MOJ
eISSN: 2381-179X


Case Report Volume 9 Issue 1
1Dept of General Medicine, VSS Institute of Medical Sciences and Research, India
2Junior Resident, Dept Of General Medicine, VIMSAR, India
3Dept of General Medicine, VIMSAR, India
Correspondence: Manoj Kumar Mohapatra, Prof. General Medicine, VSSIMSAR, India
Received: December 17, 2018 | Published: January 30, 2019
Citation: Bariha PK, Sahu AK, Kumar SR, et al. Intramedullary tuberculoma of spinal cord, in association with TB intestine and pleural effusion responded to antitubercular therapy: a case report. MOJ Clin Med Case Rep. 2019;9(1):17-19. DOI: 10.15406/mojcr.2019.09.00293
Background Spinal intramedullary tuberculoma is not only a rare cause of spinal cord compression but also of CNS tuberculosis. We report a case of intramedullary spinal cord tuberculoma associated with tuberculosis of large intestine, anal fistula, and pleura as well. The diagnosis was made clinically as well as radiologically and confirmed by histopathology.
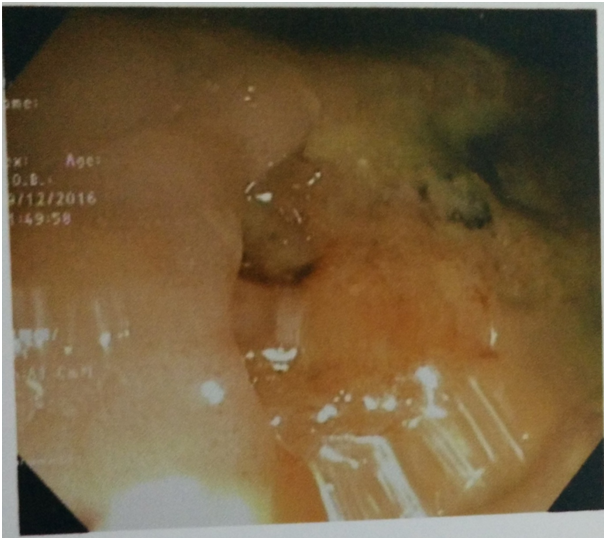
Case description The patient was a 48-year-old male with a history of early bowel and bladder involvement followed by bleeding per rectum and progressive paraparesis. MRI showed ring enhancement of the intramedullary thoracic lesion with perifocal edema. Colonoscopy showing a large tubercular ulcer in the lower rectum. Patient was treated with anti-tubercular therapy with clinical outcome.
Conclusion This case showed that intramedullary spinal tuberculoma is a rare of the spinal cord compression that responded to antitubercular drugs.
Tuberculosis of central nervous system is rare with an incidence of 0.5% to 2% among patients with systemic tuberculosis(TB)of which majority areintracranial.1 Intradural and intramedullary spinal tuberculoma comprises only a small percentage of cases. No evidence of active or distant tubercular disease was found in 38% of cases of intracranial tuberculosis.2 The first report of intramedullary spinal tuberculoma(IMT) was given by Albercrombie in 1828.3 It is usually found within age range of 18 to 45 years; however, it was also reported at the age of 4 years.4 Here we report a rare case of intramedullary spinal tuberculoma with evidence of distant tuberculosis as tubercular rectal ulcer, multiple anal fistula, tubercular pleural effusion with recovery following anti-tubercular therapy.
A 48 year old male presented with complains of hesitancy and sense of incomplete voiding for 8 months, dull aching upper back pain for 3 months and bleeding per rectum associated with multiple painful discharging sinuses in the perianal area for 2 months. Then the patient developed weakness of right lower limb with sense of heaviness for 2 months followed by weakness of left lower limb for 12 days with history of intermittent low grade fever with evening rise of temperature and night sweating and without any history of root pain.
