MOJ
eISSN: 2381-179X


Case Report Volume 13 Issue 3
1Department of Medicine, Faculty of Medicine & Health Sciences, An-Najah National University, Palestine
2Department of Neurosurgery, Palestinian Medical Complex, Palestine
Correspondence: Karam Rabi, Department of Neurosurgery, Palestinian Medical Complex, Ramallah, Palestine
Received: September 25, 2023 | Published: October 18, 2023
Citation: Rabi K, Alhammouri S, Saa S. Guarding against the storm: the imperative of early intracranial hemorrhage recognition in end-stage renal disease and hypertension: a case report. MOJ Clin Med Case Rep. 2023;13(3):69-71. DOI: 10.15406/mojcr.2023.13.00441
Intracranial hemorrhage (ICH) is a critical neurological event, often associated with uncontrolled blood pressure. While hypertension may arise from various underlying factors, it is nearly always linked to renal pathology, and end-stage renal disease (ESRD) in particular, forming a robust connection. This connection further underscores the intricate relationship between ESRD and hypertension, particularly concerning the development of intracranial hemorrhage in affected patients. We present a case of a 55-year-old male who initially arrived at the emergency department with a sudden, severe headache, recurring episodes of vomiting, and a swift progression into confusion. A non-contrast brain CT scan revealed a notable area of increased density within the brain parenchyma, signifying a substantial intraparenchymal hemorrhage on the right side. The hemorrhage has consequently resulted in a midline shift, measuring approximately 9 millimeters. The patient's surgical intervention proceeded without any complications. Postoperatively, the patient showed remarkable improvement compared to his initial presentation. The association between end-stage renal disease (ESRD), hypertension, and intracranial hemorrhage highlights the importance of vigilance among emergency physicians. Recognizing the connection between these factors can aid in the early diagnosis and management of intracranial hemorrhage in ESRD patients, potentially improving outcomes and reducing complications. This case report serves as a reminder of the need for heightened awareness and timely intervention in such cases.
Keywords: ICH, hemorrhage, ESRD, hypertension, brain, emergency
The demographic of patients grappling with end-stage renal disease (ESRD), necessitating dialysis, is witnessing a steady surge, accompanied by a mortality rate significantly exceeding that of the general population.1,2 Within this cohort, the emergence of intracranial hemorrhage (ICH) as a complication is not uncommon, and it frequently comes intertwined with the intricacies of cerebral edema. The process of hemodialysis (HD) itself introduces rapid osmolar and fluid shifts, ultimately elevating the brain's water content, thus potentially exacerbating cerebral edema. The perils entailed in administering HD to individuals grappling with acute ICH have predominantly been elucidated in sporadic case studies.3 Notably, end-stage renal disease (ESRD) stands as one of the most critical risk factors predisposing individuals to intracerebral hemorrhage.4 Consequently, maintaining a vigilant approach when assessing ESRD patients presenting with sudden-onset headaches becomes paramount. This vigilance is underscored by the looming risk of severe hypertension and the development of aneurysms known as Charcot-Bouchard aneurysms, which develop as a consequence of chronic hypertension. Individuals with chronic systemic hypertension are at high risk of developing atrophy of the outer muscular layer. With the loss of integrity of the vessel wall, microaneurysms develop in lenticulostriate Branches (LSA), which are at high risk of rupture. The hemorrhaging of these aneurysms into the brain's deep structures, referred to as intraparenchymal hemorrhage or, more broadly, intracerebral hemorrhage, can culminate in dire consequences if not expeditiously addressed.5
In this case report, we explore the critical and often life-threatening manifestation of hypertensive intracranial hemorrhage (ICH) in individuals afflicted by ESRD and hypertension. Our aim is to underscore the paramount importance of early diagnosis and swift intervention in this intricate clinical landscape. Timely recognition and management of hypertensive ICH can significantly alter patient outcomes. Through this report, we intend to emphasize the significance of vigilance, timely intervention, and a multidisciplinary approach when confronting the formidable confluence of ESRD, hypertension, and hypertensive ICH.
