MOJ
eISSN: 2381-179X


Case Report Volume 3 Issue 3
Department for Orthopaedic Trauma, University of Ulm, Germany
Correspondence: Andreas Schicho, Department for Orthopaedic Trauma, University of Ulm, Albert-Einstein-Allee 23, D-89081 Ulm, Germany, Tel +49 (0)731 500-54571
Received: October 29, 2015 | Published: December 1, 2015
Citation: Schicho A, Riepl C, Scola A. Brook’s wiring for treatment of an atlanto-axial dislocation and odontoid fracture in a child. MOJ Clin Med Case Rep. 2015;3(3):234-237. DOI: 10.15406/mojcr.2015.03.00067
Background: Upper cervical spine injuries are rarely seen in children. Distinct anatomic properties make head and neck susceptible to hyperflexion movements.
Method: We here report the case of a 5-year-old boy, who sustained a combined atlanto-axial dislocation and odontoid fracture in a high-speed car accident.
Results: Closed reduction and tension wiring according to Brook's procedure showed good anatomic and functional results with no neurologic squealae. Complementary, we discuss anatomical properties of the child body relevant for head and neck injuries, their classification and show therapeutic options and strategies.
Conclusion: Rare injuries such as fractures at the upper cervical spine require a vast knowledge of therapeutic strategies. Both conservative and surgical approaches are possible.
Level of evidence: IV–V
Keywords: upper cervical spine, pediatric, atlanto-axial dislocation, odontoid fracture, brook's technique, hyperflexion, brook’s wiring, synchondrotic fracture, neck, odontoid process, atlantoaxial, synchondrosis
EP, emphysematous pyelonephritis; DKA, diabetic ketoacidosis; CT, computed tomography
Cervical spine injuries are rarely seen in children with an overall incidence of about 1-1.5%.1,2 In pediatric cervical spine injury, the upper cervical spine is the most common site affected (52% of cases).2 The typical injury mechanisms for pediatric cervical spine injuries are hyper flexion movements as in motor vehicle accidents, because of distinct anatomic properties of a child’s body, like an increased head-to-body ratio.3,4 We here report the case of a 5-year-old boy, who sustained a severe hyperflexion trauma of the cervical spine in a high-speed car accident (approx. 60 mph). Computed tomography (CT) and magnetic resonance imaging (MRI) showed a complete atlanto-axial dislocation with synchondrotic fracture of the odontoid process.
In February 2013, a 5-year-old boy was a restrained passenger in a high-speed car crash with presumed high-force impact. Neither initial nor delayed unconsciousness were reported. He was responsive on scene, with neck pain and loss of head rotation. He was immobilized with stiff neck and spine-board and admitted to the emergency department of our hospital.
Diagnosis
Examination showed a glascow coma score (GCS) of 15 with pupils equal, round, reactive to light and accommodation. He was responsive and alert on scene but couldn’t remember what has happened. The primary survey showed no disabilities or signs of head, chest, abdominal, pelvic or extremity injury. Both loss of head rotation and neck pain persisted. No abdominal damage aroused from sonographic assessment. We decided to perform a computed tomography (CT) of his head and neck to rule out intracerebral bleeding and fractures. Standard and 3D reconstructions revealed an atlanto-axial dislocation with a displacement of the atlas >5mm, a fracture of the odontoid process with a ventral axis tilt of 22° (Figure 1) and no signs of intracerebral bleeding. A following MRI scan Figure 2 showed ruptures of the interspinous ligaments from C2 to C6 with intact alar ligaments. The spinal cord showed no signs of damage. These findings lead to the diagnosis of an atlanto-axial-dislocation with synchondrotic fracture of the odontoid process in a neurologically intact 5-year-old boy.
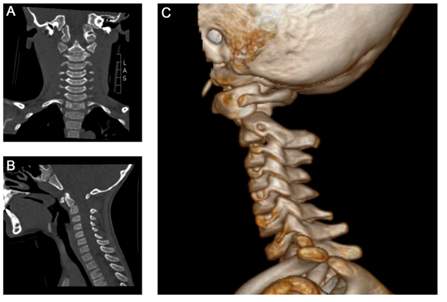
Figure 1 A) Polytrauma computed tomography. A) Coronal view showing the fracture at the synchondrotic level. B) Sagittal view with 22° ventral deviation of the odontoid fragment. C) 3D-reconstruction showing ventral dealignment of the atlanto-axial-joint and increased C1-C2 interspinous distance.
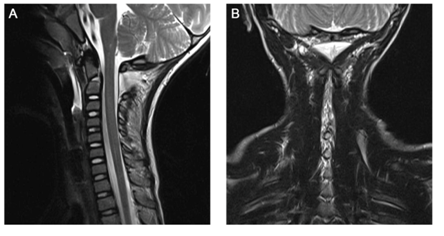
Figure 2 Preoperative magnetic resonance imaging. A) Sagittal view of T2-weighted scan showing rupture and edema in the interspinous ligaments. B) Coronal view of T2-weighted scan with high-level signal along the interspinous ligaments and the C1-C2 facet joint on both sides.
