MOJ
eISSN: 2381-179X


Case Report Volume 13 Issue 2
1Department of Innovative Endovascular Methods for the Prevention and Treatment of Cardiovascular Diseases, National Medical Research Center for Therapy and Preventive Medicine, Russia
2Department of Secondary Prevention of Chronic Noncommunicable Diseases, National Medical Research Center for Therapy and Preventive Medicine, Russia
3Department of Innovative Endovascular Methods for the Prevention and Treatment of Cardiovascular Diseases, National Medical Research Center for Therapy and Preventive Medicine, Russia
Correspondence: Mamedov Mekhman, Head, Department of Secondary Prevention of Chronic Noncommunicable Diseases, National Medical Research Center for Therapy and Preventive Medicine, Moscow, Russia, Tel 0079262283309
Received: May 15, 2023 | Published: May 22, 2023
Citation: Shukurov F, Mamedov M, Badeynikova K, et al. Improving the immediate and long-term results of endovascular treatment of a patient at extremely high surgical risk with coronary artery disease, diabetes mellitus and calcified multivessel coronary disease. MOJ Clin Med Case Rep. 2023;13(2):43-46. DOI: 10.15406/mojcr.2023.13.00434
The strategy of revascularization in severe calcified lesions is one of the most urgent problems of percutaneous coronary interventions (PCI). In recent decades, interest in rotational atherectomy has increased significantly, which is currently the method of choice for severe coronary calcification. A clinical example of successful endovascular treatment of a patient with a multivessel lesion with preliminary destruction of calcified atherosclerotic plaques by rotational atherectomy is presented. Patient K., aged 73, was hospitalized with a diagnosis of CHD: stable angina III functional class. Postinfarction cardiosclerosis (Q-forming myocardial infarction of the lower lateral localization from March 2022). Arterial hypertension. Type II diabetes mellitus. Type IIa dyslipidemia. The coronary angiography revealed 80% calcified stenosis in the terminal section of the main trunk of the left coronary artery with a transition to the proximal segment and 90% calcified stenosis in the middle segment of the anterior interventricular branch. The patient underwent endovascular rotational atherectomy followed by stenting of the affected segments of the coronary arteries. The postoperative period was uneventful, there was a positive trend in the condition: chest pain was not disturbed, including against the background of the expansion of the mode of physical activity, the symptoms of heart failure did not increase, and the patient was discharged on the 3rd day after the operation. At a planned control examination 3 months after the intervention, he noted an improvement in general well-being with an increase in the volume of physical activity without an angina clinic.
Keywords: revascularization, rotational atherectomy, coronary calcification
The strategy of revascularization in severe calcified lesions is one of the most urgent problems of percutaneous coronary interventions (PCI). Every fifth patient undergoing endovascular treatment has moderate or severe coronary calcification.1 Severe calcification significantly complicates traditional endovascular intervention. The deposition of calcium salts in atherosclerotic plaques prevents the establishment and deployment of coronary balloons and stents, increasing the risk of intraoperative complications, including dissection and perforation of the coronary arteries. It is not uncommon to observe technical problems such as insufficient and/or asymmetric stent deployment and incorrect positioning, which is associated with a suboptimal immediate outcome and a high likelihood of long-term cardiovascular events due to restenosis and thrombosis, which require repeated PCI.2,3
Given the unsatisfactory clinical outcomes of revascularization in severe calcified lesions, over the past decade, interest in rotational atherectomy has increased significantly, which is currently the method of choice for severe coronary calcification. Rotablation, in contrast to the standard intervention, makes it possible to safely modify and partially crush atheromatous masses by advancing a rotating drill and create a uniform enlarged vessel lumen for the possibility of performing balloon angioplasty and stenting with a satisfactory angiographic result.4,5 This procedure helps to minimize vessel barotrauma during ballooning, thus preventing neointimal dissection and hyperplasia as a risk factor for restenosis and facilitates drug diffusion when using drug-eluting stents due to the destruction of the calcium barrier.6 Below is a clinical example of successful endovascular treatment of a patient with a multivessel lesion involving the main trunk of the left coronary artery (LCA) and the anterior interventricular branch (LAD) with preliminary destruction of calcified atherosclerotic plaques by rotational atherectomy.
