MOJ
eISSN: 2381-179X


Case Report Volume 6 Issue 5
1Department of Anaesthesia, Dr. R.P. Govt. Medical College Kangra, India
2Department of Anaesthesia & Intensive care, PGIMER, India
3Department of Paediatric surgery, PGIMER, India
4Department of Surgery, Dr. R.P. Govt. Medical College, India
5Department of Surgery, Dr. R.P. Govt. Medical College, India
Correspondence: Rajesh Chaudhary, MS, Senior Resident, Department of Surgery, Dr. RP Govt. Medical College, India
Received: March 25, 2017 | Published: May 8, 2017
Citation: Mahajan M, Mathew PJ, Menon P, et al. Cinical presentation of foreign body aspiration in children -an observational study. MOJ Clin Med Case Rep . 2017;6(5):120-125. DOI: 10.15406/mojcr.2017.06.00176
Introduction: Aspiration of foreign body (FB) is a life threatening situation in children. A strong suspicion depending upon clinical presentation can lead to early diagnosis and treatment leading to decreased complication and mortality. This study was conducted to observe the clinical presentation of children undergoing rigid bronchoscopic removal of inhaled foreign bodies under general anaesthesia at a tertiary health care centre in north India.
Method: A total of 72 bronchoscopic procedures were done in 71 children during the study period from August 2014 to July 2015. Preoperative demographic data, time interval between aspiration and admission, circumstances of aspiration, suspected type and site of FB, clinical presentation of children presented with suspected FB aspiration was evaluated. All the children underwent rigid bronchoscopy under general anaesthesia using controlled mode of ventilation.
Result: Incidence of foreign body aspiration was more in male patients (70.4%). Most of the children (80.3%) were ≤3years of age. Most common FB was peanut, found in 42(59.1%) children. FB was predominately located in right bronchus in 37(52.1%) children. Playing and eating were the most common activities found in 34(47.9%) and 32(45.1%) of children respectively. Most common presenting symptom in our study was cough in 49(68.1%) cases, followed by noisy breathing/wheeze in 26(36.1%) cases. Air entry was decreased in 53(73.6%) cases and hyperinflation was the most common chest X-ray finding in 44(61.1%) children.
Foreign body (FB) aspiration is a life threatening situation in children. Asphyxiation from inhaled foreign bodies is among the five leading causes of accidental deaths in children.1 Approximately 80 percent of FB aspirations occur in children younger than three years, with the peak incidence occurring between one and two years of age.2 Children are more prone for foreign body aspiration at this age, because most children are able to stand and move around, are apt to explore their world via the oral route, and also have the fine motor skills to put small objects into their mouths, but they do not yet have molars to chew the food adequately. Young children are also particularly vulnerable to FB aspiration because of the smaller diameter of their airway, which is prone to obstruction. The effects of FB inhalation can vary from the nonspecific symptoms of coughing, wheezing, fever, and dyspnea to life threatening obstruction and death. Prompt and early FB removal by rigid bronchoscopy under general anaesthesia is essential for reducing the resulting complications and mortality.
This study was conducted at the Department of Anaesthesia and Intensive care and Department of Paediatric Surgery, Advanced Paediatric Centre at PGIMER, Chandigarh during the study period from August 2014 to July 2015. After approval by our institutional ethics committee and obtaining informed consent of the parents, this prospective observational study was conducted to evaluate the clinical presentation of 71 children with positive bronchoscopy for removal of airway FB aspiration. One child underwent bronchoscopy twice in two separate admissions to retrieve the same FB, so number of bronchoscopes included in our analysis was 72 in 71 children. Pre-operatively, relevant clinical information such as age, gender, time of suspected aspiration, mode of aspiration, signs and symptoms, duration of clinical picture, FB type, FB location and other comorbidities were evaluated. Preoperative AVPU (Alert, responds to voice, responds to pain, unresponsive) paediatric response scale, chest X-ray and other relevant investigations were also noted. All the children underwent rigid bronchoscopy under general anaesthesia using controlled mode of ventilation.
Tracheobronchial foreign bodies constitute a life threatening clinical entity encountered in the paediatric age group. Out of the 72 procedures performed, 40(55.5%) bronchoscopes were done during winter months in November, December and January (Table 1). One child presented twice: first in December and then again in January.
