MOJ
eISSN: 2381-179X


Case Report Volume 8 Issue 2
1Professor of Internal medicine, Cairo University, Egypt
2Lecturer of Internal medicine, Cairo University, Egypt
3Resident of Internal medicine, Cairo University, Egypt
Correspondence: Mervat Essam, Cairo University, Egypt
Received: February 10, 2018 | Published: March 19, 2018
Citation: Menyawi ME, Essam M, Shaker AZ, et al. Protracted febrile myalgia syndrome in patient with familial mediterranean fever. MOJ Clin Med Case Rep. 2018;8(2):41 – 47 DOI: 10.15406/mojcr.2018.08.00237
Familial Mediterranean fever (FMF) is a one of genetically basis auto inflammatory disease characterized by recurrent episodes of fever, serositis & musculoskeletal involvement. Protracted febrile myalgia syndrome (PFMS) is characterized by severe paralyzing myalgia, high fever, abdominal pain, diarrhea, arthritis/arthralgia, and transient vasculitic rashes. We report a 15year-old girl with PFM as non classical presenting symptoms of FMF, and discuss the course of management of this case.
We reviewed the literature and mostly recorded all case reports of PFM affected adolesecent and adult patients over the past years to give special prominence to muscle affection in FMF particularly PFM
Keywords: FMF, protracted febrile myalgia, auto inflammatory, fever
Familial Mediterranean fever is a disease described by paroxysmal and self limiting episodes of fever, serositis & synovitis. Sephardic Jews, Armenians, Turkish, and Arabs are predominantly affected through a recessive autosomal mode of transmission.1
Myalgia is not uncommon musculoskeletal manifestations (occurs in 20%). Protracted febrile myalgia (PFMS), one of muscular pain disorder characterized by severe disabling myalgia, high fever, abdominal pain, diarrhea, arthritis/arthralgia.2
High erythrocyte sedimentation rate (ESR), hyperglobulinemia, normal creatine phosphokinase (CPK), and leukocytosis are the other findings.3 The episodes last for 4–6 weeks, except in those patients need to be treated with corticosteroids. The PFMS may recur even under colchicines prophylaxis. In this article we describe our case, and also collect & summarize all reported cases from searching on the related references and reviews of literature
15 yrs old female patient born and lives in Kafr Elsheikh, Egypt was diagnosed to have typical attacks of FMF 5 years ago on colchicine treatment (1.2 mg/d), Molecular genetic study revealed positive heterozygous state , MEFV gene mutations (M694V , E148Q , P369S). The patient has positive family history (her father and uncle has FMF), During the past 6 months, the patient experienced bilateral diffuse, non exertional crippling muscle ach with swelling of both thighs restricting movement of lower limbs, not relieved by colchicin or NSAIDS, the condition was not associated with fever and colicky abdominal pain or skin rash for which she was admitted in the hospital of the faculty of medicine Alex University where initial examination and investigations were done then the patient sought a medical advice in our department. On systematic physical review: The well-developed patient was bedridden in agony normal blood pressure and temperature. Height=145 cms, weight=40 kgs, BMI=19. There was bilateral symmetrical diffuse& tender swelling of both thighs with subcutaneous edema made her unable to move the lower limbs properly, sensory and motor exam of the upper extremities was normal, Cardiac, chest, abdominal examination was apparently free. Laboratory investigations revealed normal levels of CK, CK-MB, Aldolase & transaminases. Hemoglobin 13.8 g/dL; white blood cell count 5000/mm3, platelet count, 209,000/mm3; ESR was 14mm/h and high C-reactive protein (CRP) (40 Iu/L). Normal liver & kidney function tests. ASOT within normal range (150 U/ml), ANA, ANC, RF & amyloid A were negative virology markers for HCV, HBV& CMV. Chest X-ray, Abdominal ultrasonography, bilateral lower limb arterial and venous duplex & Ultrasound knee joint showed no abnormalities. MRI of both thigh on presentation showed right posterolateral thigh ill defined patchy area of soft tissue edema involving subcutaneous tissue eliciting high signal in STIR & measure about 10 cm, normal MR musculature appearance with intact intermuscular fascial fat planes (Figure 1)(Figure 2).
