MOJ
eISSN: 2381-179X


Case Report Volume 14 Issue 2
Department of Neurosurgery, National Hospital of Niamey, Niger
Correspondence: Ousmane Issoufou Hamma, Department of Neurosurgery, National Hospital of Niamey, Niamey, Niger
Received: April 13, 2024 | Published: May 1, 2024
Citation: Hamma OI. Management of giant posterior meningocele lombosacral: about three case report. MOJ Clin Med Case Rep. 2024;14(2):44-46. DOI: 10.15406/mojcr.2024.14.00460
Meningoceles are one of the most common malformations of the nervous system, accounting for around 10% of all neural tube defects. It is a complex congenital malformation of the spine, characterized by protrusions or expansions of one or more layers of the thecal sac through a canal or foramen of the spine in which there is a defect. Children usually show no neurological signs at birth, but surgical exploration is warranted to prevent future neurological deterioration. These malformations are frequently found in a posterior position, with dysraphic vertebrae in the lumbosacral region. Their management is associated with multiple challenges in our regions, including difficulties with perioperative and anesthetic care. We report these to highlight and share our experiences in the perioperative management of meningocele.
Keywords: Meningocele, neural tube defect, spinal dysraphisms, spinal cord malformation, management
Meningoceles are one of the most common malformations associated with the central nervous system, accounting for around 10% of all patients with spina bifida.1,2 It is a complex congenital malformation of the spinal column, characterized by protrusions or expansions of one or more layers of the thecal sac through a canal or foramen of the spine in which there is a defect.3 Children are usually born without neurological deficits, but surgical exploration is warranted to prevent future neurological deterioration.3 These malformations are frequently found in a posterior position, with the dysraphic vertebrae above the thoracolumbar region.1 Their management is associated with multiple challenges in our regions, including difficulties with perioperative and anesthetic care. We report these to highlight and share our lived experiences during the perioperative management of giant spinal meningocele with impending rupture requiring surgical excision and repair.
Case 1
4-month-old male infant, born at term by caesarean section at 3.6 kg, eutrophic with a large lumbosacral mass, second child of consanguineous parents. He was the second child of consanguineous parents, the result of a poorly monitored mono-fetal pregnancy with no notable antecedents. He was referred to us by a peripheral center for management of spina bifida. On admission, he was conscious with normal general condition, normal symmetrical pupils and no neurological deficit. The swelling had been progressively increasing in size since birth and currently measured 17 cm x 15.5 cm x 10 cm; it was globular, cystic, fluctuating, painless, and threatened to rupture at any time; the skin covering the mass was normal and shiny (Figure 1). The baby's respiratory, digestive and cardiovascular examinations were unremarkable. The preoperative CT scan of the spine showed a posterior arch anomaly at the level of vertebrae L4 to S1, as well as a voluminous herniation of the cerebrospinal fluid-filled meninges (Figure 2). The diagnosis was lumbosacral meningocele with imminent unruptured rupture. Preoperative haemotological and biochemical findings were within normal limits. Surgical excision and repair were indicated, he was prepared for surgical cure and taken to the operating room. In the operating room, after general anesthesia, an orange-peel incision was made. During surgical cure, the residual neural plate was exposed and placed in the sheath (Figure 3). The post-operative course was complicated by an infection of the surgical site, but thanks to appropriate management the evolution was favorable.