A 55-year-old male, diagnosed with end-stage renal disease (ESRD) and hypertension, was urgently transported to the emergency department due to the sudden onset of a severe headache. This incapacitating headache, which occurred in a relaxed, non-strenuous setting, was accompanied by recurrent episodes of vomiting and rapidly progressed to a state of confusion. Additionally, the patient reported experiencing eye pain and blurred vision immediately following the onset of this distressing episode. This intricate clinical presentation is compounded by the patient's extensive medical history, including a 15-year battle with diabetes mellitus (DM), further complicated by diabetic nephropathy and retinopathy over the past 5 years. Moreover, the patient has been managing hypertension for 6 years, necessitating ongoing antihypertensive medications. 5 years ago, the diagnosis of end-stage renal disease was established, leading to the initiation of a maintained hemodialysis regimen. Upon arrival, the patient exhibited generally stable vital signs, except for a notable blood pressure reading of 210/100 mm Hg. Although the Glasgow Coma Scale (GCS) indicated a score of 14 out of 15, suggestive of relatively preserved consciousness, the patient was notably unable to articulate speech. This condition further deteriorated to a GCS score of four out of 15, necessitating immediate surgical intervention. During the chest examination, bilateral decreased air entry was evident, with a more pronounced reduction noted on the left side. On further neurological assessment, the patient presented with a striking clinical finding: left-sided paraplegia, indicating impaired motor function in the lower limbs. A non-contrast brain CT scan revealed a hyperdense lesion on the right side of the brain, consistent with intraparenchymal hemorrhage (Figure 1). This hemorrhagic region was accompanied by a significant midline shift measuring approximately 9 millimeters, indicative of the displacement of brain structures toward the opposite side due to the intracranial hemorrhage.

Figure 1 Non-contrast preoperative brain CT scan depicting right intraparenchymal hemorrhage and evident midline shift.(A-C): different levels of brain CT scam showing the size and extent of the ICH.
The surgical evacuation of the intraparenchymal hemorrhage entailed a meticulously executed craniotomy procedure that was employed to provide access to the intracranial compartment and to facilitate direct access to the site of hemorrhage within the cerebral tissue. The cranial incision, was carefully tailored to the precise location of the hematoma, serving as a crucial portal through which the surgical team could meticulously navigate the brain.
Following the successful evacuation of the intraparenchymal hematoma and the alleviation of elevated intracranial pressure, a Postoperative non-contrast brain CT scan showed significant improvement and no residual hemorrhage or pressure effect could be seen (Figure 2). An important aspect of the procedure involved the thoughtful repositioning of the previously removed bone flap. This restorative step was undertaken with extreme precision, considering both structural integrity and the capacity for physiological expansion within the cranial vault. The bone flap was carefully secured in a manner that not only provided protection to the vital neural structures beneath but also allowed for the accommodation of normal physiological processes and fluctuations within the intracranial environment. The surgery went smoothly, even though the bone flap moved because of the ongoing high pressure inside the skull.
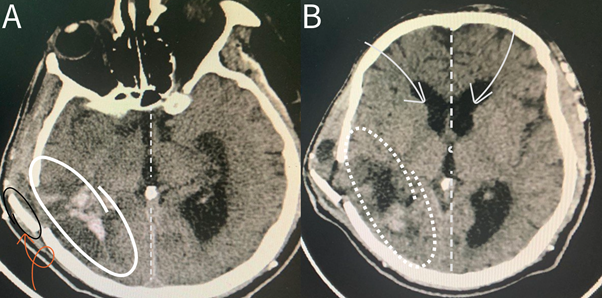
Figure 2 Postoperative non-contrast brain CT scan showing the region where the previous hemorrhage occurred, with a noticeable return to the normal midline position of brain structures. (A) Lower brain section CT scan with notable return to midline (dashed line), and a clearly seen bone flap (orange curved arrow). (B) Upper brain section CT scan showing normal position f midline structures.