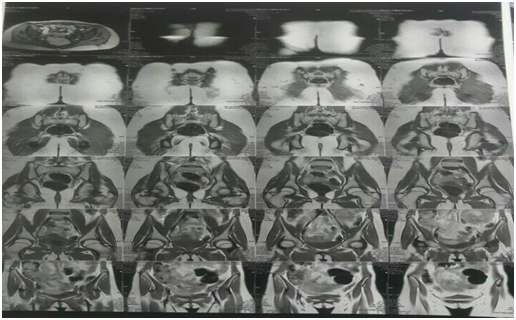
Electromyogram (EMG) and sensorimotor nerve conduction studies of both lower limbs showed evidence of patchy myopathy. After exclusion the presence of vasculitis which mostly associated with FMF and myalgia induced colchicin; we assumed that the patient had porotracted febrile myalgia (PFM), so pridnosolone 0.5 mg/Kg was first prescribed but the patient did not improve then we escalate the dose to 1mg/kg/d with extensive physiotherapy for more than 2 months the clinical condition was ameliorated (the Subcutaneous edema & muscle pain subsided & the patient could independently walk) and follow up labs were improved regarding CRP (4 IU/L). Follow up MRI show no abnormality
Then we started to tapper steroids slowly
Familial Mediterranean fever (FMF) is a genetic disease characterized by painful febrile attacks of serositis and systemic manifestations. Since the disease first described in 1945 and the gene of the disease identified in 1992. Many sets of criteria were described for the diagnosis. The commonest of these is Tel Hashomer’s (Table 1) depending on major and minor criteria.4 The pathogenesis of FMF5 is related to exaggerated inflammatory response secondary to abnormal pyrin that has a critical role in the regulation of IL-1 pathway and mutations result in increased IL-1 production, which is believed to be responsible for the clinical characteristics. During episodes, the chemotactic activity of the granulocytes is greatly increased with a massive influx of granulocytes to the affected tissues.6 Pyrin is expressed only in granulocytes and is likely to be a nuclear factor that controls the inflammatory response in differentiated granulocytes.
Major criteria |
Minor criteria |
|
Incomplete attacks of chest, |
|
Incomplete attacks of joint (joints other than specified in major criteria) |
|
Exertional leg pain and |
|
Favorable response to colchicine. |
|
|
Table 1 Criteria for FMF diagnosis
The gene responsible for FMF, MEFV, was identified in 19927, and nearly 30 mutations have subsequently been detected8 the most common are M694V and V726A. Variable MEFV mutations have different diagnostic, therapeutic, and prognostic implications.9
Streptococci might be assumed to be the incriminating agents due to increased ASO titers, circulating immune complexes, hypergammaglobulinemia, and complement component consumption are detected, in patients10 especially those with vasculitis.11
As presented the most important musculoskeletal symptoms is joint involvement, however muscle pain and tenderness may be featured, It has been reported as 20-25% in patients with FMF and has various forms of including myalgia related to Henoch Schönlein purpura and Polyarteritis nodosa, exertional leg pain, fibromyalgia, constitutional generalized myalgia & finally colchicine induced myopathy.2
Protracted febrile myalgia (PFM) is a rare pattern (1.2%) of myalgia in FMF. However it may be the first presentation of FMF.12 It is characterized by episodes of prolonged incapacitating muscle pain & tenderness3 lasting up to 6 weeks. It is associated by high fever, abdominal pain, diarrhea, arthritis/arthralgia, vasculitic rash, and nephritis. Most of the patients with PFMS bear M694V mutation, However there is a report of PFM case homozygous for E148Q.13 These attacks are not prevented by colchicine and do not respond to non-steroidal anti-inflammatory drugs. Muscle enzymes are within normal limits with elevated erythrocyte sedimentation rate, hyperglobulinemia & leukocytosis.14
MRI can be considerd as a valuable tool to diagnose PFMS, the features that suggest PFMS are diffuse oedema of subcutaneous fat tissue, increased intensity and contrast enhancement of the muscles and increased signal intensity of vascular beds.15 Electromyogram (EMG) may be normal or show nonspecific myopathic changes, Muscle biopsy was not feasible in most of diagnosed cases, but of which was done revealed non specific inflammatory inflilteration with leucocytes, lymphocytes and eosinophills.
