MOJ
eISSN: 2381-179X


Case Report Volume 11 Issue 3
Department of pediatrics, Tishreen University, Syria
Correspondence: Leen Doya, Department of pediatrics, faculty of medicine, Tishreen University, Syria
Received: February 23, 2021 | Published: June 14, 2021
Citation: Doya L, Mohammad L, Ghanem A. Factor V deficiency in a Syrian boy with spontaneous intracranial hemorrhage: a rare case report from Syria. MOJ Clin Med Case Rep. 2021;11(3):76-77. DOI: 10.15406/mojcr.2021.11.00386
Factor V (FV) deficiency is a rare autosomal recessive coagulation disorder that can manifest at any age. Spontaneous intracranial hemorrhage as the first manifests of Factor V Deficiency is extremely rare and may present with a sudden focal neurological deficit or a reduced level of consciousness. We report a case of a new onset-seizure without any history of medical ingestion, toxin exposure, trauma or falls in an 11- month- old boy. A cranial computed tomography showed right intra-cerebral bleed extending from the parietal lobe to the occipital region with a shift of the midline to the left. Laboratory results showed a decrease in Factor V activity. Fresh frozen plasma (FFP) was replaced with improvement.
Keywords: intracranial hemorrhage, factor V deficiency, fresh frozen plasma, G6Pd deficiency
Factor V (FV)deficiency is a rare autosomal recessive coagulation disorder with an estimated incidence of approximately one per million in the general population.1 This first clinical identified was in 1943 by Dr. Paul Owrenas severe bleeding tendency due to the deficiency of a previously unknown coagulation factor, so it is also called Owren’s disease, parahemophilia.2 Our report describes the first case of severe factor V deficiency presenting as spontaneous hemorrhage reports in a Syrian boy.
An-11-month old Syrian boy presented to our hospital in January 2018 with a new-onset seizure, starting right-sided jerking, and unresponsive to medication for 3 minutes. He had had recurrent vomiting (10-12 episodes per day) with pallor over the last 24 hours. The parents deny any history of medical ingestion, toxin exposure, trauma, or falls. He was the third child of the family. He was born at full term by normal, spontaneous vaginal delivery. His birth weight was 3.5kg. 1mg of Vitamin K was given intramuscularly at delivery. He had a small amount of self-limiting bleeding from circumcision on day 15 of life for 2 days. His development had been normal. The child underwent all the compulsory immunizations for his age. His parents were second cousins. There is no family history of seizures.
On examination, He looked well but pale. His weight was 11kg (normal), the length was 76cm (normal) and his head circumference was 47cm (normal). Cardiovascular, respiratory, and abdominal examinations were normal. The blood pressure (BP) was 100/60mmHg, oxygen Saturation (Sao2): 98%, the pulse rate was 110/min, body temperature was 37⁰C and respiration rate was 40/min. His spine and joints appeared normal, and there were no unusual birthmarks. Neurological examination showed normal cranial nerves and normal posture, tone, power, and reflexes in the upper and lower limbs. There were no focal neurological signs and no other signs. Funduscopic examination showed Roth's spots spread with cloudy papilla borders and ulceration vessels with flame bleeding. Contrast-enhanced computed tomography (CT) of the brain showed right intra-cerebral bleed extending from the parietal lobe to the occipital region with a shift of the midline (Figure 1). Laboratory results were as in Table 1.
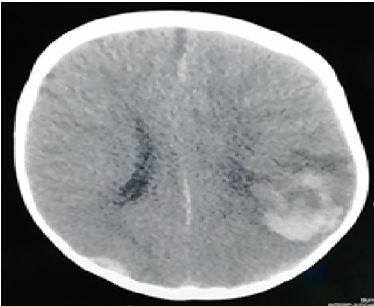
Figure 1 CT scan of brain showed parenchymal, epidural and subdural hemorrhage in the right parietal and occipital region with deviation of median.
|
Test |
Result |
Test |
Result |
|
White blood cells × (103/μl) |
22.9 |
K+ |
6.5 |
|
Neutrophils (%) |
75 |
ALT |
20 |
|
Lymphocyte (%) |
25 |
AST |
15 |
|
Haemoglobin (g/dl) |
6.5 |
Coombs test |
Normal |
|
Platelets × (103/μl) |
450 |
Fibrinogen |
Normal |
|
Urea (mg/dl) |
30 |
bleeding time |
Normal |
|
Creatinine (mg/dl) |
0.5 |
thrombin time |
Normal |
|
Hemoglobin electrophoresis |
Normal |
Prothrombin time(sec) |
18 |
|
Erythrocyte sedimentation rate (1 h) |
Normal |
INR* |
2.2 |
|
C-reactive protein (mg/dl) |
Normal |
APTT**(sec) |
82 |
|
Na+ |
136 |
|
|
Table 1
*international normalized ratio; normal range <1.14
**activated partial thromboplastin time; normal range <35 sec
Urinalysis, culture, and sensitivity were normal. PT and APTT were markedly prolonged. The level of the patient revealed a significant decrease of factor V below 1% (normal range 70-120%) and mildly decrease in factor VIII 64% (normal range 70-120%). Other coagulation factors (12,7,9,2,11, von Willebrand factor (VWF) were normal. Lupus anticoagulants were normal. After fresh red blood cell (RBC) and fresh frozen plasma (FFP) were replaced, PT recovered to 13sec and APTT to 30 sec. The patient recovered with FFP and supportive care. After 10 days, on following up the bleeding, magnetic resonance imaging (MRI) was performed and showed bleeding on the mend. (Figure 2).
After 2 weeks from admission, the patient was completely healed and has been followed at outpatient. A regime of 20ml/kg of FFP two times a month was instituted. immunizations including hepatitis B vaccination were given subcutaneously as is normal practice for children with severe bleeding disorders. No further bleeding has been noticed up to the present day and neurodevelopment has been within normal limits.
Since 1943, approximately 150 cases of isolated FV deficiency reported in the literature.3 several mutations in the F5 gene are related with Inherited factor V deficiency.4 More than 30%of FV-deficient patients are asymptomatic, while symptoms in the others range from spontaneous minor bleeding (the most common 34%) to Spontaneous major bleedings including; CNS bleeding, GI bleeding, hematoma. The hemorrhage of the nasal and oral cavity is common but intracranial hemorrhage is very rare.5 This case of isolated FV deficiency was discovered due to intracranial hemorrhage and abnormal PT and a PTT. It was unclear whether this patient has a homozygous mutation of the F5 gene since the mutation analysis was not available. There was no apparent family history was reported.
The diagnosis of FV deficiency is typically suspected in a patient with symptoms of bleeding and prolonged in PT, a PTT results that should be corrected after mixing study with normal plasma.6 Since there are neither FV concentrates nor recombinant FV available at this time, virus-inactivated FFP remains the mainstay of treatment.7
A new FV concentrate has been developed for clinical trials, and related preclinical studies are being conducted for the orphan drug designation application.8
In our patient due to younger age and severe intracranial hemorrhage, regular FFP infusions were used. Early institution of regular FFP infusions could have prevented the intracranial hemorrhage but we should establish in each case that they have severe bleeding before used, which carry the risks associated with central venous access and FFP transfusion. Many reported cases of severe factor V deficiency did not have such severe bleeds and only needed protection only before surgery.
The author declares no conflict of interest.
None.
None.

©2021 Doya, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.