MOJ
eISSN: 2381-179X


Case Report Volume 6 Issue 3
Vardhman Mahavir Medical College and Safdarjang Hospital, India
Correspondence: Arora J, Vardhman Mahavir Medical college and Safdarjang Hospital, India
Received: January 27, 2017 | Published: March 17, 2017
Citation: Arora J, Kohli M, Goel S, et al. Anomalous suprascapular foramen in adult Indian scapula. MOJ Clin Med Case Rep . 2017;6(3):62-64. DOI: 10.15406/mojcr.2017.06.00160
The present study was conducted to highlight the variations of suprascapular foramen in an extensive osteological study of 100dry scapulae. Attempt was also made to establish a comparison between osteological and radiological appearance of such variations. In only one scapula, an ossified superior transverse scapular ligament was discovered which converted the suprascapular notch into a suprascapular foramen. The ossified superior transverse scapular ligament presented as an oblique bony ridge, fan shaped in appearance. Conversion of suprascapular notch into a foramen is considered as a potential risk factor for the suprascapular nerve entrapment syndrome. The present day neurosurgeons, radiologists and orthopedic surgeons should be aware of such bony abnormalities, as these are imperative in preoperative radiological assessment and intraoperative modification of surgical procedures during arthroscopic decompression of suprascapular nerve.
Keywords: scapula, suprascapular foramen, suprascapular nerve, anatomical variations, entrapment
Anatomical variations of suprascapular region are of immense importance for arthroscopic suprascapular nerve decompression. Existence of a narrow suprascapular notch is a well-known cause of suprascapular nerve entrapment. Knowledge of anatomical variations of suprascapular notch is of extreme relevance because of occurrence of suprascapular nerve entrapment syndrome. Studies report the entrapment of suprascapular nerve at the site of suprascapular notch.1 The present study reports a rare occurrence of abnormal position of suprascapular foramen and ossified superior transverse scapular ligament (STSL) in osteological specimen of an adult Indian scapula.
Injury of suprascapular nerve is often reported due to direct trauma, anterior shoulder dislocation, presence of ganglion cysts and sarcomas.2,3 Hence, accurate anatomical knowledge of variations of suprascapular notch is of immense value to the present day clinicians.
In an osteological study of 100 intact dry Indian scapulae, an abnormal suprascapular foramen (SSF) was discovered at the base of coracoid process (Figure 1-4). Morphological features of the SSF were studied and appropriate photographs taken.
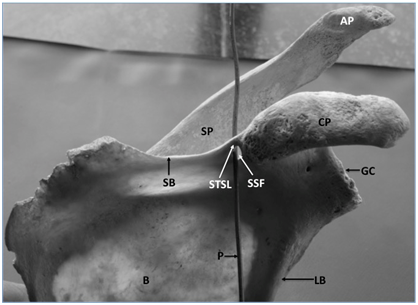
Figure 1 Anterior view of bony scapula showing.
SSF, suprascapular foramen; STSL, superior transverse scapular ligament; P, probe in SSF; CP, coracoid process; AP, acromian process; SP, spinous process; GC, glenoid cavity; B, body of scapula; LB, lateral border of scapula; SB, superior border of scapula.
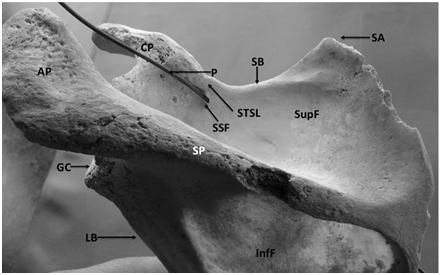
Figure 2 Posterior view of bony scapula showing.
SSF, suprascapular foramen; STSL, superior transverse scapular ligament; P, probe in SSF; CP, coracoid process; AP, acromian process; SP, spinous process; GC, glenoid cavity; SupF, supraspinous fossa; InfF, infraspinous fossa; LB, lateral border of scapula; SB, superior border of scapula; SA, superior angle of scapula
SSF, suprascapular foramen; STSL, superior transverse scapular ligament; P, probe in SSF; CP, coracoid process; AP, acromian process; SP, spinous process; GC, glenoid cavity; B, body of scapula; LB, lateral border of scapula; SB, superior border of scapula.
