MOJ
eISSN: 2381-179X


Case Report Volume 4 Issue 6
1Oftalmology department, Asociaci
2General Surgery Department, General Regional Hospital, M
Correspondence: Luis Angel Medina Andrade, General Surgery Department, General Regional Hospital #30, IMSS, México, Tel 9981114201
Received: October 14, 2016 | Published: October 26, 2016
Citation: Grecia OR, Alejandro MAA, Anna HAW, et al. Bilateral optic neuropathy secondary to fragrance ingestion. MOJ Clin Med Case Rep. 2016;4(6):159-161. DOI: 10.15406/mojcr.2016.04.00116
Background: Methanol ingestion by accident or in suicide attempts could produce life threatening conditions, but in survivors the more frequent is optic atrophy, a condition with poor results after correct treatment.
Case: A 46 years-old male come to emergency room secondary to decrease on visual acuity in right eye. He refers that 20 days ago underwent surgery for hip prosthesis fitting without complications and 48 hours after he presented the referred symptoms. He referred to be alcoholic for the past 18 years, with ingestion of fragrances the last 20 days. At physical exam visual acuity was light perception without color discrimination in right eye, and 20/800 in left eye. Intraocular pressure in both eyes were normal. Ocular movements were abnormal, without fixation and XT 30º. Anterior segment present a pupillary defect bilaterally, with mydriasis in right pupil, no reactive to light. In left eye moderate mydriasis and reactivity. Posterior pole of right eye presented an optic disc temporal pallor and optic disc periphery pallor in left eye. Visual fields show a paracentral scotoma in right eye, right superior temporal cuadrantanopsia, left eye with paracentral temporal scotoma (60º). After management with metilprednisolone for eight months’ visual acuity in right eye was finger count at 5 cm, left eye 20/400.
Conclusion: Optic neuropathy secondary to ingestion of methanol as a component of fragrance is very rare, without previous reports in literature at our knowledge. Patient in this case present multiple risk factors to develop optic neuropathy like anemia, malnourish, chronic alcoholism and finally methanol ingestion in a fragrance, contributing to poor outcomes.
Keywords: optic neuropathy, methanol related neuropathy, toxic neuropathy
Methanol is a colorless liquid with similar odor than ethanol, founded usually in the industry as solvent of many daily use products like antifreeze, windshield wiper fluid, some fuels and fragrances.1,2 Methanol intoxication induce metabolic acidosis, sometimes as severe to conduct to death if not treated on time. When patients survive or in chronic ingestion some neurologic diseases as encephalopathy, peripheral neuropathy, and parkinsonism would be present, but the more frequent is optic atrophy in survivors.3 Methanol ingestion have been reported as accidental, in suicide practices or in alcoholic people.2 The present case reports a 46years-old male presenting with bilateral optic atrophy secondary to ingestion of fragrance due to alcoholism. Fragrances usually use ethylic alcohol but in some cases like this, methanol could be a component instead.4
A 46years-old male come to emergency room secondary to decrease on visual acuity in right eye. He refers that 20days ago underwent surgery for hip prosthesis fitting without complications and 48hours after he presented the referred symptoms. He referred to be alcoholic for the past 18years and have hyperuricemia treated with colchicine. At physical exam neurologic, respiratory, cardiovascular and abdominally normal. Visual acuity was light perception without color discrimination in right eye, and 20/800 in left eye. Intraocular pressure in both eyes were normal. Ocular movements were abnormal, without fixation and XT 30º. Anterior segment present a pupillary defect bilaterally, with mydriasis in right pupil, no reactive to light. In left eye moderate mydriasis and reactivity (Figure 1). Posterior pole of right eye presented an optic disc temporal pallor and optic disc periphery pallor in left eye (Figure 2) (Figure 3).
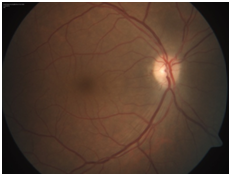
Figure 2 Funduscopy right eye: Papila with deleted edges 360º, discrete temporary yellow - orange coloring and limited peripapilar pigment.
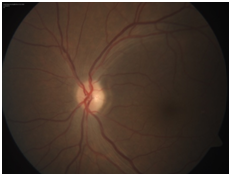
Figure 3 Funduscopy left eye: Deleted borders with temporary dominance, temporal yellow-orange coloring and paton line.
Neuroftalmology service was consulted and during interrogatory patient refers to consume fragrances the last 20days because he had no money to buy ethanol, and for this reason and symptoms of methanol toxicity diagnosis was suspected. At hematic biometry he presented normochromic normocytic anemia (Hb 8.7g/dL), in blood chemistry hyperglycemia with 331mg/dL. Cerebrospinal fluid exam and urinalysis were normal. Exam of methanol in urine was positive with 35mg/L. Simple Cranial Magnetic Resonance and angio-resonance were normal (Figure 4).
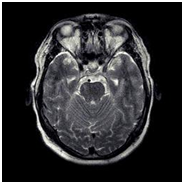
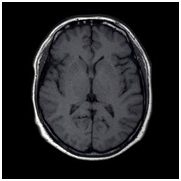
Figure 4 Contrasted Magnetic Resonance. First image T1 (left), second T2 (center) and third (right) without evidence of compression, vascular lesion or ventricular dilation.