It was peculiar that our young lady case presented with atypical attack of FMF consisting of severe muscle pain & swelling affecting both thigh but not accompanied by fever, rash or abdominal pain o. Also ESR was not elevated as excepected there is no definite rational for that; yet the compliance of the patient to colchicine may abort the elevation of ESR as acute phase reactant. We began to revise the history and to put differential diagnosis. Myopathy related to FMF was on the top after exclusion of vasculitis. Hence Fulfiling the clinical criteria, normal CPK levels & characteristic MRI findings (oedema of subcutaneous fat tissue) together with the evidence of inflammatory myopathy by EMG are the hallmarks of diagnosing PFMS and excluding out the colchicines induced myopathy. Immediately, the decision was made based on the foregoing & Steriods were prescribed with collaporation of physiotherapy team for more than 2 months a good response was achieved and the patient was able to move independently
PFM was first described by Schwabe et al.16 They noticed the attacks of fever and severe myalgia lasting 10-21 days. In 1988 Schapira et al.16 described a patient whose only manifestation of FMF was severe myalgia with fever.17 In 1994 Langevitz et al17 described 14 FMF patients with severe disabling myalgia accompanied by fever, high erythrocyte sedimentation rate, lasting up to 6 weeks3 Transient vasculitic rashes were reported in few cases.
Kaplan et al defined a group of criteria for the diagnosis of PFM in a group of children in 2007.18 Kaplan and co decided that there is a strong association between the M694V mutation and PFM.
PFMS is thought to be a vasculitic process although the supporting pathologic evidence is lacking,19 Interestingly, other vasculitides such as Henoch Schonlein, Bechet's disease, and poly-arteritis nodosa have been found in an increased incidence among FMF patients.20 The exact mechanism describing the pathophysiology of PFMS is unknown, but there may be triggering factors such as an infection, or an interaction with other proteins induced by stress, trauma or hyperthermal balneotherapy,21 these factors regulate the immune response evolving in to an inflammatory state of PFMS in some FMF patients.22
Although colchicine is the cornerstone of FMF treatment, it has clearly been non effectious for PFMS. Corticosteroids is the mainstay in treatment. Though with high-dose steroids elicits resolution of symptoms in 5 –7days,18 It may need prolonged time of intake more than 6weeks for good response.23 Moreover, corticosteroids may not be beneficial in some patients , thus the use of other immunosuppressive was issued in various cases.24 To date, immunomodulatory agents like interferon, and tumor necrosis factor inhibitors have been employed in refractory & severe cases of FMF with variable success but not issued in PFM perse.25
Demonstration of pivotal role of interleukin-1 (IL-1) in the pathogenesis of FMF leads to the use of IL-1 blockers in colchicine resistant or intolerant patients, Interleukin-1 (IL-1) antagonists, as anakinra, canakinumab and rilon accept are reported to be effective in colchicine unresponsive FMF patients.26,27
After reviewing the literatures; all reported cases of adolesecence and adult PFM and our case are summarized in Table 2.13,18,21-23,28-33 Up to that time we found 13 cases of FMF developed PFM. Their age range 12-44yrs with mean age 28±16. Five cases of them were males (38.46%) & 8 (61.53%) females. Five of them with documented positive family history (38.46%) and one patient (7.69%) with reported negative family history. Nine (69.23%) patients were known to have FMF before the emerging the PFM while the rest of patients (30.7%) diagnosed to have FMF at the onset of presentation. All patients shared the typical muscle ach and tenderness, only 8 of them; fever was associated. Normal muscle enzymes with high ESR & CRP were the remarkable lab in diagnosis of all PFM cases. Three of the cases (23.07%) were positive hetregonous for M694V and V726A; three (23.07%) were positive homozygos for M694V while one patient (7.69%) harboured homogenous for E148Q and compound heterogenous P3695-R408Q; while two case(14.38%) beared positive heterozygous mutation E148 and R764.