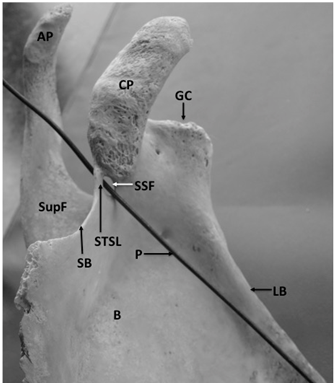
Figure 3 Anterior surface of bony scapula showing.
SSF, suprascapular foramen; STSL, superior transverse scapular ligament; P, probe in SSF; CP, coracoid process; AP, acromian process; GC, glenoid cavity; SupF, supraspinous fossa; LB, lateral border of scapula; SB, superior border of scapula; B, body of scapula
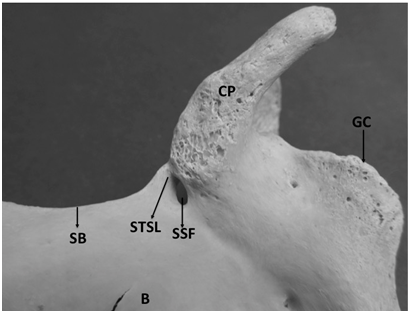
Figure 4 Anterior surface of bony scapula showing.
SSF, suprascapular foramen; STSL, superior transverse scapular ligament; P, probe in SSF; CP, coracoid process; AP, acromian process; GC, glenoid cavity; SupF, supraspinous fossa; LB, lateral border of scapula; SB, superior border of scapula; B, body of scapula
The circumference of the bony foramen was 17mm. Its superior margin was made of ossified STSL. The body of scapula constituted the inferior and medial margin. Root of coracoid process formed the lateral margin of the foramen. The maximum vertical diameter of the foramen was 7mm and the maximum transverse diameter was 4mm. The SSF was oval in shape. It was not present at the usual site but instead presented at the root of coracoid process. The margins of SSF were smooth and the foramen formed a communication between supraspinous and subscapular fossa. This was confirmed by passing a probe through the foramen. The ossified STSL, forming the superior margin of the SSF was oblique and fan shaped. It converted the suprascapular notch into a foramen. The width of STSL at the root of coracoid process was 3mm and its width at the lateral most end of superior border of scapula was 5mm. The patency of SSF was established by taking a radiological picture after putting a probe through the foramen (Figure 5) (Figure 6).
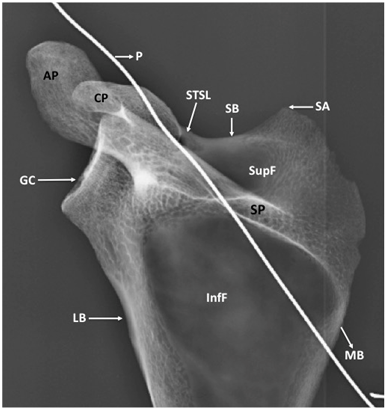
Figure 5 X-Ray of Scapula (AP view) showing. STSL, superior transverse scapular ligament; P, probe in suprascapular foramen; CP, coracoid process; AP, acromian process; SP, spinous process; GC, glenoid cavity; SupF, supraspinous fossa; InfF, infraspinous fossa; LB, lateral border of scapula; SB, superior border of scapula; MB, medial border of scapula; SA, superior angle of scapula.
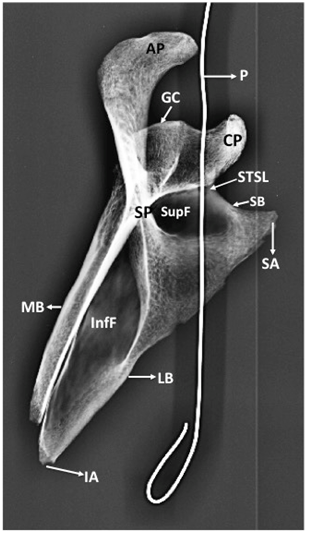
Figure 6 X-Ray of scapula (Oblique view) showing.
