MOJ
eISSN: 2381-179X


Case Series Volume 10 Issue 2
1Department of Neurology, Mediclinic City Hospital, Dubai
2Mohammed Bin Rashid University of Medicine and Health Sciences
3Department of Radiology, Mediclinic City Hospital, Dubai
Correspondence: Heike Jacobs, Department of Neurology, Mediclinic City Hospital Dubai, UAE
Received: April 07, 2020 | Published: April 20, 2020
Citation: Jacobs H, Ghanem HA, Mordani J, et al. Fast effective treatment of spontaenous CSF leak causing intracranial hypotension and debilitating orthostatic headache. MOJ Clin Med Case Rep . 2020;10(2):36-39. DOI: 10.15406/mojcr.2020.10.00338
We are reporting a case series describing clinical, laboratory, MRI and CT myelogram imaging and treatment results for 4 patients with spontaneous cerebral spinal fluid (CSF) leak with subsequent intracranial hypotension; all of which resolved via blood patches.
A 33-year-old woman (case 1) presented abrupt onset severe pain in the back and head; without preceding trauma or procedure. MRI brain revealed leptomeningeal enhancement, after CT myelogram identifying a CSF leak she received a 20ml epidural blood patch in the lumbar area. By the next day her symptoms had completely resolved.
A 36year old woman (case 2) with 1 year-long history of positional headaches. Her CT Myelogram showed frequent multilevel Tarlov Cysts; one of which displayed leakage. Her orthostatic headaches disappeared after repeated EBP.
A middle aged male (case 3) had an acute onset headache which persisted with orthostatic features since 6 weeks. He had complete remission after one epidural patching. A 47 year old man (case 4) presented with 5 days of typical orthostatic headaches, CT Myelogramm demonstrated a leaking thoracolumbar cyst. He required 2 EBP within 3 days to completely recover. Our cases support the notion that blood patching is a fast, effective and safe treatment for an increasingly recognized diagnosis of orthostatic headache caused by spontaneous intracranial hypotension.
Keywords: intracranial hypotension, spontaenousdural leak, blood patch, orthostatic/ positional headache, dural fistula, pachymeningitis, DME, tarlov cysts
LP, lumber puncture ; CSF, cerebrospinal fluid.
Changes in CSF production, absorption and flow can lead to changes in CSF volume and pressure which causes neurological sequelae, the most common being orthostatic/positional headaches. Spontaneous intracranial hypotension is being recognized with increasing frequency.
A CSF leak located in the spine is today thought to be the prevailing etiology. Either through rupture of the arachnoid membrane or Tarlov cysts opening the dura or spontaneous development of a venous fistula enabling drain from the subarachnoid space directly into the epidural space.
Clinical features are acute or gradual onset of headache; usually within 15 minutes of sitting or standing, rarely as thunderclap. Cases with neck and back pain and no meningeal enhancement are documented.
Relief usually occurs within minutes of lying down. The quality of pain consists of throbbing or dull, focal or generalized pain. Intensity can vary from mild to incapacitating. Location can be frontal as often as occipital and diffuse.
Clear orthostatic features can lack or be paradox in rare cases. Associated symptoms are nausea, vomiting, visual disturbances, and unsteady gait. Focal neurological symptoms can occur with distortion or compression of brain structures: ataxia, quadriparesis, and decreased level of consciousness in progressed cases.
Case 1: A previously healthy Sri Lankan 33-year-old female developed acute onset severe pain in the lower back while driving a week ago. She reported radiation to the head with marked frontal focus. The neck was painful to passive rotation and bending. Her symptoms progressed to orthostatic headaches in which she was unable to walk and was vomiting multiple times a day.
She had MRI brain and C spine with contrast, (Figure 1) a lumbar puncture after imaging, intravenous pain medication, dexamethasone per os, and was positioned supinely. Her brain MRI and C spine showed signs of low intracranial pressure with DME; see in Figure 2. She initially had a traumatic and dry LP with Glucose 5.68, raised protein of 3672 mg, 54000 red cells, 43 white cells and xanthochromia was positive.