Post-operatively, the patient’s overall condition appeared stable and well, characterized by vital signs within normal parameters, with the exception of elevated blood pressure readings. The Glasgow Coma Scale (GCS) yielded a perfect score of 15/15, indicating optimal levels of consciousness. Both pupils demonstrated reactivity to light, although visual acuity remained notably impaired. Motor function assessment revealed that the patient could move all four limbs, albeit with residual weakness more pronounced on the left side compared to the right. His neck exhibited a normal range of motion, indicating the absence of restrictions or discomfort. On neurological examination, left-sided body weakness was evident, with a power grade of two out of five. This weakness was particularly prominent in the lower limbs when contrasted with the upper limbs, suggesting varying degrees of impairment. Chest examination continued to reveal decreased air entry on the right side, despite the presence of a chest tube. Examination of the lower limbs detected no signs of deep vein thrombosis (DVT), yet marked edema was observed in the lower extremities. Notably, the bone flap was palpable beneath the skin. The presence of the palpable bone flap beneath the skin is a consequence of its mobility, primarily attributed to the increased intracranial pressure within the brain. It is important to note that this occurrence, although notable, does not raise immediate concerns, as it is an anticipated phenomenon that typically resolves over time.
In the one-month follow-up assessment at the outpatient clinic, the patient exhibited significant and noteworthy progress, manifesting the ability to ambulate autonomously without any lingering lower limb weakness. No postoperative CT was needed, as the patient exhibited improvement and showed excellent recovery. This remarkable recovery highlights the efficacy of the medical intervention and the patient's dedication to their rehabilitation, marking a successful and encouraging step forward in their journey to restored health.
The case report at hand unveils a compelling narrative of the intricate interplay between intracranial hemorrhage (ICH), end-stage renal disease (ESRD), and hypertension, underscoring the pivotal importance of timely intervention. Within this complex medical landscape, the convergence of these comorbidities creates a precarious scenario, demanding a nuanced approach. Hypertension, a frequent companion of ESRD, emerges as a significant risk factor for the onset of ICH. The patient's prolonged history of hypertension, exacerbated by the insidious progression of diabetic nephropathy and retinopathy, heightened the vulnerability to this catastrophic event. Hemorrhage expansion affects approximately 20% of individuals within the initial 24 hours following the onset of acute intracerebral hemorrhage, and it is correlated with adverse outcomes, including mortality and disability, which makes it an appealing therapeutic target.6 Early recognition and swift surgical intervention, specifically through craniotomy, emerged as the linchpin of successful management. This proactive approach alleviated the intracranial pressure, thereby shielding the delicate neural structures from further damage. The case serves as a poignant reminder of the intricate relationships that exist within the realm of medical comorbidities and reinforces the profound impact of judicious and timely care on patient outcomes.
It is worth mentioning that the mortality rate for ICH is relatively high. The 30-day mortality rate for ICH ranges from 35% to 52%.7 This means that a significant proportion of patients do not survive beyond the first month after the onset of ICH. Additionally, studies have shown that even survivors who regain some degree of functional independence may have a reduced quality of life compared to the general population. Post-ICH complications and disabilities can impact daily living and overall well-being.8
These statistics and references provide insights into the mortality and morbidity associated with intracranial hemorrhage. It's important to note that individual outcomes can vary widely, and timely medical intervention and rehabilitation can significantly impact a patient's prognosis.
In the presented case, the longstanding history of hypertension, coupled with the challenges posed by diabetic nephropathy and retinopathy in the context of ESRD, rendered the patient highly susceptible to ICH. The urgency of early recognition and swift surgical intervention through craniotomy was evident, playing a pivotal role in mitigating the neurological consequences of the hemorrhage, effectively relieving intracranial pressure and protecting vital neural structures.
This case report underscores the significance of prompt and collaborative care in managing patients grappling with intricate medical comorbidities. Through vigilant monitoring, early intervention, and a holistic approach encompassing medication adherence, lifestyle modifications, and ongoing follow-up, we can aspire to enhance the quality of life for patients facing the complex challenges posed by the triad of ICH, ESRD, and hypertension. In this intricate medical landscape, timely and comprehensive care remains the core guiding us toward better patient outcomes and improved well-being.
None.
Authors declare that there is no conflict of interest.

©2023 Rabi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.