MOJ
eISSN: 2381-179X


Case Report Volume 4 Issue 2
1Department of General Surgery, Universidad de Quintana Roo, Mexico
2Department of General Surgery, Universidad Nacional Autonoma de, Mexico
3Department of Applied Biotechnique, Universidad Nacional Aut
4Hospital Rural Prospera #1, Universidad Aut
5Hospital General de Zona #1, Universidad Nacional Aut
Correspondence: Luis Angel Medina Andrade, Department of General Surgery, Universidad de Quintana Roo, Mexico Instituto Mexicano del Seguro Social, Hospital General Regional No. 17, Servicio de Cirugía General, Av. Politécnico Manzana 1 Lote 1 Región 509 C.P. 55750, Cancún, Quintana Roo, Mexico, Tel +525-599-81963197, +559-981-114201
Received: March 03, 2016 | Published: March 29, 2016
Citation: Andrade LUM, Collazos SS, Ferretiz MDLAM, et al. Bochdalek hernia with gastric necrosis in a 54-year-old man, case report and review of the literature. MOJ Clin Med Case Rep. 2016;4(2):48-50. DOI: 10.15406/mojcr.2016.04.00084
Background: Bochdalek hernia is a very rare pathology with predominant presentation in newborns, manifested with respiratory distress secondary to pulmonary hypoplasia. The presentation in adults is even rarer, with some reported cases in the context of gastrointestinal complications or incidentally diagnosed, with high morbidity and mortality associated.
Case: A 54-year-old male presented at emergency room with respiratory distress. He had pathological background including Diabetes Mellitus 2 diagnosed 2years ago without control and alcoholism. He was drinking alcohol last two days. He presented feeding intolerance and vomiting last twohours associated with respiratory distress. At physical exam with Glasgow 15, not cooperative for respiratory distress, 110 beat per minute, 30 breaths per minute, without ventilation in left hemi-thorax and SO2 80%. Abdomen without hematomas or other superficial lesions, without acute abdomen signs but a correct evaluation can’t be accomplished by lack of cooperation secondary to respiratory insufficiency. Emergency Department suspected tension pneumothorax and practice a thoracic decompression by puncture obtaining 60cc of blood and intestinal material. An X-ray revealed a gastric bubble in left hemi-thorax. Emergency laparotomy was developed finding a left postero-lateral diaphragmatic hernia with 9cm of diameter, 300cc intestinal liquid and gastric necrosis in 90% with body perforation by previous punction, without reperfusion after reduction. Subtotal gastrectomy and Y-Roux gastro jejunum anastomosis and diaphragmatic hernioplasty without mesh was developed. After 7days in Intensive Care Unit with septic shock patient present pneumonia and died 7days later.
Conclusion: Bochdalek hernia in adults is a very rare pathology that must be corrected immediately after diagnosis by the high rate of associated complications as in the presented case, including advanced procedures like gastro-intestinal resections, with a high morbidity and mortality. When abdominal compromise is suspected an abdominal approach must be preferred to correct the diaphragmatic hernia and the possible lesions associated.
Keywords: bochdalek hernia, diaphragmatic hernia, gastric necrosis, hernia complications
Bochdalek hernia was first described by Vincent Alexander Bochdalek in 1848, described as a posterolateral diaphragmatic hernia.1 The incidence is about 1 in 2200 to 12,500 live births and usually is presented in newborns with respiratory insufficiency due to pulmonary hypoplasia requiring immediately surgery with a high morbidity and mortality.2 It is the commonest congenital diaphragmatic hernia accounting for 78-90% of cases. The presentation in adults is very rare, with an estimated incidence of 0.17%-12.7%. The diagnosis usually is incidental or in the course of abdominal complications for abdominal organs incarceration as in the present case.3
Case
A 54-year-old male presented at emergency room with respiratory insufficiency. His pathological background included Diabetes Mellitus 2 diagnosed 2years ago without medication and chronic alcoholism. He was drinking alcohol for previous 48hours, suspending ingestion 8hours before. He presented one day feeding intolerance and vomiting, adding itself respiratory insufficiency last two hours, reason why he came to hospital. At physical exam with Glasgow 15, dehydrated, not cooperative for respiratory distress, 110 beats per minute, arterial tension 90/50mmHg, 30 breaths per minute, without ventilation in left hemi-thorax and SO2 80% although supplementary oxygen with venture oxygen mask. Abdomen without hematomas or other superficial lesions, without acute abdomen signs but a correct evaluation can’t be accomplished by lack of cooperation. Emergency Department suspected tension pneumothorax after primary evaluation and practice a thoracic decompression with puncture obtaining 60cc of blood and intestinal material. An X-ray revealed a gastric bubble in left hemi-thorax with liquid content and ipsilateral pleural effusion (Figure 1A) (Figure1B). Laboratories revealed White blood cells 18000/mm3, neutrophils 92%, hemoglobin 13.7g/dL, Platelets 82000, Glucose 160mg/dL, Cr 1.4mg/dL. Gas Analysis reported pH 7.1 pO2 52mmHg, pCO2 22mmHg, HCO3 16mmol/L, BE ecf -14.5mmol/L, SO2 82%. Surgical department analyzed the case and suspected a diaphragmatic hernia with gastric incarceration, and perforation secondary to thoracic puncture. CT scan was not developed because septic shock was a contra indication and surgical management has been decided. Emergency laparotomy was developed for gastrointestinal perforation, finding a left postero-lateral diaphragmatic hernia with 9 cm of diameter, 300cc intestinal liquid in thoracic cavity and 90% gastric necrosis with 2mm perforation in the body (Figure 2). After reduction stomach does not presented reperfusion. Subtotal gastrectomy with Y-Roux gastro jejunum anastomosis and diaphragmatic hernioplasty with interrupted polypropylene stitches was developed without intraoperative complications (Figure 3). Patient persisted with septic shock and metabolic acidosis after surgery so their income was decided to intensive care unit. His evolution was torpid and after 7days in intensive care unit a minimal abdominal improvement was noted but unfortunately he developed pneumonia and died 7 days later.