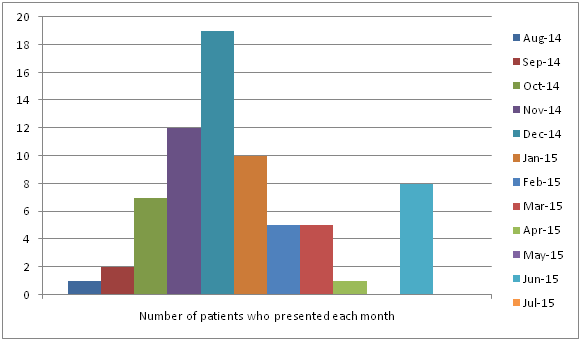
Figure 1 Monthly distribution of rigid bronchoscopies performed for removal of airway FB
*One child presented twice: first in December and then again in January.
The aspiration of FB was clearly witnessed by an adult in 58(81.7%) children including the child that presented twice for bronchoscopy. In 4(5.6%) children, the FB was suspected based on circumstantial evidences at the time of onset of symptoms, like, child was playing with the suspected FB and the adult recollected the sudden onset of symptoms from a definite time point. Therefore, we have categorized these 4 children as strongly suspected cases based on circumstantial history. There was no definite history of witnessing or a strong reason to suspect aspiration of FB in remaining 9(12.6%) children. However bronchoscopy was done either to rule out a FB or due to suspicion of FB based on the clinical presentation. The mean age of presentation of all children was 27.32+26.85months (range: 6months to 120months). Fifty seven (80.3%) children were less than 3years of age, and 14(19.7%) children were more than 3years of age. Most of aspirations were found in male patients 50 (70.4%) (Table 2).
Variable |
Total children(n=71) |
Strongly suspected of aspiration(n=4) |
Foreign body aspiration not witnessed(n=9) |
Age(months)(mean+SD) |
27.32+26.85 |
36+33.94 |
31.33+31.68 |
Number of children with ageless than 3years (%) |
57(80.3%) |
3(75.0%) |
7(77.8%) |
Number of children more than 3years of age (%) |
14(19.7%) |
1(25.0%) |
2(22.2%) |
Sex |
|||
Male (%) |
50(70.4%) |
3(75.0%) |
6(66.7%) |
Female (%) |
21(29.6%) |
1(25.0%) |
3(33.3%) |
Table 2 Demographic data of patients
The average interval between aspiration and admission to PGIMER was 4402.82±16726.73 minutes with a range of85 to 56904minutes and median of 1404minutes (Table 3). Amongst the 71 children, 31(43.6%) children presented within 24hours of aspiration. One child presented after 7days of aspiration of FB (Table 3). Out of total 71 patients, 36(50.7%) were referred from other hospitals wherein 2 children were subjected to bronchoscopy and 5 children were subjected to GI endoscopy for attempted removal of FB in the previous hospitals. Another patient had bronchoscopy twice at PGIMER on two separate occasions for the same FB aspirated. On admission to PGIMER, 69 children were alert, one child who presented twice was alert during both the admissions, i.e. 69 children were alert out of 70(97.2%) at the time of presentation. One (1.4%) patient was not alert but was responding to voice and another patient was responding only to pain. Increased work of breathing was present in 43(59.7%) patients at time of admission. The baseline percentage saturation of oxygen in blood (SpO2) among the patients in emergency ranged from 40-100% with a median of 94% and interquartile range of 90-96.5%. Seven patients presented in emergency with SpO2 less than 90% without oxygen supplementation. Out of those seven patients, one patient who was not alert but responding only to pain was intubated in emergency due to increased respiratory distress and shifted to ward. The oxygen saturation improved with the supplemental oxygen in the other six patients in emergency and were transferred to either operation theatre or ward on oxygen.
Variable |
Total Children(n=71)* |
Actually witnessed aspiration(n=58) |
Strongly suspected of aspiration(n=4) |
Foreign body aspiration not witnessed(n=9) |
Time between aspiration and admission to hospital (minutes) (mean+SD) |
4402.82+16726.73 |
4545.09+17282.14 |
2342+2750.57 |
Unknown |
Number of children who presented within 24hours |
31(43.7%) |
29(50.0%) |
2(50.0%) |
0# |
Number of Children who presented during 1-7days |
33(46.4%) |
28(48.3%) |
2(50.0%) |
3(33.3%)# |
Number of Children who presentedafter 7days |
7(9.8%) |
1(1.7%) |
0 |
6(66.7%)# |
Number of children referred from another hospital |
36(50.7%) |
27(46.5%) |
3(75%) |
6(66.7%) |
Table 3 Admission data
*One child had undergone bronchoscopic procedure twice during two separate admissions
#Duration of symptoms has been taken to calculate the parameter.
