbidity.
Case report 1
A 59-year-old male presented to the unit complaining of a gradually increasing, painless swelling in the right parotid region since 4months. The swelling was associated with dysphagia and dysphonia. Patient gave history of pleomorphic adenoma of right parotid 15years back following which he underwent superficial parotidectomy. Pleomorphic adenoma was diagnosed by Fine needle aspiration cytology (FNAC) technique. MR imaging revealed a dense extensive, homogeneous mass, 5cms in diameter, originating in the right deep parotid lobe and extensively involving the parapharyngeal space (PPS), base of skull and infra-temporal fossa pushing the soft palate to one side. Patient was admitted for definitive surgical management. He underwent excision of the lesion via paramedian mandibular osteotomy for access to the lateral pharyngeal space, base of skull and infratemporal fossa to completely remove the tumor while preserving the facial nerve. Post-operatively, the patient recovered uneventfully with no facial or inferior alveolar nerve deficits and no osteotomy related complications resuming normal mandibular movements (Figures 1-3).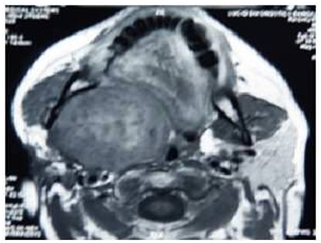
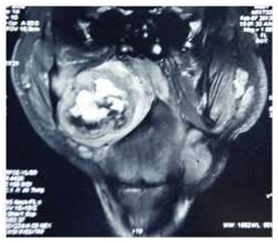
Figure 1 (A,B) - Pre-operative MRI scan depicting a dense extensive homogeneous mass, 5cms in diameter, originating in the right deep parotid lobe and extensively involving the parapharyngeal space, base of skull and infra-temporal fossa pushing the soft palate (Case 1).
Case report 2
A 63-year old female reported to the unit with a gradually increasing, painless swelling on the left side of neck from past 4months. Patient did not have any signs and symptoms of dysphagia and dysphonia. Patient gave a history of superficial parotidectomy of left parotid gland 23years back along with radiotherapy. On examination, a well-defined, 2cms lesion was found in post-auricular region which was fixed, non-tender, and firm in consistency. Another well-defined lesion of 2cms dimension was present in the left submandibular region near angle of the mandible. Fine needle aspiration cytology (FNAC) was suggestive of pleomorphic adenoma of deep lobe of parotid. MR imaging revealed a well-defined, large lobulated mass, extending from the left ramus of mandible with extension into the parapharyngeal space (PPS) medially and another oval mass in left retro-auricular region superficial to sternocleidomastoid muscle with another lesion in the pre-auricular region. Patient underwent surgical excision with paramedian mandibular osteotomy to access the tumor of the deep lobe. She withstood the procedure well with no residual functional or esthetic deficits (Figures 4-6).
