MOJ
eISSN: 2381-179X


Case Report Volume 4 Issue 2
Department of General Surgery, Sri Ramakrishna Hospital, India
Correspondence: Sarveswaran Venugopal, Head of Department and Consultant, General Surgery, Sri Ramakrishna Hospital, Tamilnadu- 641044, India, Tel 09842217268
Received: October 23, 2015 | Published: April 1, 2016
Citation: Venugopal S, Subramaniam SK, Kumar A, et al. Disseminated cysticercosis: a rare case report and review of the literature. MOJ Clin Med Case Rep. 2016;4(3):56-58. DOI: 10.15406/mojcr.2016.04.00086
Disseminated Cysticercosis is an unusual manifestation of this common disease especially in the tropical and sub-tropical regions. Till date in English literature, only fewer than 100cases have been reported worldwide so far. Here in we present a case who presented with a relatively asymptomatic sub hyoid lump as a manifestation of disseminated cysticercosis. Although rare, the disseminated form should principally be kept in mind whenever a solitary parasitic cyst is identified. The detailed physical examination of the patient cannot be exaggerated, as exemplified in our case, wherein a subtle sub hyoid swelling led to the detection of a treatable condition like cysticercosis. Disseminated cysticercosis must be kept in the list of the differential diagnosis of any solitary long standing soft tissue swelling especially in endemic areas. A multidisciplinary team approach to the treatment offers better results and minimise complications related to treatment.
Keywords: disseminated cysticercosis, sub hyoid lump, magnetic resonance imaging, taenia solium, antinuclear antibodies
ELISA, enzyme linked immuno sorbent assay; MRI, magnetic resonance imaging; CT, computed tomography; FNAC, fine needle aspiration cytology
Cysticercosis cellulose are the larval forms of the Taenia solium. The definitive and intermediate host are humans and pigs respectively. To develop the disease, the eggs enter into the intestinal lumen through the autoinfection or contaminated eatables. Finally the larval forms spread to the distant sites through the blood stream after crossing the intestinal wall leading to the clinical manifestations.1
Disseminated cysticercosis is an unusual manifestation of this common disease especially in the tropical and sub-tropical regions. Till date in English literature, only fewer than 100cases have been reported worldwide so far.2 Here in we present a case who presented with a relatively asymptomatic sub hyoid lump as a manifestation of disseminated cysticercosis.
A 33year old vegetarian woman from rural part of Tamilnadu presented to our department with a 15day history of lump in the sub hyoid region which had increased in size over last few days. The swelling was otherwise asymptomatic with no specific precipitating or relieving factors. She also revealed recurrent admission to nearby health facility for low grade fever, myalgia and right thigh pain in last few months.
A swelling of about 3x2cm was noted in the sub hyoid region in the subcutaneous plane (Figure 1). No other masses were palpable. General and systemic examination was otherwise unremarkable. Investigations revealed haemoglobin of 13g/dl, total counts of 13,850cells/cu.mm with predominant lymphocytosis and eosinophilia; Erythrocyte Sedimentation Rate of 40mm/hr. In addition, ECG, urine and other routine biochemical investigations were within normal limits. HIV, HbsAg and HCV screening were negative. The tests for Rheumatoid arthritis factor and antinuclear antibodies were normal.

Figure 1 Clinical photograph showing a swelling of about 3x2cm in the sub hyoid region in the subcutaneous plane.
Ultrasound examination of the sub hyoid region showed a 3.3x2.2cm cystic lesion in the subcutaneous plane and an eccentrically placed echogenic solid nodule with curved structure within it with surrounding inflammatory tissue changes. Findings suggested a possibility of cysticercosis (Figure 2). Furthermore, stool and blood Enzyme Linked Immuno Sorbent Assay (ELISA) were ordered and were normal and positive for Cysticercosis antibody respectively.
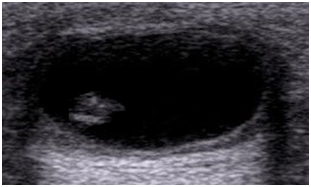
Figure 2 Ultrasonography of the neck region showing a well-defined thick walled 3.3x2.2cm anechoic cystic lesion in the subcutaneous plane with posterior acoustic enhancement and an eccentrically placed echogenic solid nodule within it with surrounding inflammatory tissue changes.
An excision biopsy of the swelling was done. On gross examination, the specimen showed a firm cyst surrounded by pale fibrous tissue. Cut section showed clear fluid filled cavity with a curved structure attached to the cyst wall. Microscopically, the cyst was surrounded by dense fibrous two layered wall showing lymphocytic infiltration. The tiny nodule contained within the cyst exhibited a coiled parasite within a connective tissue capsule (Figure 3). The diagnosis of subcutaneous cysticercosis was made.

Figure 3 Low power microscopy photograph showing a cross section of cysticerci entrapped in a fibrous capsule and surrounded by dense fibrous two layered wall showing lymphocytic infiltration and granulomatous reaction.
Orthopaedic colleague was consulted for thigh pain and Magnetic Resonance Imaging (MRI) was suggested for recurrent pain and low grade fever. MRI of both thigh regions revealed multiple tiny hyper intense lesions with perilesional edema and rim enhancement in T2 weighted images, consistent with cysticercosis lesions. A whole body MRI showed multiple such lesions all over the body (Figure 4).

