MOJ
eISSN: 2381-179X


Case Report Volume 10 Issue 4
1Department of Infectious Diseases, Hamad Medical Corporation, Qatar
2Department of Internal Medicine, Hamad Medical Corporation, Qatar
3Neuroscience Institute, Neuroradiology Department, Qatar
Correspondence: Sreethish Sasi, Medical Resident, Department of Internal Medicine, Hamad Medical Corporation, Qatar
Received: July 26, 2020 | Published: August 10, 2020
Citation: Varghese M, Sasi S, Nair AP, et al. Neurobrucellosis presenting as stroke: A case report from Qatar. MOJ Clin Med Case Rep . 2020;10(4):94-96. DOI: 10.15406/mojcr.2020.10.00352
Brucellosis is a zoonotic disease that is endemic to the Arabian Peninsula and is found to affect many organs of the human body. Neurological manifestations with brucellosis were reported in 25% of cases. However, most cases suggested the involvement of the central nervous system (CNS) by invasion through the blood-brain barrier. Here, we report a 45-year old male patient who presented with sudden onset right upper and lower limb weakness, similar to the presentation of an ischemic cerebrovascular accident (CVA), associated with constitutional symptoms of fever and low back pain. The patient had no signs to suggest cranial nerve or cord involvement. Further analysis showed that his blood and serum samples were positive for Brucella spp. He was treated with intravenous ceftriaxone for seven days, followed by oral doxycycline and rifampicin for three months. He was asymptomatic at follow-up after three months. Neurobrucellosis can present with stroke-like symptoms, and in endemic areas, prompt testing of brucella serology is warranted in patients presenting as stroke with systemic symptoms.
Keywords: neurobrucellosis, stroke, cerebrovascular accident
CVA, cerebro vascular accident; LDH, lactate dehydrogenase; CSF, cerebrospinal fluid; TB, tuberculosis; CT, computed tomography; MRI, magnetic resonance imaging; CRP, c-reactive protein; ESR, erythrocyte sedimentation rate; HIV, human immunodeficiency virus; PCR, polymerase chain reaction; CNS, central nervous system
Human brucellosis is a common anthropo-zoonotic disease endemic to the Arabian Peninsula. The principal characteristic of human brucellosis is a prolonged fever, which can manifest as Malta fever, Mediterranean fever, and undulant fever.1 It is transmitted either directly through close contact with infected animals or indirectly through infected milk and meat.2 The nervous system's involvement is uncommon and has been reported in about 2-10% of cases.3,4 Three species of Brucella were mainly found to infect humans namely B. melitensis, B. suis, and B. abortus.5 Neurobrucellosis can manifest at any stage of the disease with varying severity, involving central or peripheral nervous system leading to neuritis, radiculitis, myelitis, compression of the spinal cord, meningitis, and meningoencephalitis.6 Cerebrospinal fluid (CSF) is abnormal in most cases though normal CSF has been reported in a few cases.7 Skin lesions of brucellosis were associated with recurrent attacks of vasculitis, suggesting that the same mechanism can lead to stroke, as reported in one case.8 Diagnosis of Neurobrucellosis relies on clinical features and imaging in the background of ongoing Brucella infection. Here we report, a middle-aged male who presented with stroke and found to have positive microbiology and serology for Brucella.
A 45-year-old Bangladeshi male working as a livestock farmer in Qatar presented to the emergency department with acute onset of weakness of the right side of the body, requiring assistance for walking. There were no seizures, altered sensorium, or history suggestive of cranial nerve involvement. The patient had a low-grade fever, significant weight loss, and low back pain during the last two months. He was on metformin for newly detected diabetes over the previous four months. On examination, he was febrile with an oral temperature of 38.1 degrees Celsius but otherwise stable. He had right hemiparesis with upper limb power of 2/5 proximally, 3/5 distally, and 2/5 in the right lower limb with hyperreflexia. Other systems were unremarkable. A non-contrast computed tomography (CT) of the brain showed ill-defined small hypodensity in the left corona radiata, which the neurologist decided to treat as acute ischemic CVA. The echocardiogram was unremarkable and ruled out any cardioembolic cause. Given his prolonged constitutional symptoms, specific blood tests for tuberculosis (TB), brucellosis, syphilis, and autoimmune workup were requested, including cerebrospinal fluid (CSF) analysis, magnetic resonance imaging (MRI) of the brain and spinal cord. IgG and IgM serology for B. melitensis and B. abortus were positive (titers >1:80). Blood cultures grew B. canis. MRI Brain and spinal cord showed L1-L2 spondylodiscitis with similar spondylitis like lesions in the superior anterior endplates of T9 and focal right occipital-temporal meningeal enhancement. CSF was unremarkable. TB, Human Immunodeficiency Virus (HIV), syphilis, and autoimmune workup were negative. Ultrasound abdomen showed only a small calcific density within the right lobe of the liver, measuring 4mm. He was treated as a case of neurobrucellosis, given his prolonged symptoms, positive blood culture, and serology, despite normal CSF, with intravenous ceftriaxone 2grams intravenous twice daily for seven days followed by oral doxycycline 100milligrams twice daily and rifampicin 600milligrams daily for three months. After three months of treatment, he had completely recovered from his symptoms when followed up in the infectious diseases’ clinic.
