MOJ
eISSN: 2381-179X


Case Report Volume 6 Issue 5
1Consultant and chief of pediatrics surgery Department, King Khalid Hospital, Saudi Arabia
2Consultant Histopathology, King Khalid Hospital, Saudi Arabia 3University of Hail, Saudi Arabia
Correspondence: Adel Ahmed Alfayez, University of Hail, Saudi Arabia
Received: April 22, 2017 | Published: May 3, 2017
Citation: Madni M, Seada LS, Alfayez AA, et al. Ectopic left cervical thymic tissue in pediatric age group. MOJ Clin Med Case Rep . 2017;6(5):116-118. DOI: 10.15406/mojcr.2017.06.00175
Objective: We report a case of ectopic cervical thymic tissue in a healthy 5years-11months old girl.
Method: Case report and review of the English-language literature (using PubMed, Ovid, and Proquest databases).
Results: Case of ectopic cervical thymic tissue occurred in a preschool-aged girl to be reported in the English-language literature.
Conclusion: This case raises the alerts of ectopic cervical thymic tissue to be considered in the differential diagnosis of children younger than 10years of age with a painless neck mass. When previously healthy child manifests with a sudden onset of the asymptomatic neck mass, keep in your mind that there is a great likelihood of ectopic thymus tissue in the neck.
Keywords: thymus gland, ectopic tissue, pediatric neck mass, fibrocollagenous tissue, ectopic thymus cyst
Ectopic thymus tissue in the neck remains infrequently described in medical literature. This paper presents the case of a young girl, who presenting with a soft, fluctuating bulk mass on the left side of her neck. The patient underwent complete excision of the lesion and histological inspection showed an ectopic thymic tissue cyst. Ectopic thymic soft tissue may remain an uncommon finding, but it must be involved in the differential diagnosis of neck masses, particularly in children. This case report is complemented by a short review of the relative literature.
The thymus is a major lymphoid tissue in the embryonic stage and early childhood. It mainly appears early in fetal life as well as plays a critical role in the development of cell-mediated immunity. Ectopic cervical thymus is not often reported, for the reason that thymic remnants frequently persist as a symptomatic and unrecognized by clinicians. Most of these lesions arise as a result of migration defects throughout thymic embryogenesis. Since 1901, about 90 cases of aberrant cervical solid and cystic thymic lesions have been reported in the literature and were recognized at either surgery or autopsy.1–3 Approximately two-thirds of all reported cases were identified in children younger than 10years.4 Ectopic thymic tissue in the neck is unusual in patients older than 20years.
A 5-year and 11months old girl, previously healthy, presented in our emergency (ER) department with a left cervical swelling since 4months. It has gradually increased in size and was not associated with fever or weight loss, as the mother mentioned. On examination, the child looked well, with an average body weight, neither pale nor jaundiced. Local examination revealed a left anterior fixed, non-mobile, soft cervical neck mass. No tenderness on palpation. No discharge was coming out and no redness or hotness. After that the patient was admitted in our hospital and investigations were done for her, she underwent surgical excisional biopsy and stayed 4days in the Hospital. The histopathology report came to be “a thymic cyst with multiple foci of ectopic thymus gland tissue"(Figures 1-9).
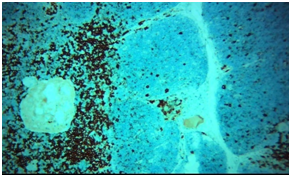
Figure 5 CD20 negative in thymic tissue. Tissue APAAP, red chromogenx200Peroxidase, DAB chromogen x200.
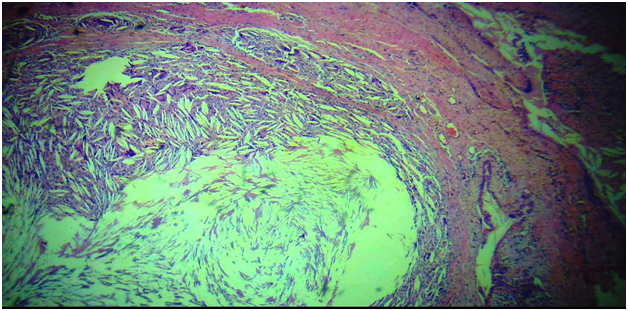
Figure 6 CD20 negative in thymic tissue. Tissue APAAP, red chromogenx200Peroxidase, DAB chromogen x200.
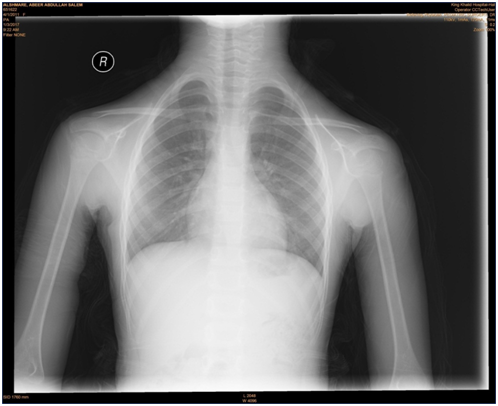
Figure 7 Chest and neck X-ray figure out and confirm that "there is no mediastinal extension of the mass".

