MOJ
eISSN: 2381-179X


Case Report Volume 7 Issue 5
1Service de Neurochirurgie Mamadou Gueye, CHNU FANN, Senegal
2Neurosciences I.P. NDIAYE, CHNU FANN, Senegal
3Institut Supérieur des Techniques Médicales de Lubumbashi, Democratic Republic of Congo
4Université de Thiès, Sénégal
Correspondence: Olivier Mukuku Institut Supérieur des Techniques Médicales de Lubumbashi, Democratic Republic of Congo
Received: November 01, 2017 | Published: November 16, 2017
Citation: Thiam AB, Bugeme M, Belarabi L, et al. Spinal abscess revealed by spastic paraplegia in a 15-month-old infant: about an observation. MOJ Clin Med Case Rep. 2017;7(5):293-295. DOI: 10.15406/mojcr.2017.07.00216
The intramedullary abscess is an exceptional localization. It often poses a diagnostic problem. MRI is highly needed, and allows for early diagnosis. The authors report an observation of a 15-month-old infant admitted for motor deficiency of the lower limbs of progressive installation in a febrile context and in whom clinical examination has found spastic paraplegia, kyphosis of the dorsal spine with slight hyper chromic swelling surrounded by a pilosity facing the T3-T4 dermatomes that suggest a dermal sinus. Medullary MRI shows a pseudo-tumor process and a tract that communicates the medullary space to the skin. A neurosurgical procedure was performed and confirmed the existence of the dermal sinus communicating the skin to the medullary space through a cord; as well as an intramedullary abscess which was drained and whose culture isolated Staphylococcus aureus. After surgery and antibiotic therapy, the evolution was satisfactory with a partial recovery of the muscular force.
Keywords: intramedullary abscess, dermal sinus
The intramedullary abscess is a very rare entity. Less than 100 cases have been reported in the literature, the majority of which originate from the pre-antibiotic period.1 Its mode of revelation can be acute or chronic always posing a diagnostic problem. It is most often secondary to a dermal sinus. Medical imaging, particularly MRI, has greatly facilitated the diagnosis. The well-conducted treatment associating surgical drainage and antibiotic therapy adapted to the germ involved are the best guarantors of functional prognosis.2–4 The interest of this observation lies in the neurological consequences of the infectious complications due to the neglected dermal sinuses making the prophylactic neurosurgical treatment urgent.5 The other interest is to present the very specialized management of the consequences of the paraplegia of the infant. We report an observation of a 15-month-old infant admitted for motor deficiency of the lower limbs of progressive installation evolving in a febrile context and in which the clinical examination revealed a spastic paraplegia. Spinal MRI shows a pseudo-tumor process. Neurosurgical surgery was performed and an intramedullary abscess was found and a dermal sinus was present. Pus culture isolated Staphylococcus aureus. Adequate antibiotics were administered and the progression was satisfactory with partial recovery of muscle strength.
It is a 15-month-old infant of Mauritanian nationality, with a history of unprotected neonatal infection, received in our neurological clinic for motor deficiency of the two lower limbs. His psychomotor development was normal. The symptomatology evolved for about 4months, with the occurrence of a fever, irritability and a dorsal kyphosis. In view of these manifestations, the infant was brought to the local health center for treatment, where a non-documented treatment has been instituted for a period of 10days. After 10days of treatment, the patient presented progressively over 20days a motor deficit of the lower limbs preceded by a functional impotence of the lower limbs causing an impossibility of the walking and the seated station, without context of acute retention of urine or constipation. This is what motivated the parents to consult again in another health center in Nouakchott where the patient was hospitalized for 5days and left without improvement of his clinical picture. Finally, he will be referred to the FANN Neurology Clinic in Dakar for specialized care. It should be noted that the parents of the infant had detected a dorsal cutaneous swelling during his neonatal period, but they had thought that it was an innocent lesion that did not need further investigation (of little clinical importance). The clinical examination found a good state of hydration, hyperthermia at 38.5°C. The infant was conscious with good preservation of superior functions. However, he had a spastic paraplegia with a muscular force rated at 0/5 on the two lower limbs, osteo-tendinous reflexes were sharp at the two lower limbs, poly kinetic and diffuse with an epileptoid trepidation of the feet, plantar reflexes were in extension, the neck