Playing was the most common activity during aspiration of FB in 34(47.8%) children (Table 4). Most common suspected location of FB was in the right bronchus i.e. in 39(54.9%) children. Vegetable foreign bodies were suspected in 53(74.6%) children, among which nuts were most commonly suspected, i.e. in 39(54.9%) cases (Table 5).
Variable |
Total children(n=71) |
Strongly suspected of aspiration(n=4) |
Foreign body aspiration not witnessed(n=9) |
|
Activity of child during suspected aspiration |
||||
Eating |
22(31.0%) |
1(25%) |
0 |
|
Playing |
24(33.8%) |
2(50%) |
0 |
|
Eating and playing |
10(14.1%) |
1(25%) |
0 |
|
Running |
2(2.8%) |
0 |
0 |
|
Whistling |
2(2.8%) |
0 |
0 |
|
Writing |
2(2.8%) |
0 |
0 |
|
Activity not known |
9(12.7%) |
0 |
9(100%) |
|
Suspected location of foreign body |
||||
Right Bronchus |
39(54.9%) |
3(75%) |
6(66.7%) |
|
Left Bronchus |
18(25.3%) |
1(25%) |
2(22.2%) |
|
Trachea |
12(16.9%) |
0 |
1(11.1%) |
|
Site of foreign body not identifiable |
2(2.8%) |
0 |
0 |
|
Table 4 Preoperative foreign body data
Variable |
Total children(n=71) |
Actually witnessed aspiration(n=58) |
Strongly suspected of aspiration(n=4) |
Foreign body aspiration not witnessed(n=9) |
Suspected foreign body |
||||
Vegetative |
53(74.6%) |
49(84.5%) |
4(100%) |
0 |
Peanut |
31(43.6%) |
28(48.3%) |
3(75%) |
0 |
Almond |
7(9.8%) |
6(10.3%) |
1(25%) |
0 |
Pomegranate seed |
2(2.8%) |
2(3.4%) |
0 |
0 |
Betel nut |
1(1.4%) |
1(1.7%) |
0 |
0 |
Cashew nut |
1(1.4%) |
1(1.7%) |
0 |
0 |
Chana |
5(7.0%) |
5(8.6%) |
0 |
0 |
Rajmah |
1(1.4%) |
1 |
||
Seed |
1(1.4%) |
1 |
||
Bengal gram |
1(1.4%) |
1(1.7%) |
||
Chicken bone |
1(1.4%) |
1(1.7%) |
0 |
0 |
Grass |
1(1.4%) |
1(1.7%) |
0 |
0 |
Raw Rice |
1(1.4%) |
1(1.7%) |
0 |
0 |
Non vegetative |
9(12.7%) |
9(15.5%) |
||
Pen Cap |
2(2.8%) |
2(3.4%) |
0 |
0 |
Plastic Whistle |
2(2.8%) |
2(3.4%) |
0 |
0 |
Soil |
2(2.8%) |
2(3.4%) |
0 |
0 |
Metal Piece |
1(1.4%) |
1(1.7%) |
0 |
0 |
Nail Polish Brush |
1(1.4%) |
1(1.7%) |
0 |
0 |
Light emission diode Pin |
1(1.4%) |
1(1.7%) |
0 |
0 |
Table 5 Suspected foreign body data
After admission the children were taken up for bronchoscopic removal of foreign body at an interval of 722+1379.79minutes (range: 12minutes to 8482minutes) with a median of 456minutes. During preanaesthetic checkup, we found that cough was the most common presenting symptom in 49(68.1%) cases, followed by noisy breathing/wheezing in 26(36.1%) children. Air entry was decreased in 53(73.6%) children, tachypnea (increased respiratory rate according to age) was present in 36(50.0%) children and tachycardia (increased heart rate according to age) was present in 50(69.4%) children. Chest X-ray showed hyperinflation in 44(61.1%) cases (Table 6). One child who presented twice, initially presented with history of cough, cyanosis and respiratory difficulty, with normal chest X-ray, but with witnessed FB aspiration by an adult. In first bronchoscopy FB could not be retrieved, child improved with antibiotics, bronchodilators and steroid nebulization. After improvement he was discharged to be followed up in OPD. Postoperative chest X-rays showed infiltration. After approximately one month child presented again with cough, respiratory difficulty, hyperinflation of right side on chest X-ray. He was readmitted and repeat bronchoscopy was done.