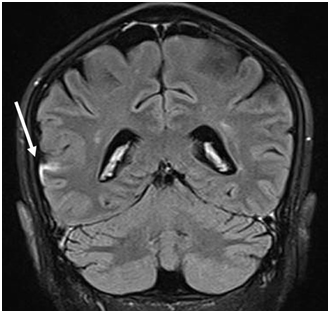
Figure 1 Coronal FLAIR-T2 MRI image post contrast showing leptomeningeal thickening and enhancement (arrow) along the right fronto-temporal sulcus.
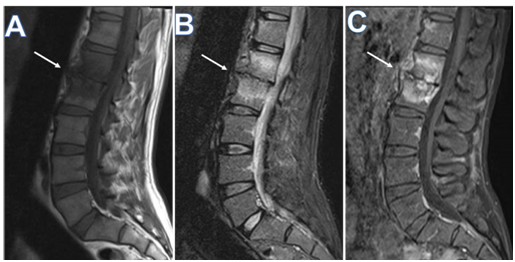
Figure 2 Sagittal MRI of the lumbosacral spine, (A) T1 weighted, (B) T2 weighted, and (C) T1-fat saturated post I.V. gadolinium based contrast medium, showing spondylodiscitis involving Lumbar vertebral bodies L1 and L2, and interposed intervertebral disc, a central pattern with disc destruction, opposed end plate irregularity (arrows in A, B , and C), and diffuse marrow edema, the latter appearing as low signal on T1W, bright on T2W, and post contrast enhancement. Note, minimal prevertebral subligamentous inflammatory changes, and mild posterior epidural bulge against anterior thecal sac.
The Brucellosis is an endemic zoonotic disease transmitted through contaminated meat products or unpasteurized milk,3 commonly infecting livestock farmers and veterinary persons, as in our patient who was a livestock farmer.9 It is also one of the most common laboratory-acquired infections known as laboratory-acquired brucellosis (LAB).10 Though brucellosis is endemic to Arabian Peninsula, neurobrucellosis remains rare. In a case series of nine patients with neurobrucellosis, the average age group of the patients was 49 years, and the manifestations were meningitis, meningoencephalitis, stroke, and abnormal CSF with evidence of vasculitis in imaging.11 Two cases of neurobrucellosis presenting with polyradiculopathy with myelitis are also described.9 Cases of neurobrucellosis presenting with fever, headache, and stroke have been described in literature similar to our situation. CSF was abnormal in most cases with high protein content and lymphocyte-predominant cell count, but negative culture.13 There are no randomized control trials for the efficacy of various combination therapies for brucellosis and neurobrucellosis. Young et al.14 suggested that the combination of rifampicin, doxycycline, and trimethoprim or sulfamethoxazole (TMP/SMX) for several months may be the most effective. ceftriaxone with better CNS penetration is also favored for the treatment. The recommended duration of therapy is for a minimum of 3 months or until CSF becomes normal.
In endemic areas, neurobrucellosis should be considered among the differential diagnoses while evaluating patients with stroke, especially when there are associated constitutional symptoms like prolonged fever. A high index of suspicion is needed to ensure early diagnosis and treatment.
The authors would like to acknowledge the Infectious Diseases Fellowship Program and Internal Medicine Residency Program of Hamad Medical Corporation for scientific support.
The case was approved by the Medical Research Center at Hamad Medical Corporation. Written informed consent was given by the patient to publish his case information, images and details.
This study was funded by Qatar National Library.
The authors have no conflicts of interest to declare.

©2020 Varghese, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.