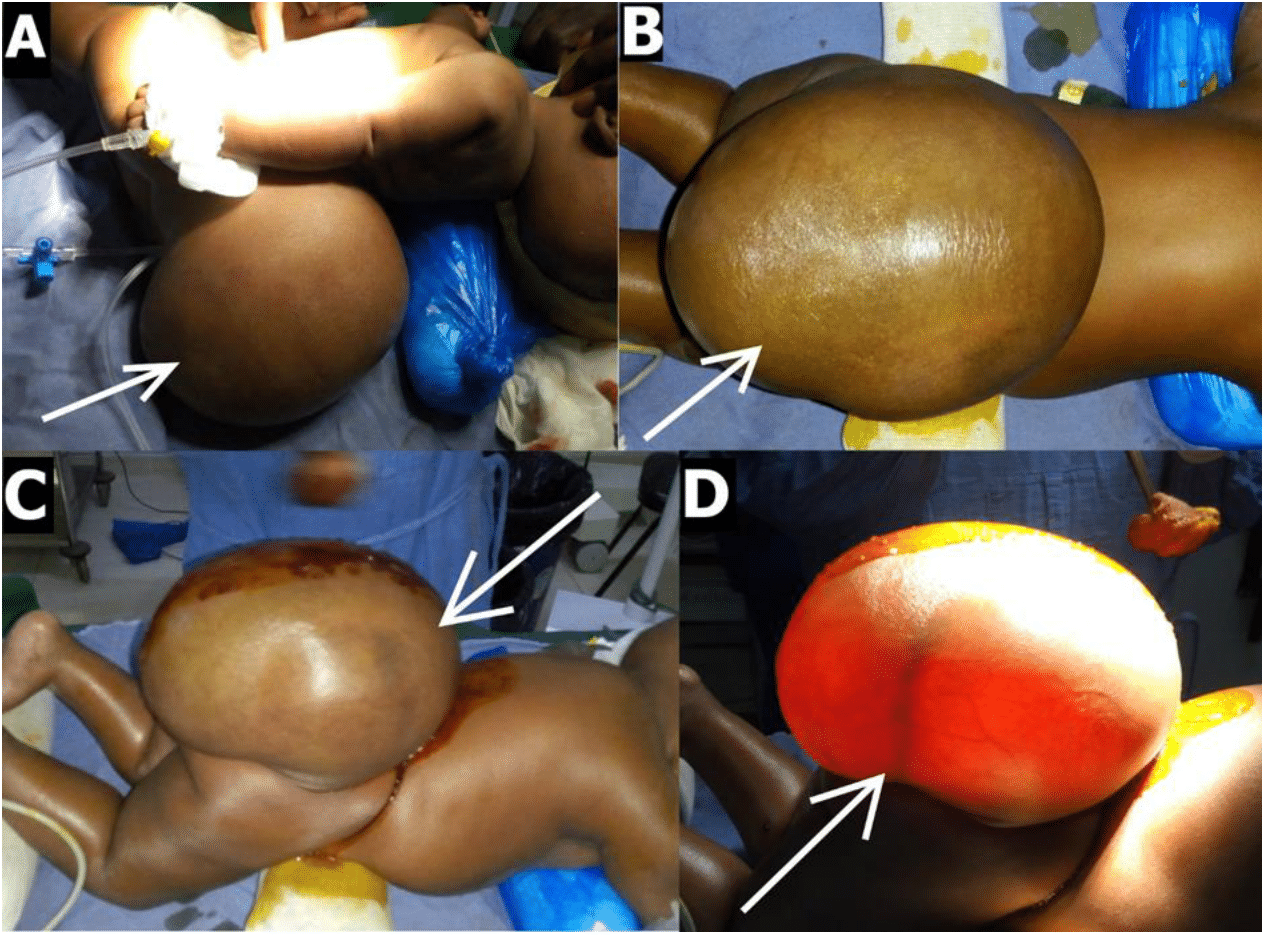
Figure 1 Operating room images of case 1, showing: A,B,C,D) giant lumbosacral meningocele presenting as a large, globular, cystic, fluctuating, translucent mass (white arrows).