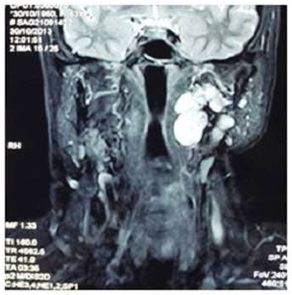
Figure 4 (A, B) - Pre-operative MRI scan revealing well-defined large lobulated mass from left ramus of mandible with parapharyngeal space extension. (Case 2)
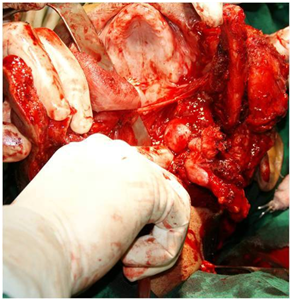


Figure 5 (A, B, C) - Enucleation and excision of the entire mass in-toto with swing mandibulotomy with the mandible dislocated superiorly; fixation of the mandibular segments was carried-out with mini plates and screws. (Case 2)
Technique of mandibular swing approach and excision of tumor: Under naso-tracheal intubation, routine skin preparation and draping, the operation began with a pre-auricular incision which was carried-out anteriorly into the submandibular region reaching the mandibular symphysis. The trunk of the facial nerve was identified by using the insertion of the posterior belly of the digastric muscle on the mastoid process as a landmark and detaching the parotid lobe from the external auditory canal to identify the tragal pointer. The submandibular skin flap was dissected in subplatysmal plane in the direction of the mandible and paying close attention to the preservation of the marginal mandibular branch of the facial nerve. Next, the periosteum was slit along the inferior mandibular border and in the premolar region, a subperiosteal dissection was done to allow a mandibular osteotomy to be made just anterior to the mental foramen preferably within the interproximal space between the canine and the first premolar. Titanium bone plates were fitted and screw holes were drilled before starting the osteotomy procedure to facilitate approximation of the mandibular fragments at the end of the procedure. The osteotomy was, then, started and the medial aspect of the mandible was freed up to the lingula region where the neurovascular bundle was isolated and preserved. This allowed lateral and superior dislocation of the body and ramus of the mandible exposing the parapharyngeal tumor which was, then, easily mobilized and delivered. At this point, there was a wide exposure from below, laterally and anteriorly which helped to control areas of the tumor that might involve local structures such as the internal carotid artery, eustachian tube and the base of the skull. Tumor size and possible extensions were, also, assessed by finger dissection. Involvement of the mucosa is rare with neoplasms of the parotid parenchyma and hence, the mass was thoroughly enucleated from the adjacent connective tissue. Once the tumor was delivered, the osteotomized mandibular segments were re-approximated and stabilized with the adapted bone plates after ensuring the position of the condyle in the glenoid fossa. Hemostasis was achieved using bipolar cautery and incisions were re-constructed layer by layer and a suction drain was placed. Post-operative management included a short course of a broad-spectrum antibiotic which was prolonged in one of the patients wherein the integrity of the mucosa was compromised.
Pleomorphic adenomas are slow growing, well-demarcated tumors constituting around 80% of benign parotid tumors.1,2 The mainstay of parotid surgical procedures involves the cleavage of the gland along the two planes divided by the facial nerve.3 Around 90% of the parotid tumors arise in the superficial lobe while approximately, 80-85% of the glandular tissue lies lateral to the facial nerve.1,4,5 Approximately 10-12% of the parotid tumors arise from the deep lobe with only a small proportion (~1%) with a tendency to extend medially towards the parapharyngeal space (PPS).1,5,6 The complex anatomic relations of the deep lobe with adjacent structures often makes tumors involving this lobe and peripheral areas a definite surgical challenge for adequate approach.7,8 Although recurrent parotid pleomorphic adenomas have been the subject of much attention in the clinical literature, especially, pertaining to managerial issues, there is a relative paucity of information defining the imaging characteristics of these lesions in the radiologic literature.9–12 Multiplicity of lesions has been described as a reliable indicator of recurrence in the parotidectomy bed of patients with prior pleomorphic adenoma resections.10 Imaging is used to predict the origin, exact location and the size of parapharyngeal tumors. MRI with gadolinium enhancement is considered better than CT scans and is the examination of choice. It can reliably distinguish a deep lobe parotid tumor from a