Under the suspicion of intracranial hypotensive headache caused by acute CSF leakage, a CT myelogram was performed Figure 3 the needle was set at L3/4 under radiographic control, contrast was repeatedly injected and x-ray images of lower and upper spine performed. After filling up to the cervical level of the epidural space, the patient’s whole spine was imaged with CT and extravasation was noted Figures 4 & 5.
A 20ml blood patch was set at the side of the lumbar puncture (L3) after withdrawing the needle from the subdural area into the epidural space.3 hours after the procedure the patient reported a significant reduction of pain and was able to sit up. She was discharged the next morning pain free and mobile.
Case 2: A previously healthy Pakistani 36-year-old female presents with a 1-year history of recurrent severe positional headaches. She reports developing a chronic tension type headache which was driven by medication overuse. This patient required 2 epidural patches to treat the positional headache successfully.
Her imaging showed multiple foraminal cysts; see in Figure 6.
The left L 2/3 nerve root sleeve demonstrates an intra- foraminal Tarlov cyst measuring approximately 7mm indiameter with active extravasation of contrast in the surrounding tissues along the left para spinal muscles.
L 1/2 nerve root sleeve demonstrates bilateral small Tarlov’s cysts, the cyst on the left measures up to 4mm in diameter; the right measures up to 2.5mm in diameter; see Figures 7a & 7b.
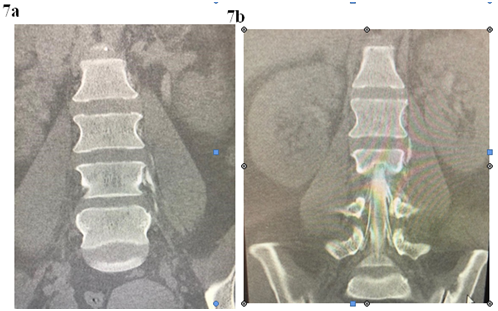
Figure 7a & 7b Myelogram: Extravasation of contrast into the paravertebral soft tissue around the left lumbar 2/3 Tarlov cyst suggesting a CSF leak at this level.
In the dorsal and lumbar spine several other levels of nerve root Tarlov cysts are identified: none of these described Tarlov cysts show any extravasation into the surrounding soft tissues. 20ml of fresh blood was injected into the epidural space immediately after instillation of contrast into the CSF space. Initially the patient was pain free but required a second patch 1 week later due to return of symptoms.
Case 3: A british male patient with a 6-week history of acute onset headaches which had migraine-like features with clear orthostatic components. Brain MRI revealed extensive leptomeningeal enhancement to suggest CSF leak or other leptomeningeal process. He had high CSF protein levels of over 6000mg/L.
The 6 weeks lasting headaches remitted completely after epidural patching.
Case 4: 47-year-old Caucasian male presents with a 5-day history of excruciating postural bilateral sharp, stabbing headaches coupled with neck pain; resolved to dull following supine position. He complains of bilateral ear block and nausea with no other associated symptoms.
Patient has history of discectomy at C6/7 level 2 years ago; CT myelogram revealed left sided Tarlov cyst leakage at T12/L1 level. CT-guided blood patch was successfully performed. There was immediate complete resolution of the headaches. There was a return of symptoms two days later and hence the patient needed another blood patch; result successful (Table 1).
Patient |
Case 1 |
Case 2 |
Case 3 |
Case 4 |
Duration of Symptoms |
1 week history |
1 year history |
6 week history |
5 day history |
Protein |
3672mg/L |
1183mg/L |
6801mg/L |
604 mg/L |
WBC |
43 |
7 |
28 |
10 |
Neut |
48 |
0 |
5 |
5 |
Lymp |
33 |
90 |
75 |
89 |
RBC |
54000 |
10 |
15 |
6 |
Table 1 All 4 patients had high protein in their CSF (normal protein: 150-400mg/L)
The clinical features of intracranial hypotension are headaches of sudden or gradual onset, developed within two hours,often within 15 minutes, of sitting or standing. Rarely, it starts as a thunderclap headache. If not diagnosed early they can persist for very long duration.