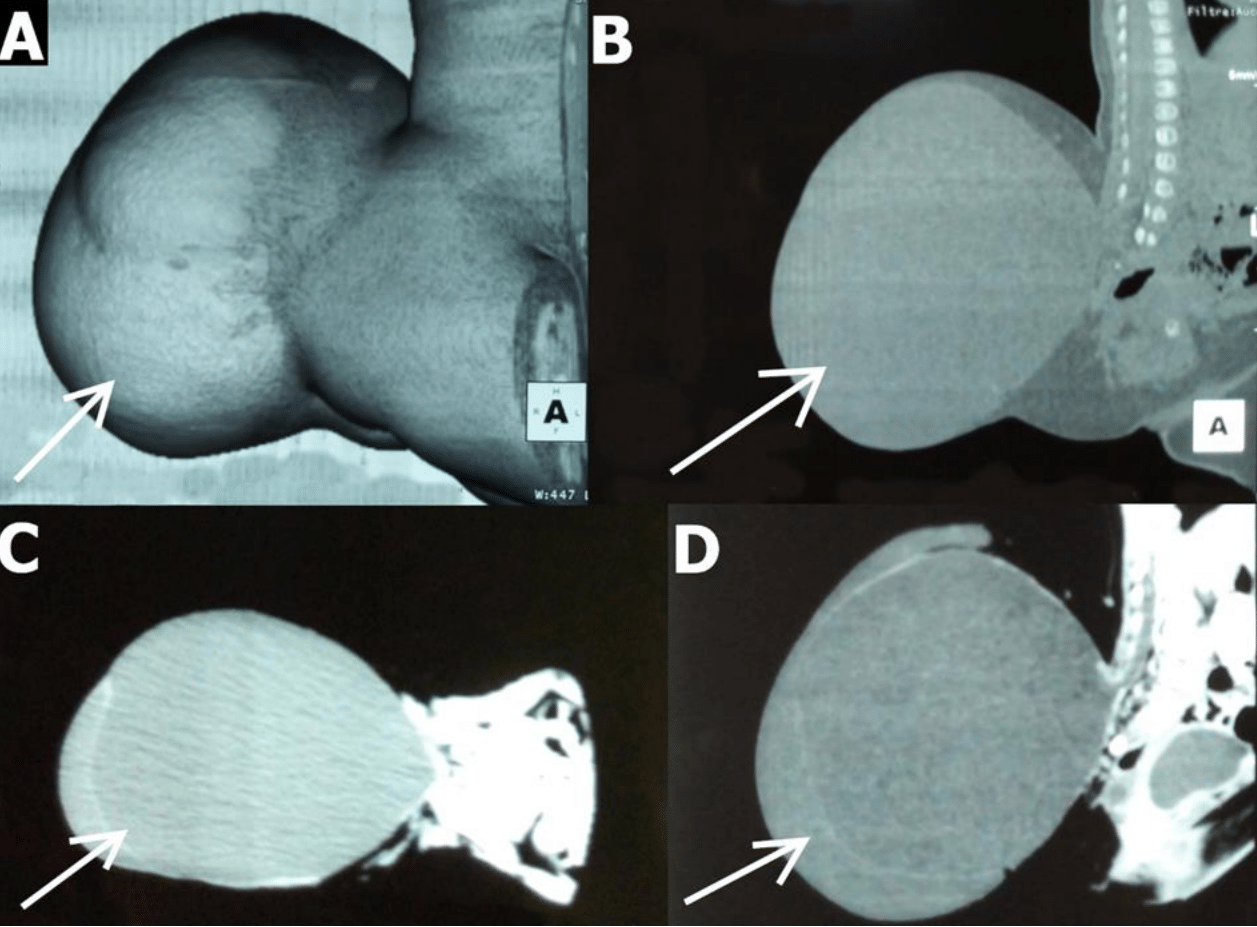
Figure 2 Preoperative CT images of case 1, showing : A,B,C,D) a posterior arch anomaly at the level of vertebrae L4 to S1, and a large herniated meninges filled with cerebrospinal fluid (white arrows).