primary parapharyngeal tumor of neurovascular origin or, of extra-parotid minor salivary glands, from evidence, in T2-weighted slices, of the fatty layer between the tumor and the pharyngeal wall. USG- or, CT-guided Fine needle aspiration cytology (FNAC) is usually performed to determine the nature of the mass. According to data in the literature, FNAC is accurate in 90-95% of cases. It is performed transorally, transcervically or, guided by USG or, CT and predicts the nature of the lesion which assists surgeon-patient planning. Management recommendations for recurrent tumors include observation, local or, extensive surgery, radiation therapy, or, a combination of these.9,13–16 Recurrences are often extensive and multifocal making the risk of facial nerve damage and chances of re-recurrence high.8,13,17 Malignant transformation to carcinoma is a well-known entity and the literature reports a rate of between 1.4% and 6.3% in the larger series of patients.18 The risk of malignant transformation seems to be higher in patients older than 40years of age, men, and patients with solitary nodules over 2cms in diameter.8 The risk of malignancy has, also, been linked to the frequency of recurrence.14,19 An accurate diagnosis is essential for planning the best surgical approach to safely and radically remove PPS tumors Papadogeorgakis et al.,20 considered five main parameters in selecting the best approach in treating tumors of the PPS including the proximity and the projection of the tumor to the oropharyngeal wall or, the neck, the size of the tumor, the suspicion of malignancy, the vascularity and relation of the tumor to the neck neurovascular bundle. Different surgical techniques and mandibular osteotomy designs have been described to improve surgical access for the removal of parapharyngeal space (PPS) tumors since Roux’s first description of division of the lower lip and mandible in 1829.9 In 1929, Trotter,15 reported a median translingual pharyngotomy in which he extended Roux's midline section of the mandible by splitting the tongue through the midline for exposure of the base of the tongue and the mid portion of the pharynx. In 1984, Attia et al.,21 introduced the double mandibular osteotomy technique to significantly improve access to the parapharyngeal space (PPS), while still protecting the inferior alveolar and lingual neurovascular bundles. Approaches described by Attia & Biedlingmaier et al.21,22 involve splitting of the lip with attendant esthetic consequences. Approaches involving lateral neck dissection are indicated for large, diffuse tumors, but full surgical exposure is impeded by the presence of the mandible. Such a problem can be overcome by involving mandibular osteotomies. Simple mandibular distraction was proposed by Martin HE.23 It sometimes entails resecting the styloid process and the stylomandibular ligament24,25 or, the posterior margin of the ramus of the mandible3. This approach makes isolation of the superior portion of large neoplastic growths particularly difficult. It, also, increases the intra-operative risks of rupturing the tumor capsule and of injury to the larger vessels. Mandibulotomy, however, allows wider and safer access to the parapharyngeal space, with better control for adequate tumor excision. Various techniques involving osteotomy of the ramus,26–30 the angle or the body of the mandible have been described. All, however, involve resection of the inferior alveolar nerve within the bone except paramedian mandibulotomy. To avoid sacrificing the mandibular neurovascular bundle, Pogrel et al.,27 proposed a horizontal osteotomy of the ramus performed just above the lingula region. The inferior mandibular fragment can, then, be distracted downwards and a few centimeters of access space can, thus, be gained. Flood & Hislop’s’1 inverted-L osteotomy, which does preserve the inferior alveolar nerve, only partially improves on the intra-operative visibility as provided by Pogrel et al.,27 technique. Increasing surgical exposure (while preserving mandibular nerve function) through a superficial parotid lobectomy followed by a mandibulotomy incision anterior to the mental foramen to access the parapharyngeal space (PPS) has been proposed by Attia et al.21 Spiroet al.,10 describe an approach which provides adequate control both of the neoplasm and of the cervical vessels but compromises esthetic outcome because these authors deem a labiotomy to be necessary.