Patient K., 73 years old, was hospitalized at the National Medical Research Center for Therapy and Preventive Medicine in September 2022 with a diagnosis of coronary heart disease: stable angina III functional class. Postinfarction cardiosclerosis (Q-forming myocardial infarction of the lower lateral localization from March 2022). Arterial hypertension. Type II diabetes mellitus. Type IIa dyslipidemia.
On admission, the patient complained of pressing pain behind the sternum and shortness of breath with little physical activity, passing at rest with a positive effect from the use of Nitrospray.
The patient suffered from hypertension for a long time. Since the autumn of 2019, he noted the appearance of shortness of breath with a gradual decrease in exercise tolerance, and in March 2022, without a previous coronary history, he suffered a myocardial infarction of the lower and lateral walls of the left ventricle (LV) with the development of an intense anginal attack but was not hospitalized. Subsequently, he noted a progressive increase in shortness of breath, for which in April 2022 he was admitted to the hospital of the Moscow city hospital. Selective coronary angiography (CAG) revealed a multivessel lesion of the coronary arteries: severe calcification of the coronary arteries, stenosis in the mouth and middle segment of the main trunk of the LCA up to 80%; LAD stenoses: in the proximal segment 30% and on average segment 90%, below - aneurysmal expansion of the artery up to 6 mm; stenosis of the diagonal branch (DV): in the proximal segment 50% and in the middle segment 70%; the right coronary artery (RCA) was diffusely changed with ectasia throughout up to 5-6 mm; the posterior lateral branch (PBA) of the RCA is occluded from the orifice. When calculating SYNTAX Score I was 25.5 points (a scale for assessing the severity of coronary lesions and the risk of adverse cardiovascular events after PCI), SYNTAX Score II for PCI and coronary artery bypass grafting (CABG) - 40.4% and 70.1%, respectively (scale for assessing the probability of 4-year mortality after PCI and CABG, taking into account clinical indicators) (in the case of the patient under discussion: elderly age, male sex, creatinine clearance according to the Cockcroft-Gault formula - 66 ml / min, LV ejection fraction (EF) - 40 %, the presence of chronic obstructive pulmonary disease (COPD) and peripheral atherosclerosis), EuroSCORE II - 4.95% (risk assessment scale for in-hospital death after CABG). CABG was refused due to the severity of the condition, correction of therapy and endovascular myocardial revascularization were recommended. In June 2022, repeated coronary angiography was performed at the National Medical Research Center for Therapy and Preventive Medicine, which revealed 80% calcified stenosis in the LCA OS and 90% extended calcified stenosis in the proximal and middle segments of the LAD. An attempt was made to perform endovascular myocardial revascularization, however, numerous attempts to insert low-profile balloon catheters using various techniques were unsuccessful due to significant calcium deposition in the stenosis zone. Further stent implantation was abandoned due to the high risk of intraoperative complications, and planned endovascular rotational atherectomy was recommended.
An objective examination: a state of moderate severity. Electrocardiography (ECG) showed sinus rhythm with a heart rate (HR) of 58 beats/min, deviation of the electrical axis of the heart (EOS) to the left, signs of focal cicatricial changes in the myocardium of the lower LV wall, and nonspecific changes in the ST segment and T wave were recorded. According to echocardiography (echoCG), significant LV dilatation, moderate expansion of both atria, moderate eccentric LV myocardial hypertrophy, pronounced impairment of local LV myocardial contractility were revealed: diffuse hypokinesis, more (up to akinesis) in the lower and lateral walls, a significant decrease in global systolic LV function (EF according to the Simpson method - 37%), mitral regurgitation of 2-3 degrees and tricuspid regurgitation of 2 degrees.
