MOJ
eISSN: 2381-179X


Case Report Volume 14 Issue 3
1Interim Assistant Academic Surgical Unit A, Universidad de la República Uruguay, Uruguay
2Associate Professor of the Academic Surgical Unit A, Universidad de la República Uruguay, Uruguay
3General Surgery Resident Academic Unit A, Universidad de la República Uruguay, Uruguay
4Interim Assistant Academic Surgical Unit F, Universidad de la República Uruguay, Uruguay
5General Surgery Resident Academic Unit F, Universidad de la República Uruguay, Uruguay
Correspondence: Ulises Parada, Associate Professor of the Academic Surgical Unit A, Universidad de la República Uruguay
Received: August 05, 2024 | Published: August 20, 2024
Citation: Ulises P, Merino G, Stop U, et al. Pancreatic trauma with surgical indication. Case series in three centers in Montevideo-Uruguay. MOJ Clin Med Case Rep. 2024;14(3):62-66. DOI: 10.15406/mojcr.2024.14.00465
Introduction: Pancreatic trauma is a rare event in 0.5-8% of trauma patients, with high morbidity and mortality (8.6-15%). Diagnosis is generally difficult, so clinical suspicion must be high. Associated visceral injuries are the rule. The challenge lies, in addition to the diagnosis, in making a correct classification of these lesions, which will have therapeutic implications that directly influence the morbidity and mortality of this pathology.
Objective: To report a series of cases of patients with pancreatic trauma who required surgery.
Methods: A retrospective observational analysis was carried out on patients with open or closed abdominal trauma undergoing surgery who presented pancreatic injury.
Results: A series of 5 clinical cases of traumatic pancreatic injuries are described, in which penetrating trauma predominates. All required surgical treatment due to the presence of hemodynamic instability and open trauma with evisceration of intra-abdominal organs. Treatment was individualized, using different surgical techniques depending on the degree of pancreatic injury and hemodynamic status. Of the complications, pancreatic fistula was the most frequent and there were no deaths in the series of cases presented.
Keywords: pancreatic trauma, pancreas, classification of pancreatic injuries, pancreatic trauma treatment, damage control surgery
Pancreatic trauma is a rare entity, occurring in 0.3-8% of polytraumatized patients, and this injury can be associated with both blunt and penetrating trauma.1–4 The importance of morbidity and mortality is highlighted, which is around 50 to 70% according to published data, conditioning the medium and long-term evolution of these patients.4,5 To recognize these injuries, it is necessary to maintain a high level of clinical suspicion and know the injury mechanism. Although the diagnosis of traumatic pancreatic injuries has improved with the availability of imaging techniques, there is still difficulty in their early identification. The challenge lies, in addition to the diagnosis, in making a correct classification of these lesions, which will have therapeutic implications that directly influence the morbidity and mortality of this pathology. By achieving a correct classification of these injuries, an appropriate and individualized treatment can be established. To define the prognosis in pancreatic trauma, the American Association for Surgery for Trauma (AAST) classification is used, which divides them according to the degree of ductal injury and the pancreatic parenchyma from I to V.6 Other variables mentioned to assess the prognosis are , the modified trauma mortality score (RTS), as well as the associated injuries it presents.4,7 he objective of this work is to report a series of cases of patients with pancreatic trauma who required surgery and analyze the different variables, comparing them with data from the relevant literature.
A retrospective observational analysis is carried out on patients with open or closed abdominal trauma undergoing surgery who presented pancreatic injury, assisted in the period December 2019 to March 2022, reported in 3 healthcare centers in Montevideo, Uruguay. The following variables are considered: sex, age, traumatic mechanism, location of the injury (head, body, tail), pancreatic duct involvement, presence or absence of injury to other organs, surgical tactics, complications and mortality.