Variable |
Total(n=72) |
Actually witnessed aspiration(n=59) |
Strongly suspected of aspiration(n=4) |
Foreign body aspiration not witnessed(n=9) |
Sign and symptoms |
||||
Symptoms |
||||
Cough |
49(68.1%) |
38(64.4%) |
3(75%) |
8(88.9%) |
Noisy breathing/wheezing |
26(36.1%) |
24(40.7%) |
0 |
2(22.2%) |
Fever |
13(18.1%) |
11(18.6%) |
0 |
2(22.2%) |
History of choking |
12(16.7%) |
9(15.3%) |
2(50.0%) |
1(11.1%) |
Irritable |
5(6.9%) |
5(8.5%) |
0 |
0 |
Cyanosis/bluishness |
5(6.9%) |
5(8.5%) |
0 |
0 |
Vomiting |
4(5.6%) |
4(6.8%) |
0 |
0 |
Excessive crying |
4(5.6%) |
3(5.1%) |
0 |
1(11.1%) |
Signs |
||||
Subcostal retraction |
23(31.9%) |
19(32.2%) |
2(50.0%) |
2(22.2%) |
Nasal flaring |
11(15.3%) |
8(13.6%) |
1(25.0%) |
2(22.2%) |
Intercostal retraction |
8(11.1%) |
7(11.9%) |
1(25.0%) |
0 |
Accessory muscleuse |
1(1.4%) |
1(1.7%) |
0 |
0 |
Suprasternal retraction |
3(4.2%) |
3(5.1%) |
0 |
0 |
Increased work of breathing |
43(59.7%) |
36(61.0%) |
3(75.0%) |
4(44.4%) |
Auscultation |
||||
Crepts |
28(38.9%) |
21(35.6%) |
3(75.0%) |
4(44.4%) |
Wheeze |
22(30.6%) |
19(32.2%) |
1(25.0%) |
2(22.2%) |
Crepts+ wheeze |
9(12.5%) |
7(11.9%) |
0 |
2(22.2%) |
Chest expansion/air movement |
||||
Air entry decreased |
53(73.6%) |
41(69.5%) |
4(100%) |
8(88.9%) |
Hyper resonant chest |
1(1.4%) |
0 |
0 |
1(11.1%) |
Variable |
Total(n=72) |
Actually witnessed aspiration(n=59) |
Strongly suspected of aspiration(n=4) |
Foreign body aspiration not witnessed(n=9) |
Chest X-ray |
||||
Hyperinflation |
44(61.1%) |
35(59.3%) |
2(50.0%) |
7(77.8%) |
Foreign body visualized |
8(11.15) |
6(10.2%) |
1(25.0%) |
1(11.1%) |
Consolidation |
2(2.8%) |
1(1.7%) |
0 |
1(11.1%) |
Collap selung |
5(6.9%) |
5(8.55) |
0 |
0 |
Pneumothorax, Pneumo mediastinum and Subcutaneous emphysema |
1(1.4%) |
1(1.7%) |
0 |
0 |
Table 6 Preanaesthetic clinical presentation data
One child who was responding to voice at admission deteriorated to become unresponsive due to cardiorespiratory arrest and was revived after 2 cycles of CPR, intubated and shifted to operation theatre on ionotropes and on assisted ventilation.
