MOJ
eISSN: 2381-179X


Case Report Volume 15 Issue 1
1Department of Internal medicine, Military Polyclinic of Kasserine, Tunisia
2Sfax Faculty of Medicine, University of Sfax, Tunisia
3Department of Ophthalmology, Regional Hospital of Kasserine, Tunisia
4Sousse Faculty of Medicine, University of Sousse, Tunisia
5Department of ENT, Military Hospital of Tunis, Tunisia
6Tunis Faculty of Medicine, Tunis El Manar University, Tunisia
Correspondence: Dr Salem Bouomrani, Department of Internal medicine, Military Polyclinic of Kasserine, Tunisia, Tel +00216 98977555
Received: January 07, 2025 | Published: February 5, 2025
Citation: Bouomrani S, Nefzi D, Mansouri O, et al. Paraneoplastic Sjögren’s syndrome revealing undifferentiated parotid carcinoma. MOJ Clin Med Case Rep. 2025;15(1):5-7. DOI: 10.15406/mojcr.2025.15.00475
Paraneoplastic Sjögren's syndrome remains exceptional with only a few sporadic observations found in the literature. It represents a real diagnostic challenge for health professionals, particularly since the association of primary Sjögren’s syndrome and cancer is now well established; as is the possibility of secondary lymphomatous transformation of this syndrome. We present the exceptional case of paraneoplastic Sjögren’s syndrome revealing undifferentiated parotid carcinoma in a 43-year-old Tunisian man with no significant pathological history. The diagnosis of these two pathologies was made synchronously and the clinical and immunological signs of Sjögren's syndrome disappeared completely after three months of radical surgical treatment of the underlying cancer. As rare as it is, this paraneoplastic syndrome deserves to be well known by clinicians, and systematic screening for an underlying cancer is essential for any recently diagnosed Sjören's syndrome given the high ancogenic risk inherent in this connective tissue disease.
Keywords: paraneoplastic syndrome, Sjören's syndrome, parotid gland, undifferentiated carcinoma
Since the initial description in 1916, the list of rheumatological paraneoplastic syndromes has continued to increase day by day.1 The average overall incidence of these syndromes is estimated at 2.65-23.1% depending on the series and the nature of recruitment (rheumatological or other).1
These syndromes are mainly represented by: pseudo polyarthritis rheumatica (polymyalgia rheumatica), dermatomyositis/polymyositis, palmar fasciitis, remitting seronegative symmetrical synovitis with pitting edema (RS3PE syndrome), seronegative asymmetric polyarthritis, rheumatoid arthritis-like syndrome (RA-like), systemic lupus erythematosus-like syndrome (SEL-like), and Marie-Bamberger hypertrophic osteoarthropathy.2,3
Dry syndrome or Sjögren's syndrome remains exceptional as an autoimmune rheumatological paraneoplastic syndrome.4,5 It represents a real diagnostic challenge for health professionals, particularly since the association of primary Sjögren’s syndrome and cancer is now well established; as is the possibility of secondary lymphomatous transformation of this syndrome.6 We describe here an exceptional case of paraneoplastic Sjögren’s syndrome revealing undifferentiated parotid carcinoma.
A 43-year-old Tunisian man with no significant pathological history was referred to our department of Internal Medicine by his family doctor for suspected Sjögren's syndrome: xerostomia with xerophthalmia, left parotid swelling, and seronegative polyarthritis that had been developing for three months and had not improved with specific symptomatic treatment.
The clinical examination noted an afebrile patient with a relatively preserved general condition, a firm, fixed, and painless swelling of the left parotid gland without skin involvement over it, and synovitis of both hands and both wrists without joint deformities.
The specialized ophthalmological examination confirmed dry eye syndrome. Standard radiographs of the painful joints did not show any joint destruction. The basic biology showed a marked biological inflammatory syndrome: erythrocyte sedimentation rate at 80mmH1, C-reactive protein at 15mg/l and normochromic normocytic anemia at 10g/dl. The rest of the basic biology was without abnormalities.
The immunological study showed positive antinuclear autoantibodies at 1/640 with speckled fulorescence and positive anti-SSA autoantibodies. The biopsy of the accessory salivary glands showed chronic lymphocytic sialadenitis with a focus score of 1 and absence of neoplastic cells or granulomas.
The diagnosis of Sjören's syndrome was confirmed by the association of: xerostomia, xerophthalmia, positive ocular tests, positive antinuclear and anti-SSA antibodies, and focus score of 1 on labial histology) validating the diagnostic criteria of this connective tissue disease.
Parotid ultrasound showed an enlarged parotid with a heterogeneous tumor, poorly defined, and hyper vascularized on Doppler, associated with multiple satellite adenopathies (Figure 1). Computed tomography (CT) scan showed a parotid swollen by a parenchymal tumor, hypodense, heterogeneous, and enhancing heterogeneously after injection of contrast product. This tumor infiltrated the peri-parotid fat with multiple adenopathies of secondary appearance (Figure 2 & 3).