Of a total of 5 patients, the average age of presentation is 30 years (range between 15 to 66 years), with males predominating in 4 cases. In 4 of the patients the injury mechanism was penetrating trauma, 3 with a gunshot wound and one injury from a grinder. The blunt trauma occurred in the context of a patient multiple traumatized by a traffic accident (Table 1). Upon admission, two patients presented with stable hemodynamics, of which one became unstable during the course. Accounting for a total of 4 of 5 patients with hypovolemic shock. The diagnosis of pancreatic lesions was made in 4 of the cases intraoperatively based on surgical exploration and one preoperatively with Computed Tomography (CT). No request for any other imaging method was made. Regarding the lesion topography, the most frequent lesion site affected was the body of the pancreas (3), followed by the neck (1) and the uncinate process (1). The main pancreatic duct was found compromised in 2 of the cases with its total section. According to the AAST classification of pancreatic injuries based on imaging and intraoperative findings, they were grade II and IV injuries. The most frequent associated injuries were: the liver in all cases, followed in frequency by the stomach, portal vein, diaphragm, colon and vena cava.
|
1 |
2 |
3 |
4 |
5 |
x age |
|
|
Age |
30 |
15 |
66 |
17 |
26 |
30.8 |
|
Sex |
M |
M |
M |
F |
M |
|
|
Injury mechanism |
Penetrating (HAF) |
Blunt (PTM) |
Penetrating (Grinder) |
Penetrating (HAF) |
Penetrating (HAF) |
|
|
Hemodynamics |
shock |
shock |
Normal |
shock |
shock |
|
|
Injury association |
IVC, Hepatic |
Gastric, Hepatic |
Gastric, Hepatic |
Hepatic, Gastric, VP |
Diaphragmatic, Colonic, Hepatic. |
|
|
Topography of pancreatic injury |
uncinate process |
Neck |
Body |
Body |
Body |
|
|
Mesenteric vessels |
Right |
Right |
Right |
Left |
Left |
|
|
Wirsung duct injury |
No |
Yes, total section |
Yes, total section |
No |
No |
|
|
AAST Classification |
II |
IV |
IV |
II |
II |
|
Table 1 Variables, injury association and classification of pancreatic injury according to AAST
The indication for surgery in this series of cases arose due to the presence of hemodynamic instability and in one of the cases due to penetrating trauma with evisceration of abdominal organs. The surgical tactic was variable. Damage control surgery was performed in most patients, with drainage facing the pancreatic bed. Surgical techniques included pancreatic raffia, distal pancreatectomy with splenectomy and pancreatic-jejunum anastomosis. Relaparotomy was necessary in 4 patients, after damage control surgery at 24 and 48 hours (Table 2). The most frequent complication was pancreatic fistula in 3 patients, followed by pancreatic pseudocyst, liver abscess, portal vein thrombosis and repeated pancreatitis in one case. No deaths were recorded in all of the cases reviewed. (Table 3–5 &Figures 1–6)
|
1 |
2 |
3 |
4 |
5 |
|
|
Complications |
Pancreatic pseudocyst Recurrent pancreatitis |
pancreatic fistula |
pancreatic fistula |
No |
Pancreatic Fistula liver abscess Portal thrombosis |
|
Death |
No |
No |
No |
No |
No |
Table 2 Complications and mortality
|
1 |
2 |
3 |
4 |
5 |
|
|
Surgical tactics |
Damage control, raffia, AAC |
Damage control, drainage, AAC Pancreatic-jejunum anastomosis |
Distal pancreatectomy |
Damage control, raffia, AAC |
Damage control, raffia, AAC |
|
Relaparotomy |
Yeah |
Yeah |
No |
Yeah |
Yeah |
|
Splenectomy |
No |
No |
Yeah |
No |
No |
Table 3 Surgical treatment
|
Degree |
Type of injury |
Description |
|
Yo |
Hematoma |
Minor contusion without ductal injury. |
|
Laceration |
Superficial laceration without ductal injury. |
|
|
II |
Hematoma |
Major contusion without ductal injury or tissue loss. |
|
Laceration |
Major laceration without ductal injury or tissue loss. |
|
|
III |
Laceration |
Distal pancreatic section or pancreatic and ductal injury. |
|
IV |
Laceration |
Proximal pancreatic section or pancreatic injury with ampullary involvement. |
|
V |
Laceration |
Massive cephalo-pancreatic destruction. |
Table 4 AAST classification of pancreatic lesions
Source: Moore. AAST article.
