MOJ
eISSN: 2381-179X


Case Report Volume 8 Issue 5
1 Department of Medical Education, Hamad Medical Corporation, Qatar
2Department of Radiology, Hamad Medical Corporation, Qatar
3Department of Medicine, Hamad Medical Corporation, Qatar
44 Department of Hematology/Oncology, National Center for Cancer Care & Research (NCCCR), Hamad Medical Corporation, Qatar
Correspondence: Mohamed A Yassin, Department of Hematology/Oncology, National Center for Cancer Care & Research (NCCCR), Hamad Medical Corporation, Doha, Qatar
Received: June 01, 2018 | Published: October 2, 2018
Citation: Ibrahim M, Awad A, Elnefati N, et al. Splenic tuberculosis in an immunocompetent patient: a case report. MOJ Clin Med Case Rep. 2018;8(5):195-197. DOI: 10.15406/mojcr.2018.08.00276
A 28-year-old male previously healthy presented with fever and abdominal pain for one month, associated with weight loss of 6kgs.Abdominal imaging revealed multiple hypoechoic lesions and CT chest showed multiple cervical and mediastinal lymphnodes. Sputum culture, PPD, blood cultures and quantiferon all were negative. Splenic biopsy was Consistent with necrotizing granulomatous inflammation. Here we present extraordinary case of splenic TB to shed the light on such important diagnosis even in Immunocompetent Patient.
Keywords: spleen, tuberculosis, splenic tuberculosis, immunodeficiency
Tuberculosis (TB) being ranked as one of the top infectious causes of mortality globally, causing ill-health for around 10million people per year, and recently it surpassed HIV as being ranked as the number one single infectious cause of death worldwide.1,2
Isolated Splenic TB is not commonly seen in immunocompetent patients,3 and usually a risk factor from the following is found: immunosuppression, preceding pyogenic infections, splenic abnormalities, prior trauma to the spleen, sickle cell disease and other hemopathies, and in the immunocompetent patient another body site infected by M. tuberculosis.4 In this case we present a young immunocompetent male with no past medical history, with splenic TB.
A 28-year-old male, not known to have any medical illnesses presented with chief complaint of fever and abdominal pain for 30days. Fever was occurring almost every day but mainly at night, which was associated with sweating, chills and rigors.
Along with the fever he complained of left hypochondrial pain for one month, mild to moderate in severity, non-radiating and it wasn’t associated with nausea, vomiting, loss of appetite or change in his bowel habits. But he reported weight loss of 6kg during this 25days and loss of appetite. His investigations showed WBC count of 13.4 ×10^3/UL, hemoglobin of 13.5gm/dl.CRP was 98mg/l (normal <5), blood cultures 2sets were negative, Sputum cultures and Acid fast bacilli stain were negative as well as quantiferon test, purified protein derivative(PPD) also was negative.HIV and Brucella workup both came back negative.CXR showed no abnormalities noted in the lungs, pleura, hila and mediastinum. The heart appears normal in size. Transthoracic Echocardiography didn’t find any vegetation or abnormality.
Ultrasound abdomen showed no obvious free fluid or sizable collection to the visualized extent, multiple heterogeneous (predominantly hypoechoic) lesions in the spleen, the largest measuring 19x9mm.
Later CT abdomen done showed multiple hypodense lesions of varying sizes are noted in the spleen; some of the lesions appear ill-defined and conglomerate. Multiple sub centimeter and borderline/mildly enlarged retroperitoneal lymph nodes were noted (Figure 1).
CT chest showed multiple lower cervical subcentimetric lymph nodes noted. Multiple mediastinum subcentimetric lymph nodes the largest measures 6.5mm in short axis in preaortic group. Multiple bilateral subcentimetric axillary lymph node with preserved fatty hilum.
Further imaging by MRI Abdomen showed Bulky spleen demonstrating lobulated and nodular outline with multiple intra parenchymal focal lesions of variable size and many of them appears conglomerate and ill-defined identified throughout the spleen. These lesions are predominantly hypointense in T1 and T2-WI with faint areas of high T2 signal and heterogeneous enhancement. Multiple subcentimetric and/or borderline size lymph nodes are identified at the left para-aortic region, portahepatis, posterior to the gastric fundus and left anterior supradiaphragmatic region the largest measuring 10 mm in short axis (left para-aortic) at SMA level (Figure 2).
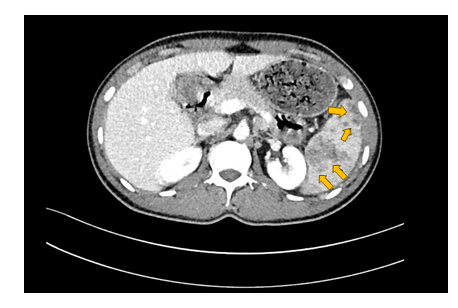
Figure 1 Contrast enhanced CT scan of the abdomen acquired in the Porto-venous phase showing multiple irregular ill-defined hypodense splenic lesions of varying sizes.