Number |
Age/ Sex |
FMF |
Symptoms |
Labs |
MRI |
EMG |
Biopsy |
FMF gene |
Typical FMF |
Famiy H/O |
Treatment and outcome |
1 Bircan Z & Usluer H28 |
15 /M |
Known |
Abdpain,vomiting, fever and dehydration Myalgia in prox. Ms. 13 yrs ago |
Slight Inc ALT,AST |
+ve homogenus for |
typical |
+ve |
To colchicine and prednisolone 2mg/kg Follow up : normalization of acute phase reactant |
|||
2Bircan Z & Usluer H28 |
12/F |
Known |
fever, abdominal pain, and myalgia |
Normal ALT,AST,ALP,CK Normal C3,C4 ESR=113mm/h, CRP26.6 mg/Dl Leucocytosis Serology for hepatitis and lupus –ve ANCA -ve |
normal |
typical |
+ve |
prednisolone 2mg/kg Follow up : normalization of acute phase reactant |
|||
3 Schapira D et al.16 |
22/F |
Not known |
Arthritis of ankle,knee joints 16 yrs ago Sever pain in calf mscs with fever |
Normal ALT,AST,ALP,CK,aldolase -ve ANA,ASMA,AMA and RFCRP+++ESR=80 |
normal |
histological:inc in collagen tissue in interstitium with most msc fiber of normal size E/M: most muscle fibres were of normal size with some atrophic cells |
Atypical |
+ve |
No response to prednisolone alone Improved on colchicine 1.5mg/kg Follow up : normalization of acute phase reactant |
||
3Kotevoglu N et al.29 |
13F |
Not known |
Sever RT leg and knee ms pain with fever 3 months inability to walk |
Normal ALT,AST, ALP Leucocytosis Elevated ESR,CRP and CK |
oedema of the subcutaneous fat tissue and the distal part of the medial gastrocnemius muscle prior to the musculo-cutaneous junction of the Achilles tendon |
normal |
Scarce non specific inflamma-tory inflilterat-ion with leucocyte,lymphocytes and eosinophils |
+vehetregonous for M694V and V726A |
Atypical |
Respond to steroids and colchicines Follow up : normalization of acute phase reactant |
|
4ALPAYCI M et al.21 |
33 M |
Not known |
Sever paralyizing myalgia, abd pain, fever, muscle tendrness |
Normal ALT,AST, CK, ASOT,RF -ve virology Leukocytosis ESR=36 CRP=51 |
+ve heterozygous V726A |
typical |
Respond to steroids and colchicines Follow up : normalization of acute phase reactant |
||||
5 Tufan G & Demir S 23 |
30F |
known |
Sever diffuse ms pain and tenderness For 2 months |
Normal CK,ALT,AST leucocytosis -ve ANA,antiDNA, ANCA |
No response to colchicine alone Respond to added steroids , tappered then stopped Follow up : normalization of acute phase reactant |
||||||
6 Fujikawa Ket al.l30 |
22M |
known |
Fever,prolonged myalgia of both UL and LL, abd pain , diarrhea For 3 weeks |
Normal CK Aldolase=6.6 high ESR & CRP ferritin=566 –ve virology |
Thickening of fascia in STIR suggestive of Fasciitis |
striking changes appear in the fascia, including an increased amount of collagen fibrils and infiltration by fibroblasts, macrophages and a few mast cells |
+ve homozygous for E148Q and compound heterogenous P3695-R408Q |
typical |
+ve |
Respond rapidly to small dose steroid 20mg/d and discontinued along 6 weeks Follow up : normalization of acute phase reactant |
|
7 Ertekin et al.31 |
14 M |
known |
Fever,abd pain, sever myalgia all mscs For 25 days |
Normal ALT,AST,CK -ve ANA ESR=92mm/h CRP=15mg/dl |
+ve heterozygous mutation E148Q and R761 |
typical |
+ve |
Respond to steroids within 10 days Follow up : normalization of acute phase reactant |
|||
8 Rıdvan M et al.32 |
41F |
Known 2yrs ago |
severe calf and thigh pain, fever and malaise 4 weeks duration |
Normal ALT,AST,CK Leucocytosis ESR=84 CRP=178 |
MRI revealed remarkable muscle oedema in her calf muscles |
heterozygous M694V mutation |
typical |
Steroid +colchicine recurrence anaqkinra 100mg /day s.c response Follow up : normalization of acute phase reactant |
|||
9 Rıdvan M et al.l32 |
44F |
Known 27yrs ago |
severe right thigh pain for 3 weeks. She also complained of diarrhoea and ankle pain |