|
Injury degree |
Description |
|
Type I injury |
Radiologically normal duct |
|
Type IIa injury |
Contrast in branches of the pancreatic duct that do not leak from the pancreatic parenchyma |
|
IIb |
The contrast of the branches of the pancreatic duct filters towards the retroperitoneum. |
|
Type IIIa injury |
Main duct injuries. |
|
IIIb |
Duct injury in head of pancreas |
Table 5 Classification of ductal lesions by ERCP
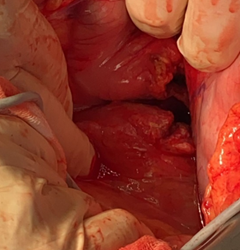
Figure 1 GII pancreatic lesion due to gunshot wound. There is a 3 cm laceration at the level of the neck of the pancreas. Indicated with arrow.
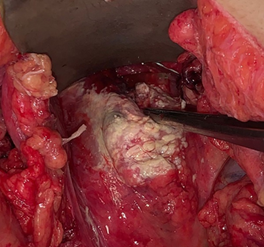
Figure 2 Pancreatic raffia with crossed surget of Polypropylene 3.0 in relaparotomy at 48hs. Elements of cytosteatonecrosis are also observed.
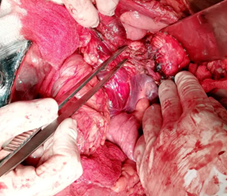
Figure 3 GIV pancreatic lesion, complete section at the level of the pancreatic neck with ductal lesion, due to blunt trauma in a polytraumatized patient.
The pancreatic trauma in this series of cases occurred with a mean age of 30 years, highlighting ages between 20 and 65 years, this agrees with what has been reported in the literature. It is suggested that, in young patients, due to their physical build, it may be related to the presence of less peripancreatic protective fat.4 According to the literature, it is more common in males (60-80%), as is the case in this series.7 The injury mechanism varies depending on the geographical regions considered. Blunt trauma predominates in developed countries with a low prevalence of civil violence.3 In the series presented, penetrating trauma from gunshot wounds and grinding injuries predominated.
Hemodynamic instability, of great importance in polytraumatized patients to define both diagnostic and therapeutic conduct, occurs in 4 of the 5 cases. Which is above what is reported in the bibliography (50%).8,9 The use of the different diagnostic techniques will depend on the patient's hemodynamic status. Early diagnosis is of great importance since it is directly related to mortality. Pancreatic lesions, at the beginning, can go unnoticed in multiple lesions, which can lead to a late diagnosis.3 Therefore, it is recommended that if laparotomy is performed, the pancreas duodenum should be explored when there is clinical suspicion due to the injury mechanism, even if the initial imaging does not suggest injury. Intraoperative cholangiography is a useful diagnostic tool in this situation. If there is an unfavorable evolution during non-operative management, laparotomy is necessary to rule out a pancreatic injury that has gone unnoticed in imaging methods.9 In the analyzed cases, hemodynamics (4 unstable patients) are what determines the opportunity for surgery, dispensing with an imaging study due to the severity of the clinical situation. This results in early diagnosis given by thorough surgical exploration due to the high level of suspicion of the operating surgical team.
Regarding diagnostic studies, requesting serum amylase and lipase may be useful, but should be considered only in the first 4-6 hours of the trauma. It has high sensitivity, but low specificity. CT on admission has low sensitivity and specificity for pancreatic lesions (47-60%). Being higher for injuries to the main pancreatic duct, reaching up to 90%. Taking the above into account, repeating the tomography should be considered between the first 12 and 24 hours, if suspicion of pancreatic ductal injury remains high with a normal beginning tomography.3,5 In this series of cases, a patient underwent initial computed tomography which evidenced pancreatic injury . This injury was confirmed intraoperatively and was classified as grade IV (AAST), with complete Wirsung section at the neck level.
