MOJ
eISSN: 2381-179X


Case Report Volume 14 Issue 2
1Orthopaedics Surgery Resident, Pontificia Universidad de Valparaíso, Chile
2Orthopaedics Surgery Resident, Universidad Finis Terrae, Chile
Correspondence: Jorge Dania Calderón MD, Pontificia Universidad de Valparaíso, Chile
Received: April 16, 2024 | Published: May 29, 2024
Citation: Calderón JD. Importance of adequate and timely diagnosis in non-neoplasic bone lesions: case report. MOJ Clin Med Case Rep. 2024;14(2):48-50. DOI: 10.15406/mojcr.2024.14.00461
Non-ossifying fibroma is defined as a bone lesion of non-neoplasic origin, characterized by the presence of fibrous tissue in eddies, it differs from the fibrous cortical defect due to its size, being the result of the periosteal cortical bone development defect that leads to failure of ossification. We present a case of a 12-year-old female adolescent who comes to this center presenting knee pain, claudication while walking and reduced range of motion of the left knee and that in the CT scan shows a hyper-enhanced lesion, hypointense on T1, hyperintense on T2, in addition to cortical lesion at the level of both distal femurs. Planning is carried out for taking a percutaneous biopsy whose report reports a non-ossifying fibroma of the bilateral distal femur, and it is decided to perform surgery on the right distal femur, with good results, in the case the clinical and radiographic characteristics of the patient and the resolution of this are described.
Keywords: non-ossifying fibroma intramedullary nailing, cortical fibrous defect children's, orthopedics
Non-ossifying fibroma is defined by the World Health Organization as a non-neoplasic bone lesion of obscure etiology, characterized by the presence of fibrous tissue arranged in swirls, containing multinucleated giant cells, hemosiderin pigment and lipid-laden histiocytes. Non-ossifying fibroma (non-osteogenic fibroma) and cortical fibrous defect (metaphyseal defect) are the most common fibrous lesions of bone and are histologically identical. They are differentiated by their size: if it is less than 2 cm, it is called a fibrous defect and if it is more than 2 cm it is called a non-ossifying fibroma. The injury is due to the proliferation of bands of connective tissue cells in the bone. It is the result of the developmental defect of the periosteal cortical bone that leads to failure of ossification.1–3 There are no specific clinical manifestations, and the diagnosis is often established from radiographs taken after trauma. Due to its location adjacent or close to the insertion of muscles, tendons and ligaments, symptoms such as pain are sometimes not clearly interpreted and are confused with other diseases, hence the importance of maintaining a high index of suspicion for this disease injury.4 The most used diagnostic means are simple radiography, computed tomography (CT) and magnetic resonance imaging (MRI). Bone scintigraphy shows an image in the healing phase where there is a homogeneous increase in uptake.5
12 year-old female adolescent patient who is evaluated in the company of her mother referred for left knee pain in a study of 1 year of evolution and tumor of the distal femur and left proximal tibia, which is evident in AP and Lateral radiography of the left knee (Figure 1), and in AP and Lateral X-ray of the left distal femur (Figure 2). On physical examination, she presented claudication decreased range of motion of the left knee with pain on flexion >90°. Contrasted Nuclear Magnetic Resonance was performed (Figure 3) with the finding of a hyperenhancement lesion, hypointense on T1, hyperintense on T2, in addition to a cortical lesion at the level of both distal femurs. Studies are complemented with endocrine evaluation with results within normal limits and x-rays of long bones ruling out any other focus of injury.
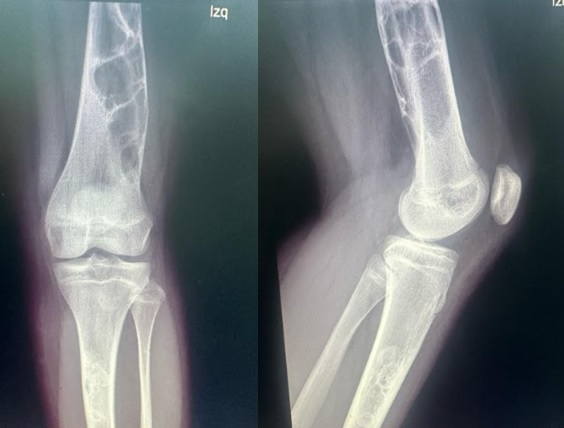
Figure 1 Left Knee AP and lateral X-ray: multiloculated image, with a thin sclerotic edge, with non-cortical reaction, without soft tissue injury.

