MOJ
eISSN: 2381-179X


Case Report Volume 3 Issue 2
Department of Neurosurgical Oncology, Miami Neuroscience Center at Larkin Community Hospital, USA
Correspondence: Andres M Alvarez-Pinzon, Department of Neurosurgical Oncology, Miami Neuroscience Center at Larkin Community Hospital, 6129 SW 70th Street South Miami, Florida 33143, USA
Received: July 14, 2015 | Published: November 16, 2015
Citation: Alvarez-Pinzon AM, Wolf AL, Tydir MS-III JAE, et al. Minimally invasive endoscopic endonasal transphenoid approach for resection of pituitary macroadenoma: case report and literature review. MOJ Clin Med Case Rep. 2015;3(2):218-220. DOI: 10.15406/mojcr.2015.03.00062
Background: Endoscopic endonasal transsphenoidal resection of pituitary adenomas is a common treatment modality used for the treatment of non-functioning pituitary adenomas due to its minimally invasive approach, excellent result yields and limited complications. Other treatment options, such as Gamma Knife radiosurgery (GKRS) can be considered as a suitable primary approach, however, GKRS is associated with a higher rate of treatment failure and tumor recurrence. Here we describe the case of recurrent pituitary macroadenoma post-radiosurgery treatment with Gamma Knife that was then treated via surgical resection with an endonasal endoscopic transsphenoidal approach.
Case description: We report the case of an 82year-old male with a primary diagnosis of non-functioning pituitary macroadenoma. The patient presented with an initial complaint of an unrelated syncopal episode. During workup an incidental suprasellar mass was found and determined to be a nonfunctioning pituitary macroadenoma. The patient was initially treated with radiosurgery by Gamma Knife, however, 3 months later presented with an acute episode of headaches, nausea and vomiting, altered mental status, diplopia and a bitemporal hemianopsia. Work up and imaging revealed panhypopituitarism and a suprasellar mass. An endonasal endoscopic transsphenoidal approach was undertaken for resection. Conclusion: Various treatment modalities are available for the management of pituitary adenomas. Gamma Knife radiosurgery is a safe and effective treatment as a primary therapy as well as a co-adjuvant to surgical resection. However, there exists a probability of treatment failure and tumor recurrence with GKRS as well as attention should be paid to the adverse affects that can develop post-radiosurgery. Endoscopic transsphenoidal resection is a minimally invasive surgical procedure that can safely be employed as a treatment option for primary and recurrent pituitary macroadenomas.
Keywords: pituitary tumor, pituitary adenoma, macroadenoma, transsphenoidal, hypopituitarism, gamma knife, radiosurgery, endoscopic, GKRS, treatment failure, endoscopic transsphenoidal, radiotherapy, endonasal, hemianopsia, panhypopituitarism, craniotomy, pituitary macroadenoma
Fibro-osseous lesions are characterized mainly by replacement of normal bony architecture with fibrous collagenous connective tissue that contains varying amounts of mineralized substances, which may be bony or cementum like in appearance. The lesion, termed as cemento-ossifying fibroma, has been regarded as an osteogenic neoplasm. The fibrous dysplasia in which the normal bone structure is replaced by collagenous tissue is normally regarded as non-neoplastic. The cemento-ossifying fibromas (COF), in some cases has been demarcated into ossifying and cementifying fibromas, based on the tissue content of encapsulated neoplasms appearing as bone and/or cementum.1 COF is most commonly diagnosed in the third and fourth decades of age and possesses a clear-cut female predilection (Female: Male ratio being 4:1).1–6 The tumor appears as intrabony slow growing asymptomatic mass causing expansion of cortical plates, displacement of root and facial deformity. Radiologically, COF appears radiolucent with varying degree of radio opacity depending upon the degree of calcification. Histopathological picture reveals fibro-collagenous connective tissue with proliferating plump fibroblast cell and osteoid/cementoid mass. The management comprises of surgical resection involving enucleation via bone bed curettage. Due to significant overlap of clinical, radiological and histopathological criteria, sub-classification of fibro-osseous lesions are difficult which often leads to the confusion in diagnosis and therefore management. The present article reports one COF case involving the left mandible and with its clinical, radiological and histological findings.
An 82-year-old male presented to an outside facility with an unrelated syncopal episode. Patient workup revealed an incidental finding of a 1.6cmx2.2cm suprasellar mass on MRI. Further assessment concluded that it was a non-secretory pituitary adenoma (Figure 1). All treatment options were then carefully reviewed and discussed with the patient and his family. A full review of the risks, benefits and alternatives were discussed with the family for options of observation, gamma knife radiosurgery and endoscopic transsphenoidal resection of the macroadenoma. The family, taking into consideration with the patient’s age subsequently chose radiotherapy. The patient underwent gamma knife radiosurgery with stereotactic localization. (Insert gamma knife radiosurgery protocol). A 14Gy was delivered to the 50% isodose line with a region measuring 2.6cc giving complete coverage but maintaining dose to the brain stem to less than 6Gy; less than 4Gy to the optic nerve and optic chiasm; and less than 50cGy to the bilateral lens.
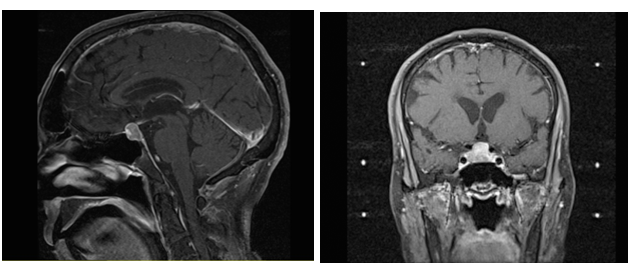
Figure 1 A) Pre-Gamma Knife T1 Weighed MRI (Sagittal View); B) Pre-Gamma Knife T1 Weighed MRI (Coronal View).