On examination there was right inguinal lymphadenopathy. Higher mental functions and cranial nerves were normal. There is hypotonia of both the lower limbs and diminished power around hip(2/5), knee, and ankle joint(3/5), exaggerated knee and ankle jerk bilaterally and bilateral plantar extensor with absence of abdominal and cremasteric reflex. There was diminution of primary modalities of sensation below T6 with sacral sparing. On examination of respiratory system, there was left sided pleural effusion as evidenced clinically by stoney dull note with decreased vocal fremitus, vocal resonance and absence of breath sound in left infra-axillary and infra-scapular area. On per rectal examination, there are multiple external openings in perianal area, tender on palpation and multiple internal openings of fistula posteriorly on digital rectal examination. A provisional diagnosis of intramedullary thoracic compressive myelopathy with the lesion at the level of T6 spinal cord segment with perianal fistula and left sided pleural effusion was made and patient was investigated accordingly.
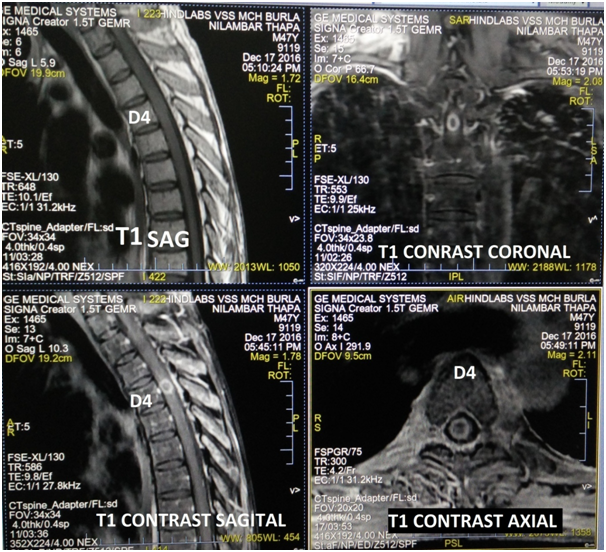
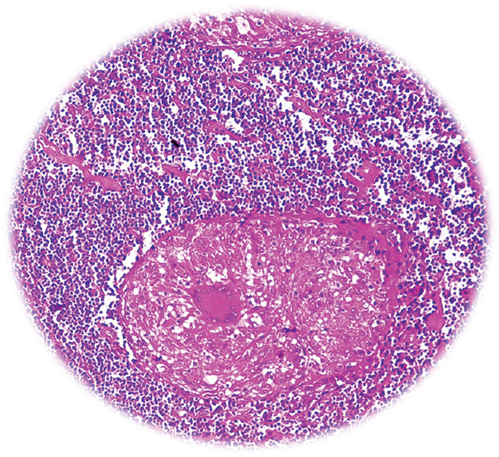
The investigations showed Hb-12.1gm/dl, ESR-45mm 1st hour, total leucocyte count-8700/mm3, differential leukocyte count: neutrophil(63%), lymphocytes(27%), eosinophils(5%), monocytes(4%), and basophils(1%). Biochemical investigations showed Fasting blood glucose-98.0mg/dl, blood urea-30.8mg/dl, serum creatinine-1.1mg/dl, serum bilirubin-0.8mg/dl, AST-34.0 IU/L, ALT-32.3IU/L, Alkaline phosphatase-100.8IU/L. Viral markers for HIV, HBSAg, and HCV was found to be negative. Radiography of Chest showed left sided pleural effusion. Radiography of thoracolumbar spine did not show any abnormality. Fistulo gram delineated the tract which was directed upwards posteromedialy. Fine needle aspiration cytology (FNAC) of right inguinal lymph node showed granular necrotic material with few lymphocytes highly suspicious of tuberculosis. MRI of thoracic spine (T2WI) showed a nodular hyperintense intramedullary lesion at T4 vertebral segment with surrounding hyperintense edema extending from T2to T6 vertebral level (Figure 1). With T1 contrast isointense lesion at D4 vertebral segment showed thick ring enhancement. Colonoscopy also showed a large ulcer in the lower part of rectum suggestive of Tuberculosis (Figure 2). The histology of biopsy material taken from perianal lesion showed caseating necrosis, epithelioid cells with Langhan’s type multinucleated giant cells suggestive of Tuberculosis (Figure 3).