Figure 9 Ultrasound of the neck shows large heterogeneous lesion which is seen in the anterior triangle of a left cervical region, between the internal jugular vein and the carotid artery, displacing the carotid anteromedially and the jugular posteriorly; it measured about 3x1.5x1.5cm, it shows heterogeneous hypervascular texture with focal calcification. For clinical correlation and further investigation considering Carotid Space masses (paraganglioma, chwannoma, others).
Gross description
One piece of an irregular nodular, firm soft tissue bit measuring 4x2x1cm. Cut section showed multiple small grayish-white nodules largest measurements. 1x0.5cm and smallest 0.3x0.3cm, multiple bits, 5blocks, all embedded.
Microscopic picture
In multiple bits of the tissue received, multiple cystic spaces are seen, some are rounded others are irregular. Cysts lining ranged from the cubical stratified epithelium. Other cysts form a fibrous capsule. Cysts are filled with huge numbers of multinucleated gains cells and large numbers of cholesterol crystals. Outskirts show multiple foci of thymus gland tissue with a well-formed cortex of packed, monotonous lymphoid T-cells, with tangible body macrophages. Medulla show less packed lymphoid cells. Epithelial whorls of Hassall’s corpuscles are evident. Fibrocollagenous tissue surrounding the cysts show congested capillaries. No evidence of Malignancy.
Differential diagnosis
The differential diagnosis of cervical thymic cyst is broad and includes thyroglossal duct cyst lymphovascular malformations, branchial cleft cyst, and laryngocele, as well as benign tumors (dermoid cysts, epidermoid cysts) and malignant tumors (lymphoproliferative, soft tissue sarcoma and other metastatic lesions).5
Cervical thymus cysts (CTC) are epithelial-lined cysts that most commonly present during the first decade of life, with a slight preponderance towards males.6 Incidences of ectopic thymic tissue in the neck have been reported in various conditions, despite their diversity, there are only a few studies focusing on patients without any thymic disease.7 CTCs can be either congenital or acquired and are most commonly found in the left sided neck, anterior to the SCM, with approximately 50% showing extension into the superior mediastinum.8 Since CTCs represent less than 1% of cystic cervical masses, they are often overlooked in the broad differential diagnosis of children presenting with painless neck masses. It is important, however, for physicians to be able to efficiently and accurately diagnose CTCs since they can usually be surgically excised with little risk of postoperative recurrence.9 The thymus gland is mainly originated from the third and fourth pharyngeal pouches in association with the inferior parathyroid glands. Right and left portions of the thymic primordium descend down the neck during the sixth to eight weeks of gestational life and fuse to form the gland.9 There are three mechanisms for pathogenesis of ectopic thymus in the neck: aberrant descent, sequestration of thymic tissue and failure of involution.10 Most patients with thymic cysts complain of a slowly enlarging, a symptomatic cervical mass. Symptomatic cases of cervical thymic cysts are so rare that this diagnosis is not common preoperatively. In patients with myasthenia gravis, hyperplasia of thymic tissue occurs in their thymus gland and ectopic thymic tissue as well. As a result, the probability of finding ectopic thymic tissue in such a patient is higher than in patients without any thymic disease.7 Diagnosis by fine needle aspiration was appropriately described.11 There has been no reported recurrence and long-term prognosis is excellent.
None.
The author declares no conflict of interest.

©2017 Madni, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.