MOJ
eISSN: 2381-179X


Case Report Volume 12 Issue 2
Faculty of Medicine, Technion, Israel Institute of Technology, Israel
Correspondence: Jochanan Naschitz, Faculty of Medicine, Technion, Israel Institute of Technology, POB 252, Nesher 36602, Derech Hashalom 11, Israel, Tel 073-2-377-300, Fax 97248345575
Received: April 22, 2022 | Published: June 6, 2022
Citation: Naschitz JE, Nesher BB. ECG at the bedside: atrial fibrillation with randomly narrow and wide QRS complexes. MOJ Clin Med Case Rep. 2022;12(2):17-18. DOI: 10.15406/mojcr.2022.12.00411
An electrocardiogram (ECG) displaying atrial fibrillation with randomly narrow and wide QRS complexes, the latter resembling left bundle branch block (LBBB), challenged the physicians’ diagnostic skills. First, Wolf Parkinson White syndrome and ventricular ectopy were excluded based on usual ECG criteria. Pertinent remaining possibilities were functional LBBB and Mahaim type preexcitation. Distinction between the two is made on intracardiac ECG by establishing the chronology of the His and QRS spikes: His spike preceding to QRS is consistent with functional LBBB while an inverted sequence is consistent with Mahaim type preexitation. In the present case invasive testing was judged to be unnecessary and hazardous. The patient was managed safely by slowing the ventricular rate with a beta-adrenergic blocker medication. Digitalis and calcium channel blockers were avoided, in considering their potential to accelerate the conduction through the accessory pathway.
Keywords: atrial fibrillation, pre-excitation, mahaim, left bundle branch block, ventricular tachycardia
An unusual electrocardiogram (ECG) challenged my young colleagues' and my, a veteran's, professional skills. On the background of atrial fibrillation (AF) with 100 bpm ventricular rate the ECG displayed narrow QRS complexes interspersed with wide QRS complex, the latter occurring either isolated or in sequences of 3 - 4 beats. The differential diagnosis between ventricular ectopic and aberrantly conducted beats was important for patient’s management.
A 84-year-old woman was admitted to inpatient rehabilitation having suffered eight days before a stroke. CT revealed a large infarction in the right cerebral hemisphere. CT angiography showed cutoff of the right mid cerebral artery. Because of the patient's late arrival to hospital thrombolytic and endovascular treatment were not implemented. Oral aspirin was started. Relevant in the patient’s medical history were arterial hypertension, dyslipidemia, and mild cognitive impairment. At the time of her transfer to our institution she was alert, her brachial blood pressure while sitting was 122/81 mmHg, the pulse 84 bpm, pulse deficit 15 bpm, and SpO2 93% in the ambient air. There was flaccid paralysis of her left arm and left leg. Results of routine laboratory tests were within the normal range: serum sodium 142 mEq/L, potassium 4.5 mEq/L, LDL-cholesterol 58 mg/Dl, HDL-cholesterol 40 mg/Dl, creatinine 0.77 mg/Dl. The ECG showed AF, previously not diagnosed, with interspersed narrow QRS complexes and wide QRS complexes (Figures 1&2). The patient's usual medications were continued, including atorvastatin 80 mg, lercanidipine 10 mg, ramipril 5 mg and famotidine 20 mg, with aspirin 100 mg added, and later atenolol 25 mg and apixaban 5 mg b.i.d.
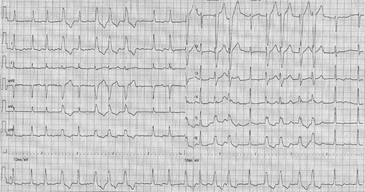
Figure 1 Atrial fibrillation with irregular irregularity of the narrow and wide QRS complexes, the latter occurring as singlets, doublets, and short runs.
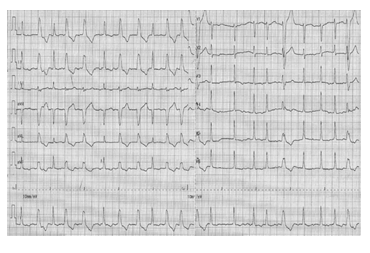
Figure 2 Atrial fibrillation, wide QRS complexes are not preceded by long RR cycles: Ashman sign suggesting aberrant conduction is not present.
