MOJ
eISSN: 2381-179X


Case Report Volume 12 Issue 3
1Cirujano oral y maxilofacial, Clínica Universidad de La Sabana, Chía; Cirujano Oral y Maxilofacial, Hospital Central de la Policía; Miembro activo de la Asociación Colombiana de Cirugía Oral y Maxilofacial (ACCOMF) y membership de la AOCMF, Colombia
2Médico y cirujano, Universidad de La Sabana. Clínica Universidad de La Sabana, Colombia
3Médico y cirujano, Universidad Militar Nueva Granada, Colombia
Correspondence: Melanie Alejandra Pérez Orbegozo, Médico y cirujano, Universidad Militar Nueva Granada, Colombia, Tel +573175768238
Received: October 23, 2022 | Published: November 2, 2022
Citation: Serna JAV, Vargas LAN, Martínez LFC, et al. Retrobulbar Hematoma after an open reduction of blow-out fracture of orbit. MOJ Clin Med Case Rep. 2022;12(3):48-51. DOI: 10.15406/mojcr.2022.12.00419
62 years old male patient who presented blunt trauma in his right eye with subsequent orbital fracture type impure blow-out who required open reduction of the facial fracture, who presented at the second postoperative day a retrobulbar hematoma with need for surgical intervention of urgency.
Keywords: orbital fracture, retrobulbar hemorrhage, injuries maxillofacial
Facial trauma has become a health problem with a very high socioeconomic cost and that has been increasing in frequency over the years due to the increase, mainly, in traffic accidents and interpersonal violence.1,2 Facial trauma frequently involves the orbital skeleton and requires timely and appropriate treatment, taking into account the complications and serious secondary sequelae due to poor handling or the trauma itself.2,3 Among the main signs and symptoms of orbital fractures are proptosis, enophthalmos, diplopia and limitation of ocular mobility,4 and although complications are infrequent, within them, tissue injuries can be found. soft surrounding the orbit or lesions that affect structures contained in the orbit or that communicate it with the structures with which it limits such as the cranial cavity, the paranasal sinuses or the nostrils.5
Retrobulbar hematoma is a condition involving deep blood congestion in the soft tissue of the posterior orbital septum, and although it is a rare complication seen in orbital trauma or as a consequence of midface fracture reconstruction surgery, it requires a immediate attention as it can cause irreversible blindness.6 This is why the management of orbital fractures is aimed at restoring the bone fragments early and correctly to avoid a defective repair that could end in the presentation of some functional complication.5 We present the case of a patient with an impure blow-out fracture of the orbit who presented a retrobulbar hematoma as a complication in order to demonstrate the importance of prompt and adequate management to prevent further complications.
A 42-year-old male patient with a medical history of arterial hypertension and chronic kidney disease undergoing renal replacement therapy, who consulted the Clínica Universidad de La Sabana for a one-day clinical picture of facial trauma secondary to an accidental fall from the stairs who presented edema, ecchymosis and chemosis in the right eye at the physical examination. A computerized axial tomography (CAT) of the paranasal sinuses was performed with findings of a fracture of the roof of the right maxillary sinus and of the orbital floor and additionally, right asymmetric exophthalmos (see Figure 1), associated with hematoma, periorbital subcutaneous emphysema and anterior and inferior perimalar. Therefore, an impure blow-out fracture of the right orbital floor was considered, with an indication for open reduction surgery plus emergency reconstruction of the orbital floor. The patient was taken to a surgical procedure where a transconjunctival approach was performed in the right eye; the inferior rectus muscle was released, achieving decompression of the orbit. A mesh was placed, achieving open reduction of the orbital floor with subsequent reconstruction.
However, during the second postoperative day, and after performing a hemodialysis session, the patient presented increased edema, proptosis and hemorrhagic chemosis that exceeded the palpebral margin, limitation for ocular closure, right ophthalmoplegia and decreased vision. visual acuity to the point of not perceiving light, so he was assessed by the ophthalmology service who performed an emergency lateral canthotomy and a new CT scan of the orbits was requested, where a hematoma with dimensions of 1.9 x 2.1 x 3.0 cm, and an approximate volume of 6.2 cm3 (see Figures 2 and 3), persistence of sinking of the right lamina papyracea and no evidence of fracture of the maxillo-malar processes, or zygomatic arches, but a slight angulation was evidenced from the posterolateral wall of the right maxillary antrum; Considering a picture of retrobulbar hematoma in the right eye secondary to an open reduction of the floor of the orbit.
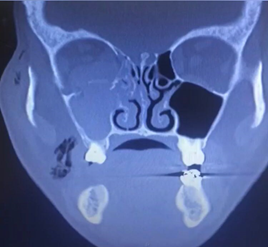
Figure 1 Fracture of the floor of the orbit (black arrowhead), fracture of the medial wall of the orbit (black arrow) and Hemosene (white arrow).

Figure 2 Right retrobulbar hematoma (black arrow). Taken from the radiological images of the patient.