The most sensitive and specific study for the diagnosis of pancreatic injury is abdominal magnetic resonance imaging (MRI) and magnetic cholangioresonance imaging (CMR). Without embargo In the acute context of a multiple trauma patient, with potentially unstable associated injuries, it is difficult to perform it initially (performance time 30-60 min). It should be taken into account when there is a suspicion of injury in the evolution of patients once stability is achieved. In a small series of cases, a diagnosis was made with 100% accuracy in CMR and MRI of the abdomen to identify parenchymal and ductal lesions, avoiding the risks of the ERCP procedure. Retrograde cholangiography (ERCP) has high sensitivity (90%) for these lesions, mainly for lesions of the pancreatic duct. Being the preferred method for diagnosis in hemodynamically stable patients.3,10 During the emergency department care of the patient who has suffered a possible pancreatic lesion, the study of choice will be CT, this allows us to perform a diagnostic approach at the first contact with the patient. And in those cases in which the patient's condition allows it, in order to increase the diagnostic sensitivity and specificity of the pancreatic lesion, MRI and CMR are performed.
In addition to the diagnosis, the classification of these lesions is essential to subsequently decide the therapeutic tactic. For this, the degree of injury at the level of the pancreatic parenchyma and the presence or absence of ductal involvement are relevant. It is evaluated according to the ASST classification of pancreatic trauma, which takes into account the type of injury (hematoma, laceration), topography (proximal, distal) and ductal involvement. If ERCP is performed, to assess the degree of ductal injury Takishima et al.11 They classify them into three categories. In a review of 18 case series carried out in 2016 by Petrone, in the USA. A higher percentage of grade III injuries is reported (23%), followed by grade II (16%), grade I (9%), grade IV (8%) and grade V (3%). The most frequent topography was at the level of the body of the pancreas, followed by the tail, head and neck. The degree of ductal injury predominated type IIIa (32%), followed by IIb (23%) and to a lesser extent I 15%, IIa19%, IIIb11%.12
In a multicenter cohort study from Japan, 45.4% grade I, 8.9% grade II, 24% grade III, 8.3% grade IV, 13.5% grade V are reported.4 In this series, 3 cases were reported with grade II injuries and 2 with grade IV injuries, presenting ductal involvement in 2 of the 5 cases. All were diagnosed intraoperatively. Associated injuries in these patients are the rule, given the location of said organ and the close relationship with the different structures. In the literature, the most frequent injury association is reported to be liver (20.9%), gastric (17.2%), major vascular (14.3%) and duodenal injuries (8.5%), which rises to 12-21% if the injury is penetrating.12
When serious injuries are analyzed, the main injury association is hepatic (15.7%) and vascular (15.5%), followed by splenic injuries (9.3%), mesenteric injuries (8.1%), duodenal injuries (5.8%) and kidney injuries (5.4%).4 In this series, all patients had associated injuries. The most frequent was liver injury in all cases, as reported in the literature, followed in frequency by stomach, portal vein, diaphragm, colon and inferior vena cava. Regarding treatment, although conservative management of certain injuries is feasible, in the series of cases presented, we focused on patients with pancreatic trauma with surgical indication.
Conservative treatment is proposed for patients who are hemodynamically stable and without associated injuries that require surgery. According to the literature, this is performed in grade I and II pancreatic lesions, prioritizing oral suspension, strict monitoring, hydroelectrolyte replacement and total parenteral nutrition. Laparotomy being an option in the case of compartment syndrome in the evolution.3,4 Mini-invasive treatment is considered for patients with non-operative management or in patients in whom initial damage control surgery was performed. Percutaneous drainage is indicated in peripancreatic collections and ERCP if ductal injury is found. The latter is considered the least invasive and effective option for its resolution. By placing a stent and sphincterotomy, it is possible to reduce the need for surgery, allow drainage of contents to the duodenum, block leaks and reduce pancreatic inflammation.3,5
Regarding surgical treatment, there is a great debate about what is the best strategy. This can range from damage control surgery with drainage facing the pancreatic bed in severe cases, to pancreatic resection.