The patient underwent endovascular rotational atherectomy followed by stenting of the affected segments of the coronary arteries. The intervention was carried out under the control of optical coherence tomography (OCT). Initially, the right common femoral artery was punctured under local anesthesia and a 7F introducer was placed. Next, the guide catheter was placed at the mouth of the LCA. The coronarogram revealed 80% calcified stenosis in the terminal LCA OS with a transition to the proximal segment of the LAD and 90% calcified stenosis in the middle segment of the LAD (Figure 1). Using a microcatheter, a conductor was introduced into the apical segment of the LAD. Next, the destruction of calcified atherosclerotic plaques in the LCA and LAD was performed using the Rotablator system of rotational atherectomy (Figure 2), after which, under OCT control (Figure 3), predilatation of the stenotic areas of the LAD with a 2.25x15 mm balloon catheter was performed, followed by positioning and implantation in the area of residual stenoses in the middle segment of the LAD, the proximal segment of the LAD and the OS of the LCA of everolimus drug-eluting stents 3x38 mm and 4x38 mm, respectively. Then, post-dilatation of the stented segments with 3.5x20 mm, 4.5x15 mm balloon catheters and proximal optimization in the LCA OS with a 5x15 mm balloon catheter were performed, achieving a good angiographic result: blood flow in the TIMI-3 arteries. On the control image and OCT control, the stents were fully extended, no signs of dissection were detected, and no residual stenoses were found (Figure 4, 5).
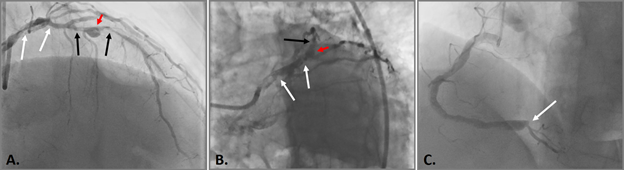
Figure 1 Selective coronary angiography.
A. and B. 80% calcified stenosis in the terminal LCA and proximal LAD segment (white arrows), 90% calcified stenosis in the middle LAD segment (black arrows) and aneurysm in the middle LAD segment with a diameter of up to 6 mm (red arrow); C. RCA is diffusely changed, expanded throughout up to 5-6 mm; VZV is occluded from the orifice (white arrow).
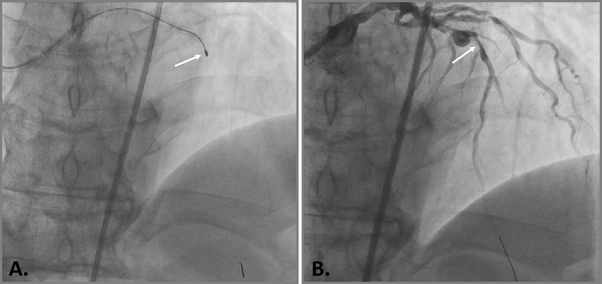
Figure 2 Endovascular rotational atherectomy.
A. Rotational drill in the area of the stenosed middle segment of the LAD (white arrow); C. Angiographic result of a rotational atherectomy in the region of the middle segment of the LAD (white arrow).
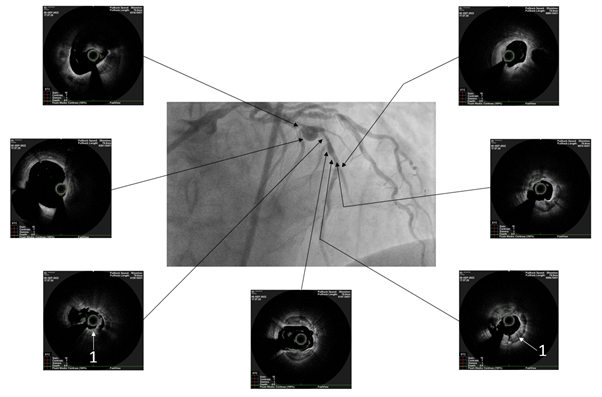
Figure 3 Optical coherence tomography after rotational atherectomy.
White arrows indicate destroyed concentric calcification (1).