A diagnosis of intramedullary spinal tuberculoma with perianal fistula and tubercular ulcer of lower rectum with left sided tubercular pleural effusion was made. Patient was treated with antitubercular therapy(HRZE+HR) and steroid (prednisolone 60mg for 2 months with gradual tapering over 1 month).His lower limb weakness improved over a period of 2 months. Patient was able to walk without support with recovery of perianal fistula and rectal ulcer.
From India, Sharma and Gupta have reported 10 and 8 cases of IMT, respectively, and they also discussed the treatment aspects of IMT5,6.
Tuberculomas involving the CNS are not uncommon in developing countries. Most of these lesions are intracranial with the ratio of cranial and spinal lesions averaging 30:1.5 Though these lesions are seen at any level of cord the thoracic cord is the most commonly involved segment followed by cervical, cervicodorsal and dorsolumbar lesions.6 Spinal TB can present in various forms, which includes pottsspine(64%), arachnoiditis(20%), intramedullary involvement(8%) and intradural extramedullary in 8%.7,8 The various types of intramedullary tuberculous lesions include tuberculoma, spinal cord edema and cavitation.9 Intramedullary spinal cord tuberculoma is a rare form of CNS TB and an uncommon cause of spinal cord compression.
Clinically, patients with intramedullary tuberculomas present with signs and symptoms depending on the location of tuberculoma in the spinal cord.5–8 Our case presented with early bladder bowel dysfunction followed by parasthesia and progressive lower limb weakness with a definite sensory level associated with multiple foci of tuberculosis as left pleural effusion, rectal ulcer, perianal fistula. MRI is the most accurate modality of investigation. T2weighted MRI showing a nodular hypointense intramedullary lesion at t4 vertebral segment with surrounding hyperintense edema extending from T2 to T6 vertebral level. T1 weighted MRI with contrast showing isointense lesion with thick ring enhancement. Radiologically the lesions that required to be differentiated from intramedullary tuberculomas include neoplastic (astrocytoma, ependymoma, haemangioblastoma, metastasis lymphoma), inflammatory, demyelinating (multiple sclerosis), vascular (malformations, infarctions) and granulomatouslesions (syphilis, pyogenic, mycotic, parasitic).
In the present case, evidences of tuberculosis was found in other sites except tuberculoma, because surgery and biopsy was not done and the patient responded to antitubercular drug. Though surgery is the treatment of choice in compressive myelopathy, IMT is a clinical entity that can respond to antitubercular drugs without surgical intervention. Some reports showed surgical removal with antitubercular drugs.5–8 In those cases, lack of tissue diagnosis was the cause of surgery. In our case as tuberculosis was diagnosed from other sites, ITM was logically thought to be due to same disease and response to antitubercular drugs was encouraging. Hence, in intra spinal tumour, investiagations should be done to exclude tuberculosis so that surgery can be avoided in such cases. Treatment of intramedullary spinal tuberculoma could be medical, surgical or both. Antitubercular therapy should be given for 9-12 months(at least 10 months)along with steroid.10 However, microsurgical technique has been advised when severe compression of cord parenchyma is evident, diagnosis is uncertain and there is a clinical deterioration despite adequate antitubercular drug therapy.11
The present case is a rare case of extra pulmonary tuberculosis of multiple sites that include large intestine, multiple fistula, pleural effusion, and intraspinal tuberculoma. Intramedullary spinal tuberculoma, although a rare entity must be considered in the differential diagnosis of spinal cord tumours to avoid unnecessary surgery.
None.
The author declares no conflicts of interest.

©2019 Bariha, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.