Biedlingmaier et al.,22 stated that it is needed to allow full outward rotation of the mandibular body. Seward GR5 used approach consisting of a parasymphysis mandibulotomy, anterior to the mental foramen, with no cheilotomy or, opening of the floor of the mouth, and preserving the inferior alveolar nerve. Another possible variant is osteotomy at the level of the condyle or, more recently described, vertical osteotomy of the mandible to facilitate greater mobilization of the corresponding segment of the mandible. He also described the possibility of approaching the parapharyngeal space (PPS) through a lateral neck dissection and a mandibulotomy anterior to the mental nerve without labiotomy (the technique which we had chosen). Seward’s approach provides a two-fold advantage over other techniques including an adequate field exposure from below, laterally, and anteriorly for radical tumor surgery, and an alternative osteotomy without labiotomy and sacrifice of the inferior alveolar nerve. In planning the surgical treatment of a benign neoplasm, these esthetic as well as functional considerations, should be foremost. The fitting of bone plates before making the mandibular osteotomy limits the need of maxillo-mandibular fixation to a few days of elastic guidance of the occlusion. This access allows the parapharyngeal space (PPS) to be reached with relative ease, and provides excellent visibility with wide surgical exposure to secure local neurovascular structures and thereby, preserves both sensory and motor functions, without appreciable esthetic compromise. The median labiomandibulotomy was popularized by Martin et al.16 Since the first osteotomies were described by Ariel et al.,4 several variants31 have been described. McGregor et al.,17 described modifications of the osteotomy with the use of power saws and dental drills to avoid dental extractions. Mandibulotomy can be performed anterior to mental foramen-medial mandibulotomy or, posterior to mental foramen-lateral mandibulotomy. Lateral mandibulotomy is, nowadays, seldom used because the combination of radiation effect and loss of blood supply by dividing the inferior alveolar artery may result in the non-union or, osteoradionecrosis of the mandible.18 Median mandibulotomy can be, further, classified into midline (median) mandibulotomy, between the two central incisors and para-midline (para-median) mandibulotomy, between the lateral incisor and canine.19 In a classical midline (median) mandibulotomy with a mandibular swing approach, the genioglossus, geniohyoid and mylohyoid muscles have to be transected,10 however, in a para-midline (paramedian) mandibulotomy with lateral mandibular swing, the centrally located genioglossus and geniohyoid muscles can be preserved.11 According to Dubner Sanford et al.,32 median mandibulotomy (mandibular "swing") supplanted mandibular resection for access to oral and oropharyngeal tumors when there is intervening grossly normal tissue between the tumor and the bone. It has, also, proved useful for exposure in selected patients with deep lobe parotid or, parapharyngeal space (PPS) tumors. The authors had reviewed 313 mandibulotomies performed between 1959 and 1988 with emphasis on indications, complications, and modifications in technique. In a comparative study between these two types, Tsung et al.,14 did not find any differences that were statistically significant. Amin et al.,12 however, concluded straight midline osteotomy to be advantageous with no significant complications seen within 1-year follow-up. The midline, stair-step osteotomy was designed to provide better stability to the osteotomy site.33 Yiwen et al.,34 resected 5 pharyngeal and parapharyngeal space (PPS) tumors and showed that mandibular swing approach is an optimal technique for thoroughly removing retromandibular tumors of the parotid gland. The excisions did not injure the facial nerve nor led to any significant complications. In all the 5 cases, tumors were located in the parapharyngeal space (PPS) while in one of the cases, the tumor protruded into the palate. During their 5-year analysis, Jungehuelsing et al.,35 evaluated 9 patients with extensive, deep lobe, benign, parotid gland tumors, who underwent lateral parotidectomy followed by a modified mandibular swing procedure without lip split. In all the patients, adequate exposure was obtained for total resection of the parapharyngeal space (PPS) lesions with mandibular swing technique. Hye-Young et al.,13 reviewed retrospectively, 30 patients who had a uniform surgical technique consisting of a lower lip-splitting, modified stair-step osteotomy with at least 14months post-operative follow up during a 5-year period. According to them, an ideal mandibulotomy technique required no intermaxillary fixation (IMF), preserved the occlusion in a precise way, enabled early function, entailed no secondary procedures, and was free of complications.36 The main