Figure 4 A whole body MRI image showing the typical rice grain likes lesions all over the body- typical 'starry sky' appearance seen in disseminated Cysticercosis.
Her family members were screened negative for cysticercosis by means of Stool examination and Blood ELISA for cysticercosis antibody. A multi-disciplinary team planned the treatment for the patient. She was primed with steroids one week prior to the initiation of cysticidal drugs. Later albendazole therapy was initiated at a dose of 15mg/kg for a period of 30days. The patient was observed at the hospital for 5days after initiation of the cysticidal drugs.
On follow-up after four months, no new lumps were reported and her myalgia had also improved significantly.
Human cysticercosis is caused by the dissemination of the larval forms of Taenia solium from the intestine via the blood stream to the organs and tissues of the body. The organs most commonly affected are the subcutaneous tissue, skeletal muscle, lung, brain, eye, liver and occasionally the heart. This may involve almost any organ of the body. Widespread dissemination of cysticerci throughout the body was reported as early as 1912 by the British Army medical officers stationed in India.3 In 1926, Priest described probably the first case of disseminated Cysticercosis in a British soldier who had epileptic seizures, mental dullness, swelling of his muscles and widespread subcutaneous nodules. In 1961, a review of 450 cases of cysticercosis by Dixon and Lipscomb reported only one case of dissemination.4 Kumar et al. 5 & Wadia et al.6 reviewed 22 cases each.
The clinical features depend on the cyst burden, viability of the cyst, the host reaction and more importantly their location. The syndrome of disseminated cysticercosis is characterized by pseudomuscular hypertrophy (100%), palpable subcutaneous nodules (87%), seizures (78%) and abnormal mentation.1,3 Subcutaneous cysticercosis may cause painful or painless subcutaneous nodules. There is diffuse symmetrical painful or painless enlargement of all groups of muscles associated with weakness and easy fatigability. Clinically, soft tissue cysticercosis can be misdiagnosed as abscess, lipoma, tuberculous lymphadenitis, epidermoid cyst, pyomyositis, neuroma, sarcoma, neuro fibroma, ganglion, myxoma, or fat necrosis.5 Although our patient had diffuse cerebral and muscular involvement, there was no significant hypertrophy and she was without associated symptoms except for the swelling in the sub hyoid region and myalgia.
Ultrasonography is the most reliable initial diagnostic modality of choice for a soft tissue swelling. An eccentrically located cyst with a hyper echoic scolex within and surrounding mild edema is the usual appearance of soft tissue cysticercosis on ultrasonography.
Computed tomography (CT) scans and Magnetic Resonance Imaging (MRI) are useful adjuvants in anatomical localization of the disease. MRI is more sensitive than CT as it identifies live forms, scolex and the response to treatment. Non enhanced CT scans of muscles can show innumerable cysts standing out contrasting against the background of muscle mass in which they are embedded.5 Cysticercosis is seen as a cystic lesion that appears hypo intense on T1weighted and hyper intense on T2 weighted images. Peripheral rim enhancement of the cyst wall is commonly due to reactive edema. Cysts within the muscles are arranged in the direction of the muscle fibers. Within the hyper intense cyst, the scolex is appreciated as a tiny hypo intense speck.7 In our patient the MRI scan had a typical ‘starry sky’ appearance but did not reveal any calcified foci in muscles.
The diagnosis of cysticercosis can be ascertained by fine-needle aspiration cytology (FNAC) or biopsy, which shows the scolex, fragments of the spiral wall and the detached hooklets of Cysticercosis cellulosae. Sometimes, only an inflammatory reaction consisting of large numbers of eosinophils and histiocytes can be seen.
Serological tests are used to confirm the diagnosis, especially by detecting antibodies against cysticercosis. Enzyme-linked immunoblots assay is more sensitive and specific than ELISA.8 The blood ELISA in our case was positive. Sensitivity of serological tests tends to be substantially lower for patients with a single cyst or calcified cysts and high for patients with multiple cysts (94%).9
Pharmacological management with the cysticidal drugs praziquantel (10–15mg/kg/day for 6–21days) and albendazole (15mg/kg/day for 30days) help by reducing the parasite burden. Cysticercosis is a serious disease with potentially life-threatening complications. These drugs hasten the death of the cysts, which even in the absence of such treatment may occur.10 It is recommended that all patients with multiple cysts should receive treatment with cysticidal drugs. There is no role for cysticidal drugs in inactive cysticercosis, i.e. calcified cysts, because the parasites are dead.5 Pharmacological treatment may be associated with severe reactions, which occurs as a consequence from massive release of antigens causing local tissue swelling, generalized anaphylactic reaction and enlargement of cysts. Before starting the cysticidal drugs, priming with corticosteroids decreases the incidence of such complications.8 Efficacy of treatment should be monitored at regular intervals.6
Since it is a common soft tissue infection in endemic region like southern Indian peninsula, clinicians should always consider cysticercosis in the differential diagnosis whenever a patient presents with painful or painless subcutaneous swelling of long duration. Although rare, the disseminated form should principally be kept in mind whenever a solitary parasitic cyst is identified. The detailed physical examination of the patient cannot be exaggerated, as exemplified in our case, wherein a subtle sub hyoid swelling led to the detection of a treatable condition like cysticercosis.
A high degree of suspicion of disseminated cysticercosis must be kept in the list of the differential diagnosis of any solitary long standing soft tissue swelling especially in endemic areas. In addition to the rarity they are also difficult to suspect and diagnose clinically. The investigations need to be tailored to arrive at relevant diagnosis so as to plan the therapy. A multidisciplinary team approach to the treatment offers better results and minimise complications related to treatment. Patients who are on treatment and who have active cysts require periodic follow ups as they remain at risk of serious complications.
None.
The author declares no conflict of interest.

©2016 Venugopal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.