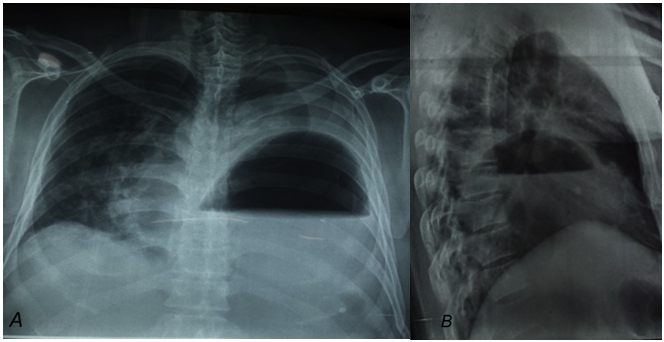
Figure 1A Postero-anterior thorax x-ray presenting gastric bubble occupying left thorax with liquid content and ipsilateral pleural effusion.
1B Lateral thorax x-ray showing stomach in left thorax with liquid content, no more intestinal loops observed.
Diaphragmatic hernia may be congenital, traumatic, or iatrogenic following thoracic and abdominal surgery.3 Bochdalek hernia is a congenital posterolateral diaphragmatic defect described since 1848. Late diagnosis in adult life is estimated in 5% of cases, and since the Alexander Bochdalek description only about 130cases of this pathology in adults have been reported in the literature.4 The general incidence is 1 in 2200 to 12,500 live births, with late diagnosis in 0.17%-12.7%.2 It accounts for 78-90% of diaphragmatic hernias, without sex predominance, but left presentation is more common than right (85% vs 12%).4
It is a developmental defective disorder due to fusion failure of pleuroperitoneal canal that closes usually by the 8th-10th weeks of gestation, with an earlier close of right hemidiaphragm.5 This could explain why right-sided hernias are rarer and other mechanism could be the liver buttressing the right diaphragm.6
Although initially could be asymptomatic in the course of life if lung hypoplasia was not developed, the pressure gradient between pleural and peritoneal spaces ranging from 7 to 20cm H2O, a trauma event, severe strain and obesity can increase abdominal pressure and facilitate herniation of abdominal content through a diaphragmatic defect.7
Diagnosis is usually incidental or in the course of gastrointestinal complications like incarceration with a mortality near 33% in the last. Usually patients course asymptomatic or with chronic symptoms like postprandial fullness or vomiting until adulthood. In an extensive literature review the frequent symptoms presented include chest pain in 69%, obstruction 39%, pulmonary symptoms like dyspnea 37%, strangulated viscera related symptoms 28% and others 20%. Asymptomatic cases account for 14%.4 In the case of incarcerated organs the most frequently displaced include stomach followed by colon, spleen and small bowel.1
Frontal and lateral chest radiographs are the most important tools for diagnosis. Computed tomography have a sensitivity of 71% and specificity of 100% for diagnosis, and accuracy of 88% for left sided injuries or 70% for right sided ones.7
Surgeon must select the better treatment option between laparotomy, thoracotomy, laparoscopic or thoracoscopic approach based on clinical presentation and the experience in each one. Clinical acute presentation usually includes incarcerated visceral components that must be carefully reduced and reviewed to discard perforation or the need for more procedures, reason why a laparotomy approach is preferred. It has been reported that 62% to 90% of Bochdalek hernias do not have hernial sac but is not the rule.8 In cases of an incidental diagnosis surgery must be scheduled as soon as possible,9 for the high risk of future incarceration and mortality associated (33%), with a laparoscopic or thoracoscopic approach confirmed as feasible and safe options.9,10
Diaphragm hernioplasty could be achieved by interrupted stitches with a non-absorbable suture for defect diameter less than 10cm, and in cases of bigger defects the use of biological mesh or a dual mesh (polypropylene and polytetrafluoroethylene) have reported good outcomes preventing fistula formation.8–10
Bochdalek hernia in adults is a rare diagnosis, but must be considered in differential diagnosis of intestinal obstruction or respiratory insufficiency, confirmed by a chest radiograph or other imaging studies like computed tomography if patient condition allow it. Once diagnosis is established, incidentally or in an acute way, surgery must be scheduled by the risk of complications and high mortality associated.
None.
The author declares no conflict of interest.

©2016 Andrade, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.