The ECG tracings showed 'f' waves 350 per minute and 0.1. mV in amplitude along with an irregular sequence of QRS complexes, typical for AF. The narrow QRS complexes, 0.080 sec in duration and the QRS axis +600, were consistent with normal atrio-ventricular conduction. The randomly wide QRS complexes displaying a left bundle branch block (LBBB) pattern required a differential diagnosis between aberrant conduction and ventricular ectopy. Several possibilities were considered: Wolf Parkinson White syndrome, ventricular ectopic beats along with nonsustained ventricular tachycardia (VT), aberrantly conducted beats, and other preexcitation variants.
Wolf Parkinson White syndrome (WPW) with AF is considered when facing a wide complex tachycardia with irregular QRS cycles and intermittently very short RR intervals. The very short RR intervals in WPW with AF are due to the capability of the bypass tract, in contrast to the atrio-ventricular node, to conduct impulses in extremely rapid and irregular sequence. The slurred or notched upstroke of the QRS complex in WPW is called delta wave; it is caused by the relatively slow conduction through the ventricular muscle from the insertion site of the bypass tract. The QRS complex of preexcitated beats is widened by early stimulation of one ventricle and the later arrival of the excitation to the other. In case the accessory bundle accesses the right ventricle, this aberrant pathway may replicate a LBBB pattern. In the proposito no feature characterizing WPW syndrome was present. Exclusion of WPW syndrome associated with AF was important because the contraindication to use digitalis, which may directly enhance conduction through the bypass tract, as well as verapamil, which may indirectly enhance conduction through the bypass tract by vasodilation and a reflex increase in sympathetic tone.1
Diagnostic criteria for ventricular ectopic beats and nonsustained ventricular tachycardia were examined. When ventricular tachycardia (VT) presents as LBBB-like QRS complexes, distinguishing form aberrantly conducted beats are presence of a ‘q’ wave in lead V6, or in AVR with an initial r or q wave duration >40 ms. None was present in the proposito.2,3 Moreover, irregular irregularity of the RR intervals observed is not a feature of VT.
Aberrantly conducted beats are easily distinguished from VT when a right bundle branch morphology of the wide QRS complexes is present with a triphasic R in lead V1, or a QRS pattern in V6 and concordant initial vector in lead V1 or in more than one ECG leads.4 Aberrant conduction is also favored by a preceding long RR interval followed by an early wide QRS. The latter has been described as the Ashman phenomenon: the earlier in the cycle a premature atrial contraction occurs and the longer the preceding cycle is the more likely it is that the impulse will be conducted with aberration.5
Other preexcitation variants. A bypass tract that connects the right atrium with the right bundle branch is referred to as Mahaim bundle.6 The impulse going down through the Mahaim tract stimulates the right ventricle before arriving to the left ventricle, thereby producing a LBBB pattern. This sequence of ventricular depolarization has been documented on intracardiac ECG under atrial pacing, showing that the paced 'p' wave was followed by an early QRS complex (preexcitated) and subsequently by the His wave (arriving after the physiological delay in the atrio-vetricular node). The ECG in the proposito is consistent with the atrial depolarization being conducted randomly through the atrio-ventricular node (narrow QRS) and through Mahaim fibers (LBBB pattern), either modality exhibiting irregular RR cycles.7 Nevertheless, the diagnosis in the proposito might be challenged by the uncommon observation in a patient having a surface ECG similar to the proposito's while intracardiac ECG during AF showed narrow and wide QRS complexes both preceded by His potentials.8
Interpretation of the patient’s surface ECG allowed to exclude ventricular ectopy and the WPW syndrome. The remaining challenge was to distinguish between functional LBBB (i.e. intermittent aberrant conduction) and Mahaim type preexcitation. A definite diagnosis would be possible on intracardiac ECG in showing the QRS to precede the His spike. Yet, an intracardiac ECG was thought unnecessary for the patient management and hazardous. Slowing of the ventricular rate was attained with a beta-adrenergic blocker. Administration of digitalis or a calcium channel blocker was avoided, taking in consideration existence of Mahaim type preexcitation and the involved risk to accelerate conduction through the accessory bundle. Thus, interpretation of this unusual tracing was advanced to a point necessary for management, when further workup would not benefit the patient.
None.
None.

©2022 Naschitz, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.