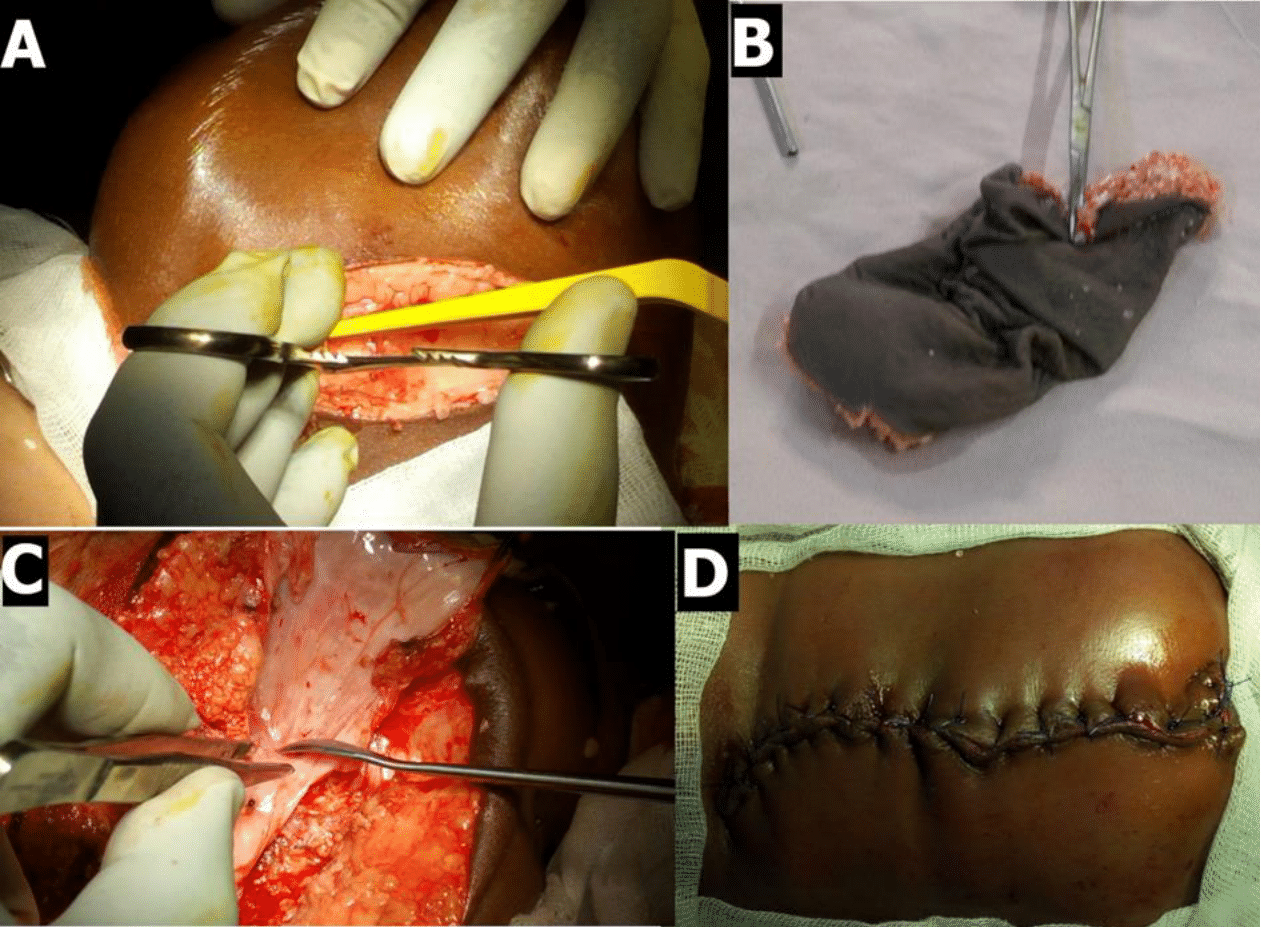
Figure 3 Intraoperative images of case 1, showing: A,B,C,D) the various stages of surgical excision followed by repair.
Case 2
14-month-old male infant, born at term vaginally, eutrophic with a large lumbosacral mass and lower limb deficits, first child of consanguineous parents. He was the first child of consanguineous parents, the result of a poorly monitored mono-fetal pregnancy with no notable antecedents. He was referred to us by a peripheral center for management of spina bifida. On admission, he was conscious and in good general condition, with normal symmetrical pupils, no paraplegia and no sphincter control. The swelling had been progressively increasing in size since birth and currently measured 12 cm x 8 cm x 6 cm; it was globular, cystic, fluctuating, painless, the skin overlying the mass was normal but with poorly epidermised areas (Figure 4). The baby's respiratory, digestive and cardiovascular examinations were unremarkable. The preoperative spine scan showed a lumbosacral meningocele. Surgical excision and repair were indicated, and he was prepared for surgical cure and taken to the operating room. In the operating room, there were intubation difficulties. Post-operative management was straightforward and the evolution was favorable.