This matches with our patients: their presentation reached from “acute onset whilst driving” to longstanding “over 1 year.”Our Patients fitted the clinical descriptions of intractable headaches which are worse on standing or sitting and relief was typically obtained with recumbency within minutes.
We see ca 1000 headache patients per year and established4 cases of spontaneous orthostatic headaches over 2 years. This constitutes an incidence of 1/500 headache referrals in our institution at present with a female to male ration of 1:1. The estimated annual incidence in a systematic review from 2006 is 5 per 100,000, peak age 40, female to male ratio 2:1. It could be speculated that real incidences are indeed higher and more matching with our observations, and that reported numbers will raise with increasing awareness and ability to establish diagnosis and treatment.
Our success in diagnosis and management shows these patients can be easily and very effectively treated with a large volume epidural blood patch. The procedureis the goldstandard for post-puncture headaches with a presumed similar etiology for intracranial hypotension caused by CSF leakage.
CT myelography is the best investigation to identify the exact site of the CSF leak. Early and delayed images are obtained at each spinal level.
In 3 of our 4 cases we performed CT myelogram and identified CSF leakage, in one case (Nr 3) we performed EBP successfully without identifying the leak. Tarlov cysts present potential locations of leakage through spontaneous rupture resulting in persisting CSF leaks. In 2 out of the 4 cases we demonstrated Tarlov cysts, of which one had multiple distributed over several spinal levels and a leaking cyst lumbar. The 4th male case had a leaking cyst at T12/L1.
In 3 out of 4 of our cases the leaks where found in the lower spine which appears the most common incidence location below L1 in our cohort. The literature estimated CSF leaks most common at cervicothoracic levels.1 For patients who fail adequate trials of conservative therapy and repeated EBP treaments options include surgical repair of the defect. Dural tears and defects can be repaired with suture or fibrin glue. A case reported the success of surgical resection of a large arachnoid cyst with CSF. The leak was at thoracic level, initially managed with a thoracic blood patch.2 However surgical repair is only suggested for patients with clearly identified locus of leak and failed EBP.
Results after EBP are quite instantaneous with most patients being headache free within a few hours.All here reported cases completely recovered from their positional headaches with two cases needing a repeat patch. Studies highlight that ca 50% of patients with SIH require more than one EBP treatment.3 Upon follow-up, we observed that EBP treatment cured orthostatic headaches irrespective of other types of headaches. Illustrated in Case 2 who continued with persistent low grade tension headaches, whilst the agonizing high grade orthostatic headaches completely resolved.
Our patients have been followed from 4 weeks to 1 year with no further reuccurence. Spontaenous spinal CSF leakage is estimated to reoccur in ca 10% of patients regardless of treatment.4 There was no repeat myelogram to avoid creating a risk factor for CSF leakage. MRI could have been used to review for leptomeningeal enhancement; however, that would have been rendered ineffective following a LP. An MRI would have shown enhancement regardless due to artificial leaking and not to showcase a true cause.
It remains unclear exactly how such therapy actually addresses the underlying leaks. The blind patching might increase CSF pressure by displacement of volume in the epidural space, until spontaneous closure occurs.
Alternative mechanisms are blood coagulation and thrombosis the presumed leakage caused by a ruptured Tarlov cyst.
Data supports slightly higher effectivity for direct targeted patching for overt leaks or suspected leaks of nerve sheet diverticula in contrast to a blind patch.5 Other cases demonstrate effective thoracalpatching at T10/11 below a reported high cervical leak at C2.6
A lumbar puncture can document low CSF pressure in suspected cases of spontaneous intracranial hypotension. It may be useful when MRI showing diffuse pachymeningeal enhancement, is not available or not tolerated. Interestingly all our patients showed a high protein level in the CSF of varying degree. Potential causes of increased CSF protein include meningeal hyperemia leading to exudates. The dilated leaky meningeal vessels may allow protein exudation into the CSF. In addition, meningeal biopsies have shown non-specific inflammation possibly leading to increased CSF protein.7
Our cases elucidate the following considerations:
None.
None.
The authors have no conflicts of interest to declare.

©2020 Jacobs, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.