Figure 1 Cervical ultrasound: Heterogeneous tumor of the left parotid gland (A) with multiple enlarged lymphatic nodes (B).

Figure 2 Axial CT scans of the parotid gland, without contrast: Parenchymal, hypodense, and heterogeneous tumor of the left parotid gland with multiple adenopathies.
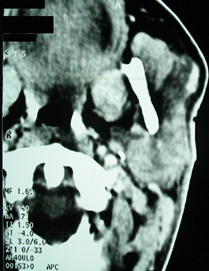
Figure 3 Axial CT scans of the parotid gland, with contrast: parenchymal parotid gland tumor enhancing heterogeneously after injection of contrast product.
Parotid fine needle aspiration cytology pointed to an undifferentiated carcinoma. The loco regional and distant extension assessment did not show any metastatic lesions. The patient was transferred to the otorhinolaryngology department for surgery. He underwent a total left parotidectomy with homolateral lymph node evidement. Additional radiotherapy was also indicated with a favorable outcome.
The follow-up after three months of surgery showed the total disappearance of somatic complaints (xerostomia, xerophthalmia, and arthralgia). The joint examination was without abnormalities and the immunological tests were negative, confirming the paraneoplastic character of this Sjögren's syndrome.
Paraneoplastic Sjögren's syndrome remains exceptional with only a few sporadic observations found in the literature.7–14 Similarly, in large series of solid cancers and/or malignant hematological diseases with paraneoplastic syndromes, Sjögren's syndrome is only exceptionally found: in the Ukrainian series of Dumansky YV et al.,4 of 1669 cases of lung cancer of which 258 presented a paraneoplastic syndrome, Sjögren's syndrome was found in only 0.19% of cases,4 and in the series of 221 cases of myelodysplastic syndromes of Henright H et al.,5 only two cases of paraneoplastic Sjögren's syndrome were noted (0.90%).5
Paraneoplastic Sjögren's syndrome was first reported in 1983 by Trubnikov GV et al.,10 in association with lung cancer.10 Since then, it has been reported in several other cancers: breast,9 thymus,11,15 kidney,12 stomach,14 pancreas,16 and myelodysplastic syndromes.5 The association with lung cancer remains the most frequent.4,7,8,10,13
The clinical presentation of paraneoplastic Sjögren's syndrome can be complete (xerostomia, xerophthalmia, bilateral and symmetrical polyarthritis without joints destruction or deformities, and positive specific ocular tests) or incomplete.7–9,11,16 It can also be summarized as a simple paraneoplastic autoimmune xerostomia.17
Antinuclear autoantibodies, anti-SSA autoantibodies and rheumatoid factor can be positive and at very high levels.7,9,11 Similarly, salivary scintigraphy and histology of accessory salivary glands can show typical features of primary Sjögren's syndrome.8,9
This situation represents a real diagnostic challenge for clinicians because the association between primary Sjögren's syndrome and cancers is well established as well as the risk of secondary lymphomatous transformation of disease.6,18,19 The risk of lymphomatous transformation during Sjögren's syndrome is estimated at 5%.18,19 The salivary glands represent the most frequent extra-nodal site of these lymphomas,20,21 and the Mucosa-Associated Lymphoid Tissue Non-Hodgkin Lymphoma (MALT) subtype is the most frequent.18–21 Indeed, and despite their rarity in the general population, salivary gland lymphomas are significantly frequent in patients followed for primary Sjögren's syndrome: in a large pooled analysis including 29,423 participants, PSS was associated with a 6.5-fold increased risk of non-Hodgkin lymphoma and a 1000-fold increased risk of marginal zone lymphoma of the parotid gland.22
The elements pointing towards a paraneoplastic origin are: the onset and rapid progression/aggravation of xerosis and/or arthritis, the absence or poor response to specific anti-rheumatic symptomatic treatments, weight loss and obvious deterioration of the general condition7,8. Similarly, the lack of improvement of dry syndrome and arthritis under systemic corticosteroids should suggest an underlying cancer.12
Paraneoplastic Sjögren's syndrome may precede cancer,8,12,14,16 be diagnosed simultaneously with cancer,7,9,11 or occur during the course of advanced and metastatic cancer.11 It may be isolated or associated with other paraneoplastic manifestations: subacute sensory neuropathy,9 Lambert-Eaton myasthenic syndrome,13 and mucous membrane pemphigoid.15
Theoretically, the clinical signs and immunological abnormalities of paraneoplastic Sjögren's syndrome should completely disappear after radical treatment of the underlying tumor.5,12
As rare as it is, this paraneoplastic syndrome deserves to be well known by any health professional. The differential diagnosis between a paraneoplastic Sjögren's syndrome and an authentic primary Sjögren's syndrome associated with cancer or a secondary malignant transformation of a previously unrecognized Sjögren's syndrome is not always easy. Thus, systematic screening for an underlying cancer is essential for any recently diagnosed Sjören's syndrome given the high ancogenic risk inherent in this connective tissue disease.
Oral and written Informed consent were obtained from the patient.
None.

©2025 Bouomrani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.