Among 71 children enrolled in our study, 40(56.3%) children presented during wintermonths in November, December and January. This may reflect the eating habits of children in this part of country in winters as also observed by Gulati et al.3 Majority of children i.e 80.3%, were below 3years of age, with mean age of 27.32months. Similar observations were made in other studies.4–6 Children in this age group are more vulnerable because of development of ability to stand and move around, tendency to use their mouth to explore the surroundings, lack molars, incomplete coordination between chewing and swallowing and lack of close supervision. FB aspiration was predominant in male children i.e.70.4%, as corroborative with other studies.4,5,7 Although there was clear witness of aspiration of FB by an adult in 58(81.7%) children and another 4 (5.6%) children had circumstantial evidence in our study, aspiration of FB was not witnessed in 9(12.6%) children. Gang et al.,6 had observed clear witnessed history in 73.8% cases while 26.2% did not have clear history of FB aspiration,6 although Naragund et al.,7 noted definitive history only in 36.4% cases, while 65.6% cases were unwitnessed7. So even if unwitnessed, a diagnosis of FB should be kept in mind when dealing with respiratory diseases if other signs and symptoms of FB aspiration are present. Physical activities like playing and eating were most common activities during aspiration as supported by Foltran et al.8 The propensity of children to talk, laugh, and run while chewing also increases the chance that a sudden or large inspiration may occur with food in the mouth. In our study there were 31(43.7%) children who presented within 24hours and 40(56.3%) children presented after 24hours. Tomaski et al.,9 observed 60% presentation whereas Maddali et al.,10 observed 44% presentation within 24hours. Delayed diagnosis of FB may be due to variable clinical history and clinical findings, delay in seeking treatment by parents and misdiagnosis by clinicians. Since ours is a tertiary centre in this region and most of these cases are referred from other hospitals, delay in referral and transportation also play a role in delayed presentation of these children to this institute. In our study 36(50.7%) cases were referred from other hospital. FB aspiration is a life threatening situation, so early diagnosis and treatment plays a crucial role in the management of these children. Vegetable foreign bodies were found in 60(84.5%) cases, although these were suspected in 53(74.6%) cases based on history. Peanut was the most common vegetable FB in 42(59.1%) patients. Fidkowski et al.4 Boufersaoui et al.,5 Kaur et al.,11 had similar finding. Groundnut/peanut was the most common airway FB in winter months because it is quite cheap and commonly eaten commodity and is usually given to appease crying children by their ignorant parents realising little of its potential of airway aspiration. Among 12(16.9%) non-vegetable FB, pen caps were removed in 3(4.2%) children. Type of FB aspirated reflect the eating habit of people around the world, peanut in china, dry pumpkin seed in Greece, watermelon seed in Egypt, head scarf pins in Turkish are most commonly aspirated.12,13 Vegetable FB absorb water and subsequently change partial obstruction to complete obstruction. They also release chemical that lead to surrounding tissue reaction leading to chemical bronchitis with fever and chest infection. Non vegetable FB produces few sign and symptoms and may present later until they become obstructive causing emphysema or atelectasis.
In our study, FB was mostly found in right bronchus in 39 (54.9%) children as compared to left bronchus in 21(29.6%) children. Sinha et al.,14 Fidkowski et al.,4 Kaur et al.,11 had similar finding. Whereas Naragund et al.,7 found no significant difference between FB aspiration in right and left bronchus,7 Liu et al found predominance of FB aspiration in left bronchus in 60% children.15 Most common presenting symptom in our study was cough in 49(68.1%) cases, followed by noisy breathing/ wheeze in 26(36.1%) cases. Increased work of breathing was present in 43(59.7%) cases. Naragund et al.,7 found cough in 90.9% cases, wheeze in 90.9% and respiratory distress in 72.7% cases.7 Similarly Kaur et al observed cough in 92% cases, respiratory distress in 80% cases and wheeze in 64% cases.11 A history of cough is highly sensitive but not very specific for aspiration of FB as observed by Fidkowski et al.4 They also found that a history of cyanosis and stridor is very specific for FB aspiration but is not very sensitive4. Air entry was decreased in 53(73.6%) cases. Similar finding was observed by Naragund et al.,7 in 72.7% children and Kaur et al.,11 in 72% children. The classical triad of presentation cough, wheeze and decreased air entry should raise the suspicion of airway FB in children presenting with respiratory distress. Chest X-ray is the most common and readily available investigation to confirm the diagnosis. In our study we observed hyperinflation in 44(61.1%) children as the most common finding that is consistent with review done by Fidkowski et al.4 There was single mortality (1.4%) in our study. Kaur et al.,11 had observed 2% mortality and Sahin et al.,16 found mortality of 0.8%. Thus the risk of serious complications caused by retained FB outweighs the low morbidity associated with rigid bronchoscopy done for airway FB removal. Rapid, accurate diagnosis and timely intervention to remove the FB are important prerequisite to reduce the complications and mortality caused by aspiration of tracheobronchial FB.
Tracheobronchial foreign bodies constitute a serious and potentially fatal situation usually occurring in children. The classical triad of presentation –cough, wheeze and decreased air entry should raise the suspicion of airway FB in children presenting with respiratory distress. Besides this classical triad, hyperinflation of chest on X-ray in a male child of less than three years produces a strong suspicion of foreign body aspiration. Rigid bronchoscopy should be done in all the children with classical signs and symptoms, even if not witnessed, as risk of serious complications caused by retained FB outweighs the low morbidity associated with rigid bronchoscopy done for airway foreign bodies.
All the authors Contributed substantially to the Conception, design, Acquisition of data, Analysis and interpretation of data, drafting the article, Critical revision of the article and final approval of the version to be published.
None.
The author declares no conflict of interest.

©2017 Mahajan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.