Figure 2 Axial T2 and multi-planer contrast enhanced T1 Fat suppressed images of the abdomen showing a bulky spleen demonstrating a lobulated outline with multiple conglomerated intra parenchymal focal lesions of variable sizes showing predominantly hypo-intense signal on T1 and T2-WI with faint areas of heterogeneous enhancement.
Decision was made to go for splenic biopsy, which was Consistent with necrotizing granulomatous inflammation associated with mixed acute and chronic inflammation. No definite organism’s identified and no definite evidence of malignancy in the biopsy. After reviewing the histopathology results patient was started on Anti-TB treatment with Rifampicin, Isoniazide, Ethanbutol and Pyrizinamide along with pyrodixine. After which he achieved complete remission.
Tuberculosis (TB) is a critical infectious disease that primarily affects the lungs through the introduction of Mycobacterium tuberculosis. Usually this occurs when a person with active TB exhales the bacterium engulfed on tiny air droplets. 5 With 10million mortality per year, TB has been ranked as among the top most infectious causes of death. It currently ranks above HIV as most infectious disease with the largest mortality rates across the globe.1,5
Pulmonary TB (PTB) has been described as TB of the lungs. On the other hand, extra-pulmonary TB (EPTB) has been known to affect other organs different from the lungs such as the spleen as is the case with the 28-year-old, lymph nodes, joints, skin, bones and other body organs.2,5 The bacterium Mycobacterium tuberculosis has as well been established as a viable risk factor capable of resulting in EPTB .The multiple heterogeneous (hypoechoic) lesions in the spleen (largest 19x9mm) indicate that this was a case of EPTB with the organ of under attack being the spleen and not PTB. A study by Sunnetcioglu and his colleagues endeavoured to establish clinical differences between PTB and EPTB.6 The study utilized a sample size of 411 patients (221men and 190women). 208 (50.6%) reported having PTB while the remaining 203 (49.4%) registered EPTB. Further findings showed that PTB was higher in men (59.6%) while EPTB was higher in women (52.2%). Since EPTB was not present in the lungs, it was highly associated with lymph nodes (39.4%), pleura (23.6%), peritoneum (9.9%) and bone (7.4%). With such information available, it becomes possible to design awareness programs that sensitize the people for better prevention methods against the established risk factors such as the bacterium Mycobacterium tuberculosis as is the case with the 28-year-old.
Usually, splenic TB is not easily notable among many of its immunocompetent patients. Nonetheless, the body lies susceptible to attack especially in the presence of risk factors such as immunosuppression, splenic trauma, preceding pyogenic infections, sickle cell disease, splenic abnormalities and other homeopaths.7 In this case of the 28-year -old male patient, the lack of previous cases of TB indicates that the patient is immunocompetent which shows the bacterium Mycobacterium tuberculosis as the most likely cause of the complication. The high acceleration of the disease could be attributed to splenic trauma and attack by pyogenic infections.
A case by Mandal and colleagues (2014); reported a 20-year-old woman was admitted with similar complains of fever only. Abdominal ultrasonography showed splenomegaly with hypoechoic lesions.8 Presence of acid-fast bacilli in the lesion as shown in the CT-aspiration confirmed splenic TB similar to our reported case.
In summary, splenic TB is indeed a rare type of EPTB. Nonetheless, its effects cannot be understated. Risk factors such as Immunosuppression expose the immune system making it weak and vulnerable to attack from external antigens.9 Usually infection by Mycobacterium tuberculosis on a weak immune system makes the body unable to respond and fight.10 Often the body weakens, and health depreciates at a higher rate as evidenced by the loss of 6kgs in 25days in the 28-year-old patient who has no previous records of the illness.
In endemic area with Tuberculosis, Extra pulmonary Tuberculosis should be considered in patients with low immunity and those who are at high risk. Even though EPTB still can present in immunocompetent patients and further imaging and testing is required in order not to miss such cases.
None
No conflicts of interest have been found.

©2018 Ibrahim, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.