Visual fields show a paracentral scotoma in right eye, right superior temporal cuadrantanopsia (30º), left eye with paracentral temporal scotoma (60º). Patient was treated with eight bolus of metilprednisolone of 500mg every 12hours for four days. After that a dose of 75mg of prednisolone every 24hours was administered for the next four months. Finally dose was diminished to 50mg every 24hours for four months. Final visual acuity in right eye was finger count at 5cm, left eye 20/400.
Toxic optic neuropathy include a group of disorders characterized by bilateral visual loss, central scotoma, reduction of color vision and papillomacular bundle damage secondary to substances including drugs, metals, organic solvents, methanol, carbon dioxide and tobacco. Other risk factors identified for presentation of this pathology include nutritional deficit of vitamins (B1, B2, B3, B6, B12), folic acid and proteins with sulphur containing amino acids. If toxins and those deficits are present a synergic effect would be appreciated, and their presentation in developed countries is rare.5 Methanol is a component of multiple industrial solvents and could be found in adulterated alcohol or fragrances as previous mentioned. Methanol is metabolized by alcohol dehydrogenase into formaldehyde, and this metabolized by aldehyde dehydrogenase into formic acid with the subsequent metabolic acidosis and toxicity by formate anion.6
Alcohol and tobacco produces toxic effects with chronic expusure leading to vitamin B12 and folate deficiency, causing accumulation of formic acid and cyanide, metabolites that inhibit the electron transport chain and mitocondrial function, resulting in disruption of ATP production and ultimately impairing the ATP-dependent axonal transport with focal retrolaminar optic nerve delamination and retrobulbar demyelination.7,8 The effect of methanol in optic nerve is complex and could be difficult to diagnose without appropriate background. In optic fundus, ophthalmoscopic and angiographically, the only lesion founded is optic disc edema by axoplasmic flow stasis, for the inhibition of oxidative metabolism, secondary to swelling of the cytoplasm of the astrocytes and oligo-dendroglia in the retrolaminar space and for compressive obstruction of orthograde axoplasmic flow. This swelling is secondary to metabolic acidosis and cytochrome C oxidase formic acid inhibition, resulting in histotoxic hypoxia and histopathologic changes in outer retina like enlarged retinal subspaces, areas of cone degenerations seen on light microscope, focal retinal pigment epithelium (RPE) detachment and degeneration or vacoulation of RPE cells with loss of apical microvilli seen on electron microscopy. Necrosis on basal ganglia and retrolaminar portion of the optic nerve could be found, in part due to alteration in blood flow.9
Symptoms include painless loss of visual acuity (acute or chronic), in the acute presentation could be refered until up to 24-48hours after ingestion, blur at the point of fixation (central scotoma), reduced contrast perception, a blur in the centre when reading (continuously and slowly progressing), faded colours (particularly red) or a general loss of colour perception. Light perception could be minimally reduced in rare cases. Visual fields test reveals symmetrically central or paracentral scotoma, initially with preservation of the peripheral field.5 Clinical signs of toxic neuropathy usually include sluggish pupils without a relative afferent pupillary defect and decreased color vision. Optic disc can be swollen, hyperemic in early stages or initially normal, with temporal pallor seen in late stages. The selective papillomacular bundle involvement leads to the previous mentioned central and cecocentral scotomas.10 Imaging studies include MRI of the optic nerves to exclude a compressive lesion and use to be normal in methanol induced optic neuropathy, sometimes basal ganglia degeneration could be found.5
Treatment is to discontinue the toxic agent initially. An inhibitor of alcohol dehydrogenase called Fomepizole is very useful to treat methanol toxicity, resulting in complete restoration of vision and resolution of metabolic acidosis, but not available in all medical centers.1–6
Steroids are the preferred and more used treatment because it is believed that may inhibit demyelination but this and the combination with ethanol and B-group vitamins have limited success, sometimes with final visual acuity in counting fingers. In some series the use of steroids, vitamin B12, and folic acid resulted in visual improvement. Erythropoietin have been proposed to suppress neuronal apoptosis and decrease the inflammatory response, with beneficial effects on retinal ganglion cells, including reduction in apoptosis and increased survival after optic nerve transaction.9 Sergey Zakharov11 reported that pre-hospital administration of ethanol reduces 90% the probability to present abnormal findings in retinal nerve fiber layers (p=0.01), but however long-term symptoms after this and correct treatment persist in 10-30% of patients.12
Optic neuropathy secondary to ingestion of methanol as a component of fragrance is very rare, without previous reports in literature at our knowledge. Patient in this case presents multiple risk factors to develop optic neuropathy like anemia, malnourish, chronic alcoholism and finally methanol ingestion in a fragrance. All this factors contribute to clinical presentation and poor visual recovery after treatment with steroids. Ethanol admnistration was not feasible as patients come too many days after ingestion. Although that, other measures like administration of vitamins and erythropoietin could help to achieve better results as mentioned in some series and the treatment would be stablished as soon as possible once the suspected diagnosis is confirmed with the mentioned characteristics.
None.
The author declares no conflict of interest.

©2016 Grecia, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.