MOJ
eISSN: 2381-179X


Case Report Volume 2 Issue 3
Department of Neurosurgery, Neuroscience Center, USA
Correspondence: Andres M Alvarez-Pinzon, Department of Neurosurgery, Neuroscience Center, Larkin Community Hospital, USA
Received: December 13, 2015 | Published: June 2, 2015
Citation: Alvarez-Pinzon AM, Stein AA, Wolf AL, et al. Minimally invasive surgical treatment of intractable trigeminal neuralgia in multiple sclerosis. MOJ Clin Med Case Rep. 2015;2(3):71-73. DOI: 10.15406/mojcr.2015.02.00023
Background: Retrograssean balloon compression of the trigeminal nerve is a common treatment modality used for the treatment of trigeminal neuralgia in patients without multiple sclerosis (MS), but is not commonly used in patients diagnosed with MS, where the facial pain is a result of scar tissue or demyelinating plaques. Approximately 10 percent of patients with MS have a diagnosis of trigeminal neuralgia (TN). Most patients develop other symptoms of multiple sclerosis and optic neuritis before the facial pain and the diagnosis of MS is usually established before they develop chronic facial pain. These patients are more likely to develop the symptoms on both sides of the face than those without MS, but rarely anyone has both sides of the face are affected at the same time. This cases report an efficient method to treat an acute episode of intractable trigeminal neuralgia in multiple sclerosis patients.
Case description: We report the cases of two women with a primary diagnosis of MS that presented with secondary trigeminal neuralgia. The patients were 38 and 56years old. Patients presented to the ER with pain that was described as a “shooting” sensation in the V1-V2 and V3 distributions, with an intensity of 10/10, and not relieved by pharmacologic or Radiosurgical treatment. Both cases were treated by retrograssian balloon compression by neuro-navigation based on the difficulty to foramen ovale puncture.
Conclusion: The treatment of TN in patients with MS presents a dilemma. The difficulty of demyelinating disease is identifying the source of pain and finding the best treatment for the symptoms. This is the primary challenge for neurosurgeons in treating MS patients with atypical facial pain. Micro vascular decompression should not be considered as primary treatment of trigeminal neuralgia in this patient population, where the target plate and not the neurovascular conflict related trigeminal neuralgia. Stereotactic Radiosurgery can be a good treatment option, but there is a lack of published data to support the treatment in acute setting after failure of treatment by Radiosurgery. Retrograssean balloon compression by neuro-navigation could be a successfully rescue technique in acute complex trigeminal neuralgia in MS patient.
Keywords: percutaneous balloon compression, pain management, multiple sclerosis, trigeminal neuralgia
MS, multiple sclerosis; TN, trigeminal neuralgia; MRI, magnetic resonance imaging; PBC, percutaneous balloon compression; RFR, radio frequency rhizotomy; PRGR, percutaneous retrogasserian glycerol rhizolysis
Multiple sclerosis (MS) is a multifaceted disorder of the central nervous system that results in demyelination and axonal loss as well as inflammation. Affects 2.5million people worldwide.1 Pain is a common symptom, but was observed to be understated in MS public and is estimated in a range of 29 to 86 percent in this type of diagnosis. Pain in MS includes tonic spasms, Lhermitte’s sign, headache and trigeminal neuralgia.2 Trigeminal neuralgia is a representative source of extreme pain and debilitating symptom in patients with multiple sclerosis, and is known to be an early symptom of the disease. The Trigeminal neuralgia could be classified as an intermittent form of central neuropathic pain. The pain associated with trigeminal neuralgia hypothesized mechanism of paroxysmal high frequency generated by demyelination intra-axial and extra-axial of trigeminal primary afferent nerves.
The prevalence of TN in MS ranges from 1.9% to 6.3%. The clinical presentation are similar compared with idiopathic TN3 associated with the phenomenon of L’hermitte described as a transient, similar to electric shock paroxysmal discharge, usually caused by bending of the neck, to sit in the back neck and extends to the lower extremities. Although this phenomenon is not an exclusive symptom of MS. Facial pain in MS has been frequently reported by patients with MS as a shooting constant pain non-related to any patient action. The pain of neuralgia may often describe as throbbing, stabbing, shooting, beating, sudden and repetitive. Studies using Brain MRI shows demyelinating plaques of one or both sides of injury in the trigeminal branches V2 and V3 that produces high signal in the pons and brainstem nuclei. The treatment of TN associated of MS is a challenge. The management with medicine and continuous amount of anticonvulsant drugs used to treat TN makes the MS symptoms worse. Neurosurgery assessments are available for the treatment of TN with Radiosurgery percutaneous balloon compression. Reviewing the literature, treatment failures have been observed in MS patients, however retrograssean balloon compression have the highest rate of initial free pain response and a long duration of pain-free intervals comparing to other modalities.4,5
Case 1
A 38-year-old woman presented with symptoms of TN that began at the age of 34. At first, she presented with optic neuritis and intermittent jaw soreness. Within a period of 4 months her visual symptoms had resolved and her facial pain had progressed along the V1, V2 and V3 distributions of the trigeminal nerve on the right side of the face including (eyes, jaw, teeth and tongue). The patient underwent three dental procedures with no pain relief. Her facial pain was controlled for one year with carbamazepine 600mg daily and pregabalin 300mg daily, however the side effects limited the continued maintenance with this medicine. Gabapentin was also tried, but with poor response. Surgical options were considered. Percutaneous trigeminal ganglion balloon compression (PBC) was performed under neuronavigation as a salvation therapy for acute uncontrollable pain episodes. The patient was admitted to the hospital with acute, constant, and intense pain (Figure 1). Immediately after the procedure the patient experienced pain control. Pregabalin was stopped. After one year, the patient began to experience pain along the V2 distribution. Pain was not well controlled with carbamazepine 600mg a day. Another PBC was done to treat her right V2 pain. Patient pain was controlled.