Three months later the patient presented acutely with complaints of headache, nausea/vomiting, altered mental status and diplopia. Physical examination revealed bitemporalhemianopsia and CNIII palsy. Laboratory and imaging workup revealed panhypopituitarism and a 1.7cmx1.9cm contrast enhancing surpasellar hemorrhagic mass impinging on the optic chiasm with extension into the cavernous sinuses R>L (Figure 2). Treatment options were discussed and the patient chose to undergo surgery for resection of the macroadenoma. The patient successively underwent Endoscopic Endonasal Transphenoid Resection of the Pituitary Adenoma (Insert surgical protocol) (Figure 3). Post-operatively, the patient had no major complications or focal motor or sensory neurological deficits. Patient noticed immediate improvement in his peripheral vision with marked resolution of CN III palsy several days post-op. Patient had no complications, clear rhinorrhea, or infection. Patient was placed on hormone replacement therapy (with Hydrocortisone, Synthroid and Vasopressin) due to his panhypopituitarism from pituitary apoplexy.
With the various subtypes of pituitary adenomas, many factors must be taken into consideration when determining the best treatment modality. Multifactorial elements include tumor size, location, hormone production, neoadjuvant, radiation or surgical treatments history, patient’s health, applicable comorbidities and inevitably patient preferences of the treatment options. Treatment options that are widely available include medical therapy (if hormone producing), microscopic or endoscopic surgical resection, gamma knife radiosurgery, radiation therapy, or observation depending on the tumor and clinical status of the patient.2 Here we focus on Gamma Knife Radiotherapy and Endoscopic Endonasal techniques.
Radiotherapy has its benefits in that it is a reliable way of gaining local control for radiographically progressing pituitary adenomas.3 Gamma Knife also has better long-term effects as compared with external beam radiation therapy. This is due to the fact that it allows radiation to be largely confined to the target with minimal radiation reaches the surrounding brain.3 However, the minimum distance required between the irradiated target and the optic pathway should be 2mm for secreting adenomas. In cases of non-secretory adenomas this distance is even lower.4 This is an important factor to consider in regards to the recurrence of pituitary macroadenoma in this patient as a factor.
The most common reported complication after radiosurgery is delayed hypopituitarism followed by cranial neuropathies.2 Direct complications include radiation necrosis, which is a radiation-induced damage to the tissues. In addition, complications specific to certain diseases and their locations do occur. For the treatment of pituitary adenomas, specific radiotherapy complications include pituitary failure. The most common precipitating factors for pituitary apoplexy include pituitary stimulation, surgery (particularly coronary artery surgery) and coagulopathy.5 A risk of inducing neoplasia from irradiation of normal tissue or tumor also exists.6 This could be a causative factor in the recurrence of pituitary macroadenoma seen.
The endoscopic endonasal technique brings advantages to not only to the surgeon but to the patient as well. Patients treated with the endoscopic endonasal approach have been reported to have less nasal traumatism, no nasal packing, less post-op pain, quick recovery and shorter hospital stay.7,8 This is minimally invasive in comparison to the other available surgical approaches of pituitary macroadenoma, which include neuroendoscopy and craniotomy. Benefits of endoscopic endonasal technique to the surgeon include an enhanced visualization of the surgical field of the relevant anatomy, enlarged working angle with a panoramic view and smoothing of interdisciplinary cooperation. From the peer-reviewed literature over the last 15years, the endoscopic endonasal technique has provided an increase in the opportunities, knowledge and medical activity from these surgeries.7–9 Lastly, advantages can also be seen at the level of the facility with shorter post-op hospital stay allowing for an increase in the number of cases.8
A retrospective study performed on 32patients with pituitary adenomas examined efficacy, safety and outcomes of the endoscopic endonasal transsphenoidal approach.10 Total-subtotal tumor resection was achieved in 75% of the microadenomas (<10mm) and 45% and macroadenomas (>10mm). Post-op complications of the patients included CSF leak (3patients) and transient diabetes insipidus (2patients).10 The endoscopic endonasal approach has been reported to have similar outcomes as compared to major microsurgical series in regards to removal of the mass, relief of clinical symptoms, cure of the underlying disease and complication rate. However, patient compliance is by far better in endoscopic endonasal cases.9 Overall, endopscopic transsphenoidal surgery is an effective and safe treatment for most patients with pituitary adenoma and could be considered the first-choice therapy in these patients.10
Gamma knife Radiotherapy can be a suitable primary approach for patients with pituitary macroadenoma. It is a safe and effective treatment option especially for patients with advanced age or comorbidity. However, a certain probability exists for failure of treatment, as seen with the gamma knife technique discussed in this case report. Attention should be paid to the late adverse radiation effects such as hypopituitarism, optic neuropathy and radiation-induced neoplasms, which cannot be excluded.11 Considering all surgical methods available for the resection of pituitary macroadenoma, the endoscopic endonasal approach is minimally invasive compared to the neuroendoscopic and more invasive approaches such as craniotomy. Treatment of macroadenomas is overall complex, since macroadenomas are more likely to have greater involvement such as suprasellar and cavernous sinus extension.10 Complications to the Transsphenoidal approach do exist, which include CSF leak, requiring sellar repair. Other complications include residual mass, blindness, bleeding, infection and the possibility of developing panhypopitutarism. However, with advances in both technology and surgical technique using the endonasal approach treatment for pituitary adenoma can be both safe and effective, while also giving the patient the chance of complete resolution of the macroadenoma.
None.
The author declares no conflict of interest.

©2015 Alvarez-Pinzon, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.