Figure 3 Patient on the second postoperative day. Right proptosis and hemorrhagic chemosis are evidenced.
He was taken to a new surgical procedure where a retrobulbar hematoma was found with displacement of the optic nerve of the right eye and occupation of the right maxillary antrum compatible with hemosenum, for which the retrobulbar hematoma was drained plus bone decortication and bone curettage of the facial bone as an emergency. Through a transconjunctival approach. Using a different route, a right vestibular intraoral incision was made, with a Cadwell luc-type approach to perform drainage and subsequent bone curettage of the facial bone.
A new postoperative control orbit CT scan was requested, where a decrease in proptosis and hematoma volume was found by approximately 80%. The patient was assessed by ophthalmology who found improvement in visual acuity and decreased chemosis, so he was discharged with an adequate clinical and postoperative evolution (see Figures 4,5 and 6).
A bibliographic search was carried out in the global databases PubMed, ProQuest, SciELO and Elsevier, in English and Spanish, in which articles published in the last ten years were selected in research and review categories, using the MeSH and DeCS terms: “orbital fracture”, “retrobulbar hemorrhage”, “maxillofacial trauma”. Articles were reviewed for titles, abstracts, and content, and were ordered by relevance. Next, articles that repeated information and did not provide new or updated information were excluded. Articles that referred to current concepts, risk factors, complications, diagnosis and treatment of retrobulbar hematoma were taken into account.
Facial trauma has become a health problem with a very high socioeconomic cost and that has been increasing in frequency over the years due to the increase, mainly, in traffic accidents and interpersonal violence.1,2 Likewise, it has been shown that this type of trauma occurs with a higher prevalence in males between the ages of 20 and 40.7 In the context of facial trauma, the facial mass is determined by three well-defined areas: the upper, middle, and lower thirds. And in each of these thirds there are bone and soft tissue structures that will determine the severity and possible complications of this type of trauma.8 In the middle third of the face, the orbital fracture is especially important since this type of fracture is very frequently associated with injuries to the surrounding soft tissues and, on other occasions, to the content of the cavity itself.5
The orbit is made up of seven bones that form a pyramid whose main function is to protect the eye and its adjoining structures.9 The bones that are located in the superior and lateral portions of the orbit are stronger, and, conversely, those that are located in the medial portions and in the floor of the orbit are weaker. This is how the force applied to the orbit is dissipated through the eyeball, generating the fracture of the weakest walls.10 Although the eyeball represents only 0.3% of the total surface of the human body, vision loss, whether unilateral or bilateral, has been considered a disability of 24% or 85%, respectively.11
Orbital fractures can be classified in different ways according to the bone compromise they present, however, a special type of orbital fracture is called blow-out or bursting, which are those solutions of continuity of the floor or the medial wall of the orbit that are generated by a mechanism of direct impact on the orbit that causes an increase in intraorbital pressure and a subsequent bone rupture with displacement of its content towards the maxillary or ethmoid sinus, keeping the rim intact12 and in turn, this type of blow-out fracture can be classified as pure when there is a bursting with rotation of the bone fragments of the central portion of the wall and as impure when the injury is associated with a fracture line that extends towards some of the orbital rims. And the latter are frequently related to extra-orbital bone fractures such as malar, maxillary, naso-orbital, naso-orbito-ethmoid and frontal fractures.13
Although orbital fractures are not considered situations that by themselves compromise the life of those who suffer from them, the association with intracranial or ophthalmological injuries that require a timely and effective approach due to their risk of presenting irreversible and even vital functional complications, make their early management is considered an emergency.5 Among the complications and possible consequences that this type of fracture can present is the retrobulbar hematoma, which, although it has a low incidence, requires important care since it can lead to people who present it ending up with visual alterations and even with irreversible blindness due to optic nerve ischemia, retinal necrosis and retinal artery vasospasm due to increased intraocular pressure (IOP).6,14,15
When a retrobulbar hematoma occurs, people may experience ocular symptoms such as circumbulbar pain and pressure, proptosis, eyelid discoloration, mydriasis, visual impairment, and diplopia. Similarly, symptoms of increased IOP such as nausea, vomiting and headache may occur.6,16 The diagnosis of this condition must be made through a computerized axial tomography (CAT) of the orbit or an ocular ultrasound. These types of images also have a very important utility in demonstrating the size of the hematoma.17
The treatment of this condition must be effective and must be carried out in a timely manner once it is suspected and diagnosed, either through the clinic presented by the affected person or through an adequate and effective imaging diagnosis, since it has been found that the delay in the management of the retrobulbar hematoma between one to three hours has shown an increase in the probability of presenting irreversible damage to the retina.18 This is why it has been recommended to follow a logical treatment sequence to ensure a reduction in the risk of complications; Initially, it is recommended that treatment should be immediate, and if surgery is required, the latter should be performed as soon as possible, ensuring the necessary supply of oxygen to maintain saturation above 92%, as well as management with corticosteroids. intravenously, mainly methylprednisolone at a dose of 100 mg and the use of topical beta-blocker medications, since they have shown a necessary decrease in aqueous humor secretion, and acetazolamide at a dose of 500mg intravenously. Finally, within the management of this complication, the use of intravenous mannitol at a dose of 1.5 to 2 g/Kg in 30 minutes has been recommended to reduce the risk of neurological complications.19,20
Retrobulbar hematoma is one of the complications of orbital trauma, which, although it has a very low prevalence, must be diagnosed early to give a appropriate treatment in a timely manner in order to considerably reduce the presentation of both aesthetic and functional complications, mainly irreversible blindness secondary to the initial impact or as a consequence of alterations such as post-traumatic retinal detachment.
The authors declare that no experiments have been performed on humans or animals for this research. The confidentiality of the data was guaranteed. The authors declare that they have followed the protocols of their work center on the publication of patient data. Informed consent was obtained from the patient reported in the case. Institutional ethics committee approval was obtained.
None.
The authors declare that they have no conflict of interest.

©2022 Serna, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.