STSL, superior transverse scapular ligament; P, probe in suprascapular foramen; CP, coracoid process; AP, acromian process; SP, spinous process; GC, glenoid cavity; SupF, supraspinous fossa; InfF, infraspinous fossa; LB, lateral border of scapula; SB, superior border of scapula; MB, medial border of scapula; SA, superior angle of scapula
The anatomical variations of suprascapular notch have been implicated in suprascapular nerve entrapment.4 Several morphological variations and classification of the suprascapular notch have been reported in western population. Studies report double suprascapular foramen, one above the other.4,5 Ossification of bifid superior transverse scapular ligament (STSL) have been indicated in these studies. The suprascapular notch is situated in the lateral part of the superior border of the scapula just adjacent to the base of coracoid process. The STSL connects the superior margin of scapula medially with the coracoid process laterally and forms part of an osseo fibrous foramen through which the suprascapular nerve courses. The STSL converts the suprascapular notch into a foramen separating the suprascapular artery and nerve. Studies have reported changes of STSL in response to mechanical load, reflected in the composition of extracellular matrix. Fibro cartilaginous character of enthesis has been reported which suggests that the insertion sites of STSL are subject to both compressive and tensile loading and are regions of stress concentration.6 Several classifications of suprascapular nerve have also been described in literature.7–9 Studies have implicated the course of suprascapular nerve through a grove which makes it liable for entrapment.4
Our study reports an anomalous suprascapular foramen at the root of coracoid process. It is our humble assumption that the formation of this suprascapular foramen could have resulted as a sequel to ossification of superior transverse scapular ligament. Such an abnormal foramen which simulates a bony canal may decrease the area of suprascapular notch and lead to entrapment of suprascapular nerve. Knowledge of such abnormal suprascapular foramen is essential for preventing neurovascular injury during surgical procedures. Interventional procedures of suprascapular nerve and management of entrapment neuropathy requires accurate knowledge and awareness of such abnormal foramina. Studies report that the suprascapular notch is frequently bridged by bone rather than a ligament, converting it into foramen in some animals, but incidence is not so common in humans.10 The presence of suprascapular foramen clearly indicates the presence of ossified superior transverse scapular ligament. One of the most important risk factors for suprascapular nerve entrapment is a completely ossified STSL.8,11 Studies report evidence of neural degeneration in nerve specimens of STSL ossification.12
Studies report a wide variability of ossified STSL. Rare in Alaskan Eskimos, 0.3% and more frequent in Brazilians, 30.76%. Occurrence of such diversity in incidence of ossified STSL has been attributed to genetic basis.13 On the basis of newest description of STSL variations, the bony bridge of STSL has been classified as either fan shaped or band shaped. It is reported that band shaped type was more often ossified than fan shaped type.14 The mean surface area of the foramen formed in this way was greater in the fan shaped than in the band shaped type (50.75mm2 and 30.43mm2 respectively). The ossified STSL reported in the present study is fan shaped. This fact was established after measurement and comparison of the width of ossified STSL at its two ends. The ossified fan shaped STSL may be a potential risk factor in suprascapular nerve entrapment because the space below the bony bridge is significantly reduced.
Etiopathogenesis of suprascapular nerve entrapment depends on several factors. These may be presence of a bifid STSL15,16 trifid STSL,16 narrow V-shaped suprascapular notch7or presence of anomalous double suprascapular foramen.5 The present study reports an anomalous suprascapular foramen at the root of coracoid process, interestingly, not in the normal site of suprascapular notch. It is the evident conversion of an abnormally located suprascapular notch into a foramen by an ossified STSL. As anatomists we opine that presence of such an anomalous abnormally located suprascapular foramen may precipitate abnormal diverted routes taken by suprascapular artery or nerve and affect scapular anastomosis.
Anatomical knowledge of variations of suprascapular foramen may assist the clinicians to define the presence of suprascapular foramen and correlate it to suprascapular nerve entrapment