problem with the original mandibulotomy technique concerned the post-operative fragment mobility due to a bony gap on the osteotomy line. In spite of rigid flxation, the bony gap remains, and mobility of unstable fragments increases the probability of post-operative complications such as malocclusion, non-union, and osteoradionecrosis following post-operative irradiation. Mandibulotomy is an important surgical approach for tumors in the oral cavity, oropharynx, parapharyngeal space, nasopharynx and skull base.14 Based on these factors, mandibular swing approach has been considered to be an ideal technique to approach tumors in the pharyngeal and parapharyngeal space (PPS) region avoiding blind and unnecessary injuries (Han, et al. 2002 and Sun, et al. 2006). Although, the significant concerns regarding the mandibular swing approach include incomplete concrescence of mandible, inarticulacy, deglutition obstacles, middle ear effusion and bleeding, and cranial nerve palsy (Wang, et al, 1998). Abdel-Haleem et al.,8 has reported 11 patients diagnosed to have parapharyngeal space (PPS) occupying lesions that were subjected to surgical excision by the transmandibular approach. In 2007 and 2009, Kolokythas et al.,37 reported the use of a double mandibular osteotomy without lip split to remove tumors of the parapharyngeal space (PPS). Double mandibular osteotomy facilitates the resection of even large and malignant neoplasms of the parapharyngeal space (PPS) but the double osteotomy seems to create stability problems of the mandible and thus, post-operative occlusal derangement which has to be treated later, then, by lingual splints and arch bars. When considering a mandibular osteotomy procedure, complete removal of the tumor, maintenance of occlusion with acceptable temporomandibular joint function, and functional preservation of facial and inferior alveolar nerves are the major considerations to be kept in mind. perform a mandibulotomy is made once the transcervical or, transcervical-transparotid approach to the parapharyngeal space (PPS) is performed and access for total tumor removal assessed. If the tumor can be removed with the transcervical or, transcervical-transparotid approach, then, a mandibulotomy is not performed. If the tumor cannot be adequately exposed via the transcervical or, transcervical-transparotid approach because of the involvement of the pre-styloid compartment of the parapharyngeal space (PPS) such as with tumors that originate in the deep lobe of the parotid or, parapharyngeal space (PPS), or, ectopic salivary gland tissue, a single, anterior, symphyseal osteotomy is sufficient for parapharyngeal space (PPS) access and tumor exposure. Removal of a mandibular incisor to allow for an anterior mandibular osteotomy is, also, recommended. A midline mandibular osteotomy has been described with a lip and soft tissue incision across the midline to provide access for exposure and placement of the rigid fixation. This is unnecessary for the mandibular swing technique. It is sufficient to expose the mandible, as described above, and not to perform lip and soft tissue split. The mandibular processes turn around an imaginary axis through the symphysis and mandible articulation has enough latitude to allow wide lateral deflection. Multiple techniques and combinations of osteotomies have been employed to facilitate access to the parapharyngeal space (PPS).38 In the present cases, the use of a single midline mandibular osteotomy technique was employed for exposure of deep lobe parotid gland tumors allowing mandibular swing and improved access to the parapharyngeal space (PPS).
We have illustrated the surgical technique and reviewed our experience with 2 patients treated from 2013 through 2014. While employing mandibular osteotomy for access to resect a deep lobe parotid or, parapharyngeal space (PPS) tumors, the important goals considered should include preservation of facial nerve function, complete removal of the tumor without rupture, maintenance of the pre-operative occlusion, functional temporomandibular joint movement, and preservation of the inferior alveolar nerve sensation. Median mandibulotomy (mandibular "swing") has supplanted mandibular resection for access to oral and oropharyngeal tumors when there is intervening grossly normal tissue between the tumor and the underlying bone. It has, also, proved useful for exposure in selected patients with deep lobe parotid or, parapharyngeal space (PPS) tumors. Mandibulotomy technique provides excellent access up to the base of skull with no significant morbidities. Long term follow-up of patients with pleomorphic adenoma, even confined to superficial lobe, plays a very important role as it has a high chance to recur in the deep lobe, even after 15-20years, requiring follow-up for the lifetime.
None.
The author declares no conflict of interest.

©2016 Rao, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.