Figure 2 Left distal femur AP and lateral X-ray: multiloculated image, with a thin sclerotic edge, without cortical reaction, without soft tissue injury.
Planning is made to take a percutaneous biopsy, which is performed and whose report reports non-ossifying fibroma of the bilateral distal femur. It was decided to place a knee immobilizer and ambulation with canes in unloading of the left lower extremity as a protective measure against future pathological bone fracture. He was maintained in weekly check-ups for clinical and radiological evaluation with adequate evolution, ruling out the presence of fracture. In the postoperative control one month later, removal of the immobilizer and initiation of free walking at home and the use of canes for long distances are indicated. Surgery is planned where a lateral approach to the right distal femur is performed, a square window is drilled in the central region of the main defect, curettage of the lesion, tissue is taken for biopsy and cleansing with abundant physiological saline, then distal curettage is performed of the injury completely. It is filled with 50 cc of Sinermed® brand bone allograft (Providencia, Chile) in the metaphyso-diaphyseal defect, the size of the isthmus of the spinal canal is determined and 2 Synthes® brand TEN nails of 3.5 mm (Raynham, USA) and 1 of 2 are introduced at the distal metaphysodiaphyseal level. 5 mm contoured with a 45° curve at the insertion end and a smooth, uniform curvature over the remaining length interlocked together in the spinal canal, checking for adequate graft filling of the lesion and good hardware position.
The patient remains hospitalized for 72 hours postoperatively with adequate progress and is discharged with instructions to keep the operated limb unloaded. He subsequently attended clinical control, highlighting good pain tolerance with slight limitation to flexion-extension. The postoperative control radiograph shows adequate positioning of osteosynthesis material and bone filling at the level of the defect (Figure 4). Kinesiotherapy and partial weight bearing begin. During radiological control, signs of consolidation were observed in the graft area, so a total weight load was decided as tolerated and it was monitored 2nd month after surgery. The patient presented improvement in terms of gait, greater strength, and knee joint range.
Non-ossifying fibroma (NOF), also known as metaphyseal or cortical fibrous defect, is considered a lesion with spontaneous regression in skeletal maturation. The presentation of this disease can vary from asymptomatic to the presence of pathological fracture. Due to its location adjacent or close to the insertion of muscles, tendons and ligaments, symptoms such as pain are sometimes not clearly interpreted and are confused with other diseases, hence the importance of maintaining a high index of suspicion for this disease injury.6 FNO predominates in males in 60% of cases. The highest incidence occurs in the first two decades of life, especially the second.3
The diagnosis of FNO in the long bones is based on the characteristic radiographic and clinical appearance, typically FNO appears as an asymptomatic multiloculated lesion, often identified incidentally during a radiographic evaluation indicated for another reason.5 The interior architecture has a foamy appearance. Typically, there is a cortex of reactive bone or sclerosis surrounding the lesion. There may be cortical thinning and, in some cases, slight expansion, which may be misinterpreted as malignant change. The size varies from 0.5 to 7 cm. The most frequent location is the metaphyses of the long bones, especially in the lower extremities, around the knee (distal femur, proximal or distal tibia and fibula). In the bone they are usually eccentric, several centimeters away from the cortex and more frequently intramedullary. Very rarely they are purely diaphyseal. Generally, plain radiographs are sucient for diagnosis; if in doubt, additional imaging studies can be performed.7 In cases of a disrupted lamellar periosteal reaction, radiographic findings could mimic bone malignancy.8
However, a single layer of new bone formation in the periosteum is typical of a stress fracture injury and a malignancy could be excluded due to lack of cortical destruction or tumor extension into the surrounding soft tissues.9 An infection could also be considered in the differential diagnosis, but the exertional nature of the pain lasting several months along with the normal laboratory findings ruled out this possibility. Radiographic evidence of advanced bone healing may also aid diagnosis. In most patients, treatment is conservative.10,11 Flinck et al.12 performed a biomechanical comparison of semi-rigid locked intramedullary nails versus titanium elastic intramedullary nails in femur fracture models, where they evaluated the combination of two 4.0 mm titanium elastic intramedullary nails or femur fracture models femur treated with additional 3.0 mm titanium elastic intramedullary nails, produce much greater stability. Models treated with two 3.0 mm titanium elastic intramedullary nails had poor rotational stability in many tests.
Non-Ossifying Fibroma is a complex pathology that needs to be diagnosed, evaluated, and treated appropriately to obtain good results. In our case, after diagnosis, planning is made to take a percutaneous biopsy and it is decided to perform right distal femur surgery with good results, clinical and radiographic characteristics of the patient and its resolution are described. It is important to keep in mind that it is a pathology where we do not find characteristic and/or distinctive clinical findings, and that may have a variable progression over time, so it is ideal that more studies and research be carried out on this condition.
None.
The authors declare that there is no conflicts of interest.

©2024 Calderón, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.