MOJ
eISSN: 2381-179X


Case Report Volume 9 Issue 5
Advisor in Pediatrics and Pediatric Psychiatry, Children Teaching Hospital of Baghdad Medical City, Iraq
Correspondence: Aamir Jalal Al Mosawi, Advisor in Pediatrics and Pediatric Psychiatry, Children Teaching Hospital of Baghdad Medical City, Iraq
Received: August 20, 2019 | Published: September 16, 2019
Citation: Mosawi AJAI. Pediatric unilateral Vogt Koyanagi Harada syndrome: The second case in the world. MOJ Clin Med Case Rep . 2019;9(5):108?109 DOI: 10.15406/mojcr.2019.09.00316
Vogt Koyanagi Harada syndrome is a systemic autoimmune granulomatous disorder of adults that affects melanocyte-rich, pigmented tissues which contain melanin including the eye, skin, inner ear, meninges, and hair. The most characteristic feature of the syndrome is the bilateral ocular manifestations which include diffuse uveitis presenting with an acute or subacute onset of bilateral visual impairment with or without pain and redness.
Vogt Koyanagi Harada syndrome has not been documented in Iraq. The aim of this paper is to report the first patient with pediatric Vogt Koyanagi Harada syndrome who is the case number 106 and the second case with unilateral Vogt Koyanagi Harada syndrome in the world.
Keywords: ocular manifestations, Vogt Koyanagi Harada syndrome, retinal pigmentation
Vogt Koyanagi Harada syndrome is a systemic autoimmune granulomatous disorder of adults that affects melanocyte-rich, pigmented tissues which contain melanin including the eye, skin, inner ear, meninges, and hair. The syndrome was first described by a Swiss ophthalmologist Alfred Vogt and was named after him and a other two Japanese ophthalmologists. The most characteristic feature of the syndrome is the bilateral ocular manifestations which include diffuse uveitis presenting with an acute or subacute onset of bilateral visual impairment with or without pain and redness.
In 1911, Dr. Jujiro Komoto, a Japanese professor of ophthalmology at the University of Tokyo published in a German language journal “Klinische Monatsblätter für Augenheilkunde” a paper about the condition. In, 1914, Yoshizo Koyanagi, an other Japanese doctor published a paper in the Nippon Ganka Gakkai Zasshi, but his second paper published in 1929 led to the definite association of his name with the syndrome.
In 1926, Einosuke Harada published a paper in Nippon Ganka Gakkai Zasshi included several case reports that was credited for being comprehensively described the syndrome. During the 1970s and 1980s childhood Vogt Koyanagi Harada syndrome has been increasingly recognized. Vogt Koyanagi Harada syndrome has not been documented in Iraq. The aim of this paper is to report the first patient with pediatric Vogt Koyanagi Harada syndrome who is the case number 106 and the second case with unilateral Vogt Koyanagi Harada syndrome in the world.1
A seven-year old girl who developed uveitis manifested by unilateral loss of vision in the right eye associated with retinal pigmentation and blurring of the optic disc was observed (Figure 1).
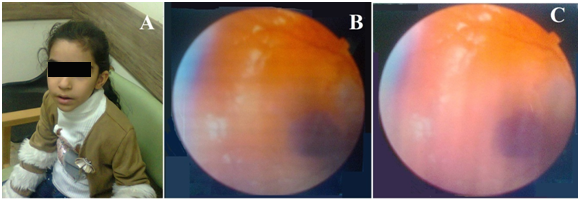
Figure 1 A seven-year old girl. (A) who developed uveitis manifested by unilateral loss of vision in the right eye associated with retinal pigmentation and blurring of the optic disc (B,C).
The girl also had extra-ocular manifestations which included increasing vitiligo (Figure 2) and abdominal pain. The patient condition improved with initial treatment with daily steroids followed by long term cyclosporine. However, the use of cyclosporine resulted in the development of oral ulcers and gingival hyperplasia (Figure 3).
The total number of the reported patients with childhood Vogt Koyanagi Harada syndrome is 105 including only one patient with unilateral ocular involvement reported by Forster and colleagues 1991.1,2 During the 1970s and 1980s, there were only five cases of well documented childhood Vogt Koyanagi Harada syndrome including two patients reported by Weber and Kazdan, 1977; one patient without eye involvement reported by Nordlund et al ,1980; two patients, a brother and sister reported by Ozdirim and colleagues,1980.1
During the 1990s, there were twenty three cases of well documented childhood Vogt Koyanagi Harada syndrome including the first reported patient with unilateral ocular manifestation reported by Forster and colleagues,1991;one patient reported by Gruich et al, 1995; two patients reported by Krásný and Honzová,1995; one patient with severe refractory disorder reported by Cunningham et al,1995; one patient reported by Kara and Elaraoud 1998; three patients reported by Rathinam et al,1998; thirteen patients reported by Tabbara and colleagues,1998; one patient reported by Ikeda et al,1999.1
During the 2000s, there were sixty eight cases well documented childhood Vogt Koyanagi Harada syndrome including two patients reported by Laghmari et al, 2002; One patient reported by Tian'en and colleagues 2003; One patient reported by Kohnen and colleagues, 2004; One patient reported by Swiech-Zubilewicz and colleagues 2005; One patient reported by Rieger and colleagues, 2005; One patient reported by Al Hemidan and colleagues, 2006; ten patients reported by Soheilian et al, 2006; One patient reported by Ghosh et al, 2007; One patient reported by Lucena et al, 2007; One patient reported by Berker et al, 2007; twenty three patients reported by Abu El-Asrar et al, 2008; One patient reported by Benfdil et al, 2010; two patients reported by Khalifa and colleagues, 2010; twenty two patients reported by Martin et al, 2010.1
After 2010, there were nine cases of well documented childhood Vogt Koyanagi Harada syndrome including one patient reported by Venaille et al, 2011; one patient reported by Setiabudiawan, 2011; one patient reported by Ojaimi et al, 2012; one patient reported by Hernandez and colleagues, 2012; one patient reported by Bilgiç and colleagues, 2014; one patient reported by Takada et al, 2015; one patient reported by Yoshida and colleagues ,2016; one patient reported by Khan et al, 2017; one patient reported by Budmann and colleagues, 2018.1
The primary pathogenesis of Vogt Koyanagi Harada syndrome is T cell-mediated autoimmune response directed towards melanocyte or melanocyte-associated antigens causing diffuse inflammatory condition involving most parts of eye.1,3 The diagnosis is achieved mainly by clinical features.1–4
Early treatment with systemic corticosteroids and early non-steroidal immunosuppressive drug therapy can reduce vision threatening ocular complications and lead to good visual recovery.3 Treatment of Vogt Koyanagi Harada syndrome include.2,3
Review of the available evidence suggested that mycophenolate mofetil can provide the same therapeutic benefit, but without the development of gingival hyperplasia.
The author would express his gratitude for the father of the patient who accepted publishing her photos.
None.
There is no conflict of interest.

©2019 Mosawi. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.