Normal ALT,AST,CK ESR=78 CRP=66 |
homozygous for M694V mutation |
typical |
Naproxen +colchicine no response Anakinra 100mg /day s.c response Follow up: normalization of acute phase reactant |
||||
10Senel K et al.33 |
12/M |
Known to be FMF |
LL pain , skin rash,fever inability to walk |
Normal muscle enzymes CRP=12 ESR=108 ASOT=601 Leukocytosis Virology -ve |
Non-spesific changes |
homozygous for M694V mutation |
Steriodes for 3 weeks Follow up: normalization of acute phase reactant |
||||
11Soylu et al.13 |
14/F |
Not known tohave FMF |
UL & LL myalgia, fever & arthralgia |
Normal muscle enzymes CRP=183 ESR=102 ASOT =Normal Leukocytosis Virology –ve ANA,Anti-dsDNA, P-ANCA, C-ANCA -ve |
homozygous E148Q |
atypical |
Improved after 24 hrs from intake of steroids prednisolone 2mg/kg/day Follow up : normalization of acute phase reactant |
||||
12 Brican Z22 |
12/F |
Known |
Abd pain fever Vomiting diarrhea Sever myalgia Skin rash convulsion |
Normal muscle enzymes leucocytosis ESR=115 CRP13.3 ASOT: normal ANA,ANCA –ve Virology -ve |
Normal |
homozygous for the M694V |
typical |
prednisolone 2mg/kg or more than 62 days Follow up: normalization of acute phase reactant |
|||
The patient of this report |
15/F |
Known |
Severe bilateral thigh pain and swelling not associated with fever or abdominal pain for 2 weeks |
Normal muscle enzymes ESR=15 CRP: 47 ASOT: normal Virology & ANA negative |
subcutaneous tissue dema with intact musculature |
patchy myopathy |
Heterozygous for (M694V , E148Q , P369S) |
typical |
+ve |
Steroids 1mg/kg/d for 10 weeks began to improve after 1 month of treatment |
Table 2 Adult PFA
Out of the cases, three (23.07%) only underwent musckuloskeletal MRI on the affected muscles which revealed subcutanoeus and muscle oedema, EMG was done in four cases(30.7%) [normal EMG findings done in 3 (23.07%) cases only, non specific changes in one patient (7.69%). Muscle biopsy was taken in 2 patients which demonstrated histological examination of the striated muscle did not show signs of vasculitis. There was an increase of the collagen tissue in the interstitium of the muscle and also a few inflammatory cells. The electron microscopic examination showed most muscle fibres were of normal size, but atrophic muscle cells of 17-20 im were dispersed. The sarcomere pattern was well preserved. The perivascular basement membrane of capillaries and of small venules was uniformly and moderately widened and the interstitium was infilterated with fibroblasts, macrophages, and a few mast cells.16
Mostly of the patients [10(76.9%)] responded well to steroids while 2 cases showed steroid resistence and achieved proper improvement on the use of an IL-1 inhibitor, anakinra. Owing to the scarcity of studies about the management of steroid resistant PFM, we hereby declare the urgent need to evaluate the management of PFM & variable response to different medication which might be related to phenotypic characteristics such as age of onset, ethnicity, Clinical presentation as well as frequency & the severity of the attacks aside of the genotypic features. Herein, we reported a successful treatment with prolonged use of high dose steroids along 10 weeks with extensive physiotherapy
FMF can be considered to be recognized easily with the classical features including abdominal pain, fever, pleuritis, arthralgia & myalgia. The atypical presentation of PFMS with severe disabling muscle pain and prolonged weakness may be a rare pattern of FMF. We would like to point out that FMF with PFM which respond well to steroids & immunosuppressive drugs to reduce the time of pain and complications.
None.
The author declares there is no conflict of interest.

©2018 Menyawi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.