It must be individualized for each patient, according to hemodynamics and the degree of injury. Damage control surgery is the best tactic in severe cases, it can reduce mortality, but it has high morbidity. This is why, as mentioned above, emphasis should be placed on endoscopic management of the ductal injury, once the acute phase has passed specific surgical treatment is required, initial pancreatic resection is recommended for grade III and IV lesions. In grade III lesions, distal pancreatectomy plus splenectomy is indicated. This reduces morbidity and avoids reintervention. Splenic conservation is debated since it would imply longer surgical time. In proximal injuries, there is no unified criterion; the tactic will be individualized and according to each stage. In general terms, for lesions in the neck of the pancreas with ductal involvement, pancreatic resection and pancraticojejunostomy/pancreaticogastroanastomosis are considered, with conservation of pancreatic parenchyma to avoid pancreatic insufficiency. Emergency pancreaticoduodenectomy (CPD) has been displaced by non-operative management; it is considered the last option given its high mortality. It is feasible in cases of cephalic disruption, when there is an association of duodenal injury and it must be performed in a phased manner, with reconstruction in the second instance.3,5,12 In the cases presented, exploration of the duodenum-pancreas during laparotomy was performed as the first diagnostic maneuver. Damage control surgery was the first option in 4 of the 5 patients, performing relaparotomy with surgical resolution in the second instance. Endoscopic management of the ductal lesions was not performed after the acute phase, and surgical treatment with ductal closure and pancraticojejunostomy was chosen. The morbidity of this pathology is very high. Although the record of short- and long-term organ-specific complications is variable, the most common short-term complication is pancreatic fistula, while in the long term pancreatic pseudocyst predominates.
Other complications described are peripancreatic collections, subhepatic abscesses, acute pancreatitis, and bile duct strictures. In this series, pancreatic fistula was observed in 3 cases, resolving spontaneously in all of them. It was more frequent in patients in whom damage control was performed, which agrees with what has been reviewed in the literature. The long-term complications were: one case with a pancreatic pseudocyst, another with liver abscess and repeated pancreatitis. Only one patient did not present postoperative complications. In the literature, mortality is reported to be around 14.3% of pancreatic traumas. Mortality is directly related to age, the degree of AAST injury, the coexistence of severe abdominal injury, and the revised trauma score (RTS), which assesses the degree of consciousness, systolic blood pressure, and oxygenation on admission.4 No deaths were reported in the series presented, highlighting that the number of cases is not representative. All patients gave consent, accepting the surgical procedure.One of the main limitations of the present study is the number of patients. It is a small sample, from which we cannot draw conclusions that can be extrapolated to the population.
Pancreatic trauma constitutes a true diagnostic and therapeutic challenge for the emergency surgeon. Although this is a series of cases, injuries due to penetrating trauma and in males predominate. Furthermore, associated injuries were the rule and surgical exploration was the first diagnostic step in most cases. Regarding treatment, damage control surgery and staged management was the tactic used in 4 of the 5 patients due to the severity of the injuries. Conservative management with the development of mini-invasive techniques is a feasible approach in lower grade injuries. However, the hemodynamic situation and associated injuries often determine the management algorithms, leading to the need to dispense with preoperative imaging studies. The surgical tactic must be individualized, and adjusted to the patient's general condition, degree of pancreatic injury and associated injuries, with therapeutic alternatives ranging from damage control surgery to large resection surgeries such as distal pancreatectomy and even pancreaticoduodenectomy. The common denominator is a high level of suspicion and the correct examination to identify and adequately classify the pancreatic injury, a critical point for defining the patient's treatment and prognosis.
None.
The authors declare that there is no conflicts of interest.

©2024 Ulises, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.