Treatment
The patient was transferred to the operating room for closed reduction and internal fixation with two tension wires and a bone allograft according to the Brook’s procedure. The atlas was reduced during surgery by manual hyperextension of the head, also tilting up the ventrally deviated odontoid process. Fluoroscopy showed realignment of the odontoid process and anatomic reduction of the atlanto-axial joint. A bone-allograft from the pelvis was interponed and the intact laminae of atlas and axis were fixed by two tension wire loops. Control computed tomography before weaning showed anatomic reduction of both, the odontoid fracture and the C1-C2-dislocation (Figure 3).
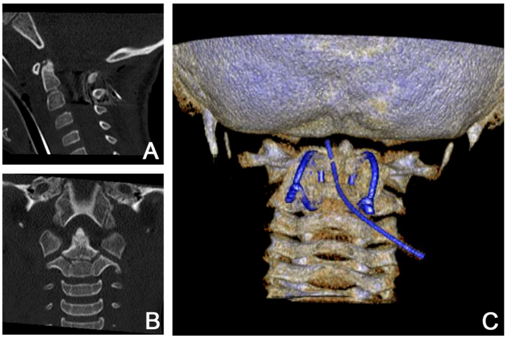
Figure 3 Postoperative computed tomography with Brook’s tension wiring. A) Sagittal reonstruction showing realignment of the odontoid process and narrowed C1-C2 interspinous distance. B) Coronal view with intact facet joint alignment and central odontoid process. C) 3D-reconstruction with two paramedian C1-C2 tension wires and a 8-mm drain.
Postoperative course
Throughout his stay on the ward, the patient remained neurologically intact, suffered no complications and was dismissed pain free after 8days (Figure 4). After six weeks of immobilization with three weeks each in a Miami-J-collar and a soft collar, the boy had regained good range of motion and was free of pain with no neurologic disabilities. Roentgen graphic controls showed no dislocation (Figure 5) and good functional results. Three month after trauma, the range of motion was flexion/extension 40/0/35°, lateral bending left/right 40/0/40° and rotation left/right 80/0/80°. The tension wires were removed six month after fusion without complications (Figure 6). Another four weeks later the range of motion was flexion/extension 70/0/80° with no chin-to-sternum-distance left, lateral bending left/right 70/0/70° and rotation left/right 80/0/90° (Table 1).

Figure 5 Functional radiographs. A) AP-view in neutral position. B) Lateral view of head flexion. C) Lateral view of head extension.
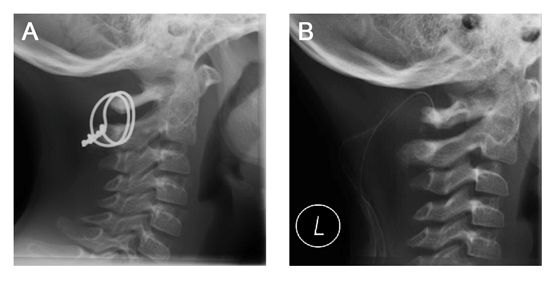
Figure 6 Lateral view x-ray before and after removal of tension wires. A) Before removal, 3month after trauma. B) After removal, with an 8-mm drain in situ.
Class 1 |
Gas confined to the collecting system |
Class 2 |
Gas confined to the renal parenchyma alone |
Class 3A |
Perinephric extension of gas or abscess |
Class 3B |
Extension of gas beyond the Gerota fascia |
Class 4 |
Bilateral EP or EP in a solitary kidney |
Table 1 Huang and Tseng classification of EP CT scan findings (2000)
We here report a case of complete atlanto-axial-dislocation with fracture of the odontoid process in a 5-year-old boy who was dismissed from hospital without neurologic sequelae after8 days. He now is neurologically intact with a good functional outcome. Although cervical spine injuries in children are rarely seen with an overall incidence of 1-1.5%,1,2 the upper cervical spine is affected most commonly in spine injuries. In pediatric patients with blunt trauma, the associated mortality rate is almost 6-fold higher when the upper cervical spine is injured.1 Imaging studies have to be obtained whenever appropriate; according to the NEXUS instrument,2 tenderness and distracting injury are the most common abnormalities in pediatric cervical spine patients. In the here reported case, the patient presented with loss of head rotation, which is a definite sign for obtaining spine imaging according to the Canadian c-spine rule.5 Assessment instruments like NEXUS for children or the Canadian c-spine rule for grown-ups and adults facilitate decision making whenever cervical spine injury is suspected and are helpful tools for the physician in charge.
Mechanism of injury
The main motion between atlas and axis is rotation, followed by extension and flexion. The articulation consists of three articulations between C1 and C2: two facet joints and the articulation of the odontoid process with the anterior arch of the atlas body. These are secured by an anterior longitudinal ligament, anterior atlantoaxial membrane, posterior atlantoaxial membrane and longitudinal ligament and the transverse ligament holding the odontoid process against the arch of atlas. Additionally, the odontoid process is directly attached to the occipital bone by two alar ligaments and the apical ligament. The interspinous ligaments reach up to the occiput as another direct connection of C2 to the head. In children up to the age of 6 to 10, the odontoid process of C2 is separated from the vertebral body by a cartilaginous band called subdental synchondrosis. Usually, this synchondrosis does not fully close and partly persist into adult age. Because of the minor resistance of this synchondrosis, shear stress like in hyperflexion movements leads to dislocation of the odontoid process at its cartilaginous connection to the body of the axis. For complete atlantoaxial dislocation all three articulations have to be disrupted: two facet joints and the odontoid process, either by a fracture between body and process or disruption of transverse, alar and apical ligaments.