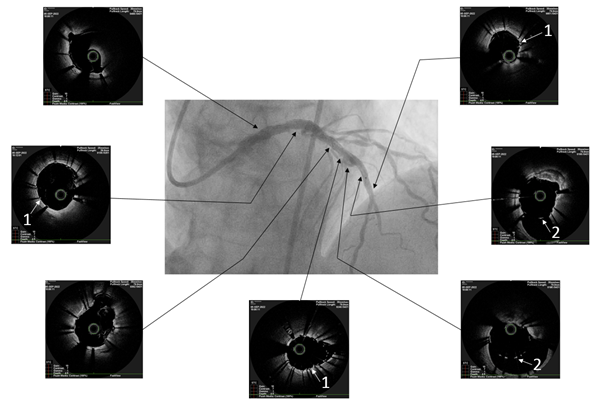
Figure 5 Optical coherence tomography after balloon angioplasty and stenting.
White arrows indicate full adherence of stent cells to the vessel wall (acoustic shadows of stent strata) (1) and stent cells in the area of aneurysmal expansion of the vessel (2).
The postoperative period was uneventful, there was a positive trend in the condition: no chest pain, including against the background of the expansion of the mode of physical activity, the symptoms of heart failure did not increase, and the patient was discharged from the hospital on the 3rd day after the operation.
Currently, the patient is under dynamic observation, and during a planned follow-up examination 3 months after the intervention, he noted an improvement in general well-being with an increase in physical activity without an angina clinic.
Rotational atherectomy was developed as a method for the complete removal of atherosclerotic plaques and was considered as an independent intervention or a preliminary stage before balloon angioplasty. With this approach, a high rate of restenosis was observed in the long-term period7,8 and, considering other disadvantages of the procedure, such as the risk of distal embolization in the absence of active aspiration and peripheral filter protection, the use of larger sheaths and an increase in the duration of the intervention, rotablation has lost its practicality significance.
Attempts to routinely perform rotablation followed by angioplasty and stenting both in the era of bare-metal stents7 and in the era of drug-eluting stents9 did not have a significant effect on the severity of restenosis and the incidence of late ischemic events.
Thanks to the improvement of equipment and techniques of interventional interventions, rotational atherectomy has occupied a niche where traditional ballooning and implantation of stents are insufficient - in case of severe calcification of the coronary bed.
According to the results of the ROTAXUS study, rotablation before angioplasty and stenting of a calcified lesion resulted in greater immediate angiographic success (92.5% in the rotatable group vs.) At clinical follow-up, almost a third of the patients included in the study developed serious cardiovascular events over a two-year period, but there were no statistically significant differences between the groups of rotablation and isolated angioplasty and stenting.10
Similar results were obtained in the PREPARE-CALC study, in which patients with severe coronary artery calcification were divided into rotational atherectomy and modified balloons before stent implantation. The criteria for the success of the procedure were achieved by 98% of patients from the first group and 81% of patients from the second group, respectively. After 9 months of follow-up, differences in stented vessel diameter loss between groups were not statistically significant. In addition, when assessing procedural complications, the total dissection rate in the rotablation group was 7%, and in the ballooning group it was 9%.11
Rotational atherectomy in the area of heavily calcified “unprotected” LCA OS requires special attention, since this vessel provides blood supply to 75% of the mass of the left ventricular myocardium with the “right” or “balanced” type of blood supply and 100% in the case of the “left” type of blood supply. The rotablation technique for bifurcation calcified lesions of the coronary bed also leads to more favorable immediate and long-term results compared to isolated angioplasty and stenting, preventing displacement, as a rule, of large bifurcation plaques and acute occlusion of the lateral branches.12
Thus, the technique of rotational atherectomy in combination with balloon angioplasty and implantation of modern drug-eluting stents is an effective and safe strategy for endovascular treatment of patients with severe calcified coronary disease, including in the LCA and LAD, which is demonstrated by the clinical observation described above.
Currently, the use of rotablation in the Russian Federation is limited and accounts for less than 1% of the total number of endovascular interventions. The introduction of this procedure into a wider clinical practice, facilitated, among other things, using imaging methods such as intravascular ultrasound and/or optical coherence tomography, will significantly improve the immediate and long-term results of endovascular treatment of this category of patients.
None.
Authors declare that there is no conflict of interest.

©2023 Shukurov, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.