was supple. On the other hand, tone, muscle strength and osteo-tendinous reflex were normal to the upper limbs. There were no signs of meningeal irritation. At the level of the musculoskeletal system, a kyphosis of the dorsal spine was noted with a slight hyper chromic swelling surrounded by a pilosity with respect to the T3-T4 dermatomes, suggesting a dermal sinus (Figure 1). The rest of the clinical examination was normal. The hypotheses of a compressive or non-compressive myelopathy associated with dysraphia were mentioned. The medullar MRI performed showed an edema of the cervico-dorsal marrow as well as the bulbar junction, with lesional signal abnormality, hypo-intense T1, hyper-intense T2, heterogeneous enhancement, with a small area In a cockade with a hypo-intense center at the height of C6-C7, a part strongly raised facing T1 and a fusi form part of 31x11,8mm just below. A linear fistula was seen, communicating the collected lesion to the skin (Figure 2). The diagnosis of intramedullary abscess was retained. The haematological assessment found a leukocytosis at 19000/mm3 and the sedimentation rate was high. A neurosurgical procedure was performed and confirmed the existence of the dermal sinus, communicating the skin to the medullary space through a cord (Figure 3). Partial Laminectomy was performed with drainage and lavage of the cavity (Figure 4), but also a resection of the sinus. The cytobacteriological examination of pus isolated Staphylococcus aureus. Prior to pus culture, treatment consisted of broad spectrum antibiotic therapy with Ceftriaxone, Metronidazole and Gentamycin. And after the isolation of the germ, the infant was put on Vancomycin and Chloramphenicol. Evolution was satisfactory with partial recovery of muscle strength.
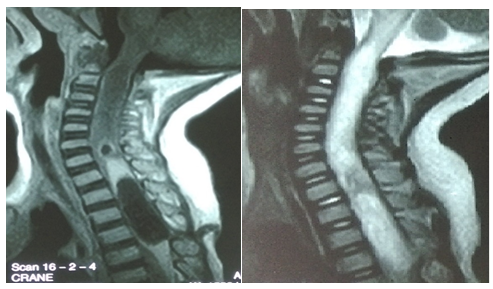
Intramedullary abscess is an extremely rare condition.2,3 It was described for the first time in 1830 and since then only sporadic cases have been reported. Since 1950, its incidence has been estimated at one case per year. The sex ratio is 2.5 in favor of men.6,7 40% of abscesses occur during the first 2years and 27% occur before the age of 10years. The mortality rate is 8-12% and neurological sequelae are found in 70% of patients.9 These abscesses may be unique, multiple or extensive. They may affect all regions but the majority of single abscesses affect the dorsal region.9 There are currently fewer than 100 cases, of which 30% are children.3,8 The medullary abscess may be secondary to direct inoculation after penetrating trauma or by contiguity in case of cutaneous infection on dysraphism.1,3,8 On the other hand, there are medullary abscesses considered as primary for which no infectious focus is found. The congenital dermal sinus is involved as the main cause of intramedullary abscess in children.2,5 It is an infrequent form of closed dysraphism, a pertuis which communicates the skin with the subcutaneous tissues; It can cross the spinal canal and reach the medullary cord. Medullary abscesses are secondary to these sinuses in 20% of cases and the prevalence of these sinuses is 1/2500 births.2,5 As in our case the infection was associated with a dermal sinus. The medullary abscess is considered primary when no causative infectious focus has been found (45% of cases). In order of decreasing frequency, the staphylococcus aureus (23%), streptococcus (17%) and Gram-negative bacilli are the responsible bacteria.4,7,8 Staphylococcus aureus is the germ isolated in our case after the cytobacteriological examination of pus. Diagnosis of intramedullary abscess should be considered in any patient with congenital dermal sinus with symptoms of complete transverse myelitis.2,7 The thoracic spinal column is most often involved. In the case that we present, the dysraphy was located opposite the dermatomes T2-T3. Radiological findings are essential for diagnosis and treatment.2 MRI plays a critical role in the diagnosis of intramedullary abscess. It shows the intramedullary seat of the lesion. In the abscess stage, the marrow appears enlarged, the collection presents a hyposignal T1 and a hypersignal T2. After injection of gadolinium the periphery of the abscess enhances strongly.1,3 Treatment consists of surgical drainage of the abscess with aspiration of the pus and lavage of the cavity after partial laminectomy and myelotomy, combined with a broad spectrum antibiotic therapy, followed by a targeted antibiotic treatment after identification of the germ.3 This was done in our case, and the infant was put under treatment with Ceftriaxone, Metronidazole and Gentamycin and after the isolation of the germ he was treated with Vancomycin in combination with Chloramphenicol.
None.
The authors do not declare any conflict of interest.

©2017 Thiam, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.