Figure 1 Neuronavigation conducted for a balloon compression technique approaches to the foramen ovale for the management of trigeminal neuralgia increases goal visualization and potentially decrease the possibility of complications.
Case 2 A 56-year-old woman presents with TN symptoms since 46years of age. At first, she had an episode of right facial pain, intensity 9/10, radiated to her eye with spontaneous remission after 6months of treatment with carbamazepine. After 1year, a new onset facial pain started that affected the right side of his face, Radiosurgery gammaknife was performed with the resolution of 80% after 2months. After 1year, a new onset facial pain began to affect the right side of her face. Gamma Knife Radiosurgery was performed with an 80% resolution of pain after 2months. 1 year post-operatively, the patient experienced recurrent pain the territory supplied by V1 and V2 of the trigeminal nerve. The patient was diagnosed with secondary progressive MS with continuously progressive symptoms in the distributions of V1, V2 and V3. The patient was treated with carbamazepine and pregabalin until adverse reactions of the pharmacotherapy presented itself in the patient. At this point, further surgery was considered.
Patient presented to ER with a shooting, uncontrollable facial pain. Percutaneous balloon compression of the trigeminal ganglion was performed (Figure 2). After surgery, the patient had complete resolution of their pain, but later suffered a mild atypical facial pain 5/10 in the distribution of the V3. She was placed back on medical therapy with oxcarbazepine and pregabalin. Eight months post-balloon compression, the patient had gradually improved pain control.
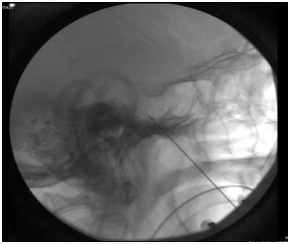
Figure 2a Preoperatively, a skull computed tomography (CT) scan is achieved and the acquired images are introduced into the navigation system. Intraoperatively, a precise reference frame is strapped firmly to the patient’s forehead. The preliminary CT images are registered in the system, and cannulation is performed under the guidance of the navigation system.
TN can be categorized as idiopathic or symptomatic by etiology. In idiopathic or essential TN etiology is unknown. Patients describe a short, intermittent, and sturdy shock affecting one or more division of the trigeminal nerve. The posterior fossa tumors and multiple sclerosis are the most common cause of secondary TN. According to Buerchiel, recently a new classification of facial pain syndromes has been proposed that includes seven categories based on the history and quality of patient pain. The idiopathic TN is divided into type 1 (spontaneous and episodic) and type 2 (constant pain).6 Facial pain syndromes are subdivided into the trigeminal neuropathic pain resulting from unintentional injuries in the trigeminal nerve trauma or surgery; differentiation trigeminal pain resulting from nerve injury or peripheral nerve ablation, gangliolysis or rhizotomy in a deliberate attempt to try either TN or other facial pain. The last category, atypical facial pain, is synonymous with high somatoform pain disorder.4,7
In MS, demyelination extends along the proximal portion of the trigeminal nerve root and in some cases, to its junction with the peripheral nervous system. There were also reports of some other findings include: astrocyte processes, which are generally more numerous and widely distributed in the regions of demyelination. PBC produces acceptable pain relief and is associated with a lower incidence of complications compared with RFR and PRGR, although transient masseter weakness can be expected in most cases during the immediate postoperative period.1,7 The shape of the balloon can have an important role in the clinical outcomes of PBC and pear shaped balloons are associated with superior pain relief compared to other forms. Compared to open surgery and percutaneous techniques, the SRS is less invasive, accurate and has a small number of postoperative complications. The disadvantages of radiosurgery however, are the high recurrence rate and latency to provide pain relief after radiation treatment as described in the current cases. We presume that the SRS could be a good alternative in patients with multiple sclerosis who have chronic central pain first treated with Gamma Knife and present acute recurrent pain.
The pain caused by MS and resistant to drugs and Gamma Knife is a challenge. The percutaneous technique is a fair behavior in patients with MS. Although MVD is recognized as the “gold standard” treatment for patients with TN, there is no role for this surgical approach in patients with MS. SRS with neuro-navigation offers a minimally invasive successfully option for the treatment of TN in patients with recurrent symptoms. Is necessary to conduct randomized controlled clinical trials to evaluate the long term success rate of this technique in patients with secondary progressive MS. and TN.
None.
The author declares no conflict of interest.

©2015 Alvarez-Pinzon, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.