In the here reported case, MRI and CT scans showed the synchondrotic fracture and tears of the facet joint capsules as well as longitudinal posterior ligament disruption which are required for the complete atlanto-axial dislocation. The head-atlas complex was in a flexion position with an C1-C2 interspinous distance of 2.4cm. These findings in combination with the high-force head-on impact let presume a severe hyperflexion trauma of the cervical spine. Especially young children are predisposed to upper cervical spine injuries facilitated by a high head to body ratio and horizontal facet orientation.3,6 Moreover, the vertebral bodies are wedge shaped, ligaments are elastic, stabilizing muscles are weak and complex sensomotor coordination is slow.4,7 The here additionally observed fracture of the odontoid process represents one of the most common cervical injury in pediatric patients.
Classification
Fractures of the odontoid process are commonly categorized according to the Anderson and D’Alonzo classification.8 Fractures of the tip are type I, at the base type II and through the vertebral body and/or facet joint type III. Due to the anatomic differences in children, four types of odontoid fracture in pediatric patients with open synchondrosis were defined by Hosalkar.9 Type I with three subtypes describes fractures at the level of the subdental synchondrosis. Up to 10% of displacement equals subtype IA, 11% to 100% displacement to IB and IC is defined by more then 100% displacement. Type II comprises all fractures above the level of synchondrosis.10 The diagnosis of odontoid fractures in children can easily be missed, especially in type IA and type II fractures of the Hosalkar classification. Thus a CT scan should be performed if any uncertainty arouses from the plain radiographic imaging, patient’s signs or symptoms, or case history. In any case of detected fracture of the odontoid process, ligamentous disruptions and myelon damage has to be ruled out by MR imaging. Griffiths11 and Fujii12 classify comparable cases as epiphysioloysis or separation of the cartilaginous plate with ventral displacement of the odontoid fragment with atlas and head.13Treatment
There are several techniques to be found in literature for reducing odontoid fractures and atlanto-axial dislocations. In odontoid fractures, Uchiyami uses an assisted but active extension movement without anesthesia for reduction.14 Advantages in this approach are direct feedback on neurologic symptoms and no risk of anaesthesia. Griffith describes reduction by constant traction which needs immobilization.11 We here used the passive reduction under anesthesia in the operating room with fluoroscopy control as previously described by Mandabach.15 As we opted for implantation of dorsal tension wires according to Brook’s procedure, reduction under anesthesia with fluoroscopy control in the same session seemed most appropriate. Odontoid fractures in children can be treated with or without surgery depending on the stability of the fragment. For successful fracture healing, 50% contact of the fragments is reported to be sufficient in children.16 Dislocation of the odontoid fragment into the myelon must be avoided. Thus, in cases of fragment dislocation and/or damaged transverse ligament, a direct screw to the odontoid process stabilizes the odontoid fragment, enabling fracture healing. Non-dislocated fractures in younger children can be treated by minerva cast for 4 to 6weeks.17,18 Also dislocated, reducible odontoid fractures can be managed by 6weeks of cast, not necessarily requiring surgical treatment.19For the surgical treatment of atlanto-axial instability several methods are known: e.g. the Gallie procedure,20 interlaminar clamp, one-piece frame, Magerl procedure21,22 and Brook’s procedure.23 Latter is useful for atlanto-axial instability resulting from different causes such as infection, arthritis, trauma and dysplasia.24 We here used it as a definitive treatment for both, atlanto-axial dislocation and fracture of the odontoid process. When the transverse ligament is intact as in our case, an indirect stabilization and immobilization of the odontoid fracture via atlanto-axial spondylodesis can be used. Thus, tension wiring and bone graft implantation as in the here performed Brook’s procedure is adequate. As described by Moon et al.,24 the Brook’s procedure yields good results when all three, wire fixation, bone grafting and postoperative cervical bracing, are given. When used for atlanto-axial instability management in adults, up to 6weeks of (halo-) cervical bracing with thoracic support are recommended. Alternatives to be found are e.g. 2 to 4weeks of bed rest followed by 8 to 14weeks of cervical brace.25,26 Because of the patient’s young age, we used 3weeks of rigid cervical bracing with a Miami-J-collar followed by another 3weeks of soft collar bracing.
We here describe the case of a 5-year-old boy with atlanto-axial dislocation and fracture of the odontoid process. The Brook’s procedure of wiring C1 and C2 here was a safe and sound surgical treatment. With only six weeks of cervical bracing and three month of tension wiring it was a rather short and comfortable therapy regime for the young patient, yielding a good functional and neurological outcome.
None.
The author declares no conflict of interest.

©2015 Schicho, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.