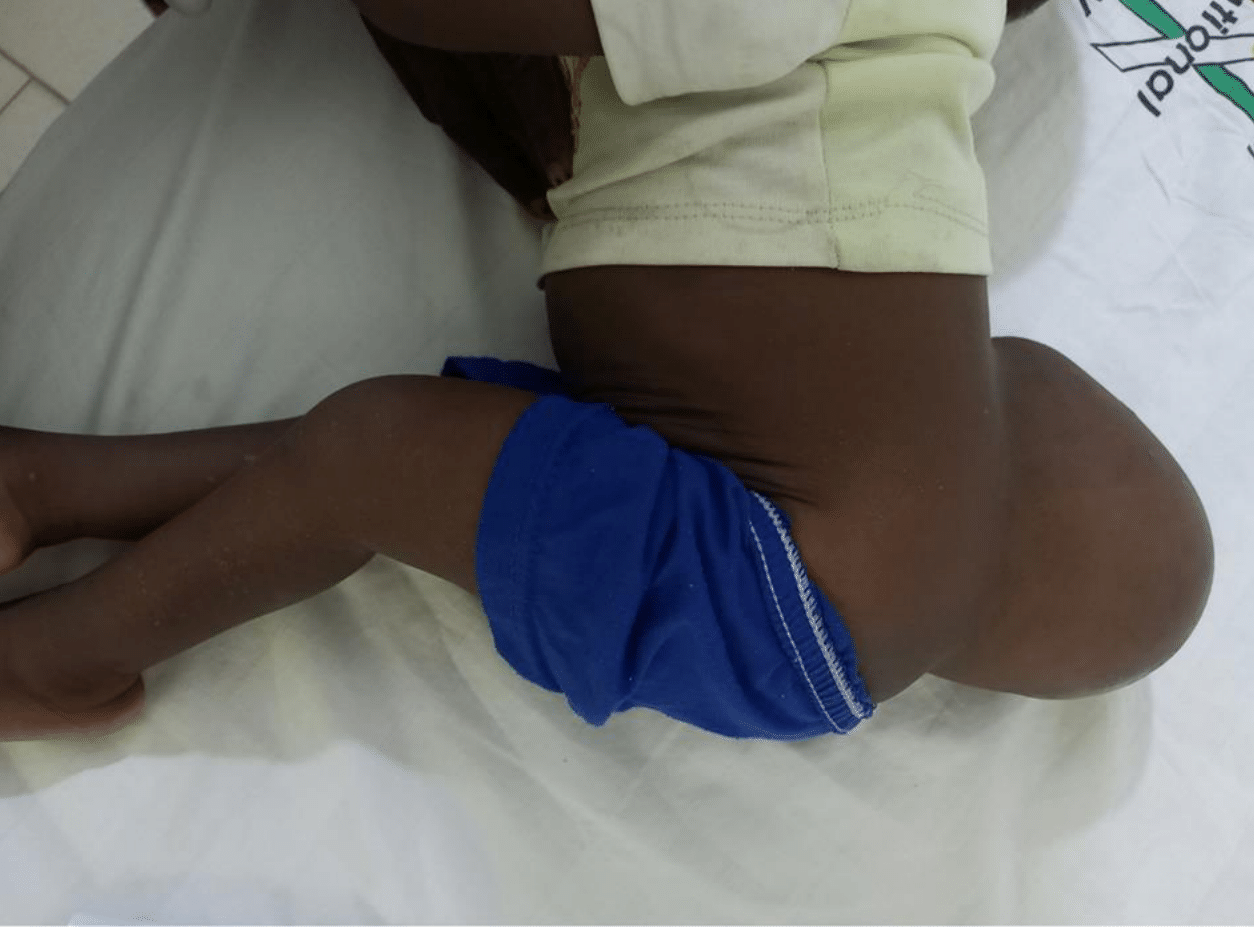
Figure 4 Image of case 2, showing giant lumboscral meningocele presenting as a large, globular, cystic, fluctuating mass.
Case 3
3-month-old male infant, born at term with a large lumbosacral mass, first child of non-consanguineous parents. He was born of a well-monitored pregnancy with no notable antecedents. He was referred to us by a peripheral center for management of spina bifida. On admission, he was conscious with normal general condition, normal symmetrical pupils and no neurological deficit. The swelling had been progressively increasing in size since birth and currently measured 12 cm x 10 cm x 7 cm, was globular, cystic, fluctuating, painless, and the skin overlying the mass was normal (Figure 5). The preoperative CT scan showed a lumbosacral meningocele. Surgical excision and repair was indicated, he was prepared for surgical cure and taken to the operating theatre. Surgery was unremarkable. The postoperative course was complicated by a CSF leak requiring revision surgery, but the evolution was favorable.
Neural tube defects constitute a very heterogeneous group of pathologies affecting the encephalon and spinal column, unified by their clinical signs of spinal cord dysfunction and distinguished by their mechanisms of mental development and the involvement of different tissue types.4 From around 18 days' gestation, the central nervous system is a flat sheet of cells (the neural plate) which then undergoes remarkable morphological changes at around 28 days' gestation to form a tube of neural tissue surrounding the fluid space which eventually becomes the cerebral ventricles and spinal canal.4 Meningoceles are the most common neural tube defects, accounting for around 10% of all spina bifida patients. They are projections or expansions of one or more layers of the thecal sac through a canal or foramen of the spine in which there is a defect.1 These malformations are characterized by a bulging of the dura mater due to the bony defect, and a cystic malformation contains only cerebrospinal fluid with no nerve tissue. If the cystic malformation protrudes dorsally from the spinal canal, we speak of a posterior meningocele. If the cystic malformation protrudes ventrally from the spinal canal, it's called an anterior meningocele. Early authors believed that meningocele usually presented no neurological deficit.2
However, a growing number of clinical studies show that simple meningocele is associated with a very high rate of attached spinal cord, leading to progressive neurological signs with age. It should be noted that during the last four years of continuous observation, Bao et al.2 found that in 37 cases out of 38 (97%) a simple meningocele was associated with other spinal cord malformations, such as a tight terminal filum, an arachnoid cyst, an epidermoid cyst, an attached spinal cord due to fibrous bands, an adhesion between the dura mater and the spinal cord or ponytail, etc. It should be noted that certain spinal cord malformations are not associated with a simple meningocele. it should be noted that certain giant and limited dorsal neural tube defects such as dorsal myeloschisis, simple dorsal meningoceles... may be associated with a normal functional prognosis.5
Their management may require paraclinical examinations, as these malformations may simulate other spinal pathologies; Francis et al reported a case of sacrococcygeal meningocele simulating a sacrococcygeal teratoma.6 However, around 60% of these children may have associated intracranial and/or extra-SNC malformations affecting perioperative management, such as hydrocephalus, microcephaly, micrognathia, Chiari malformation, pulmonary hypoplasia and renal agenesis.7 Early closure of the meningocele, usually within the first week of life, is recommended to reduce infectious agent contamination of the exposed spinal cord after pouch rupture, which is the leading cause of death in this population during the neonatal period. Anesthesia in prone children, particularly infants, presents the highest risk of complications. Safe anesthetic management depends on a full appreciation of the physiological, anatomical and pharmacological characteristics of infants.3 Anesthetic management of meingoceles is associated with multiple challenges, including difficulties securing the airway, prone position, blood loss, electrolyte imbalance, hypothermia, cardiorespiratory disorders and perioperative care. The main objectives are to prevent hemodynamic and ventilatory fluctuations, and excessive pressure on the bag to avoid premature rupture and manage any difficulty during intraoperative care.7 Among the complications during intraoperative care, surgical site infections, cerebrospinal fluid leaks and secondary neurological deficits are the most serious to manage.
Giant posterior lumbosacral meningoceles are still common in our region, as preventive measures such as folic acid supplementation and the avoidance of consanguineous marriages are not yet firmly established. However, difficulties during perioperative care are linked to the country's limited resources.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The author declares that there is no conflicts of interest.
The study has been approved by the Ethics Committee of the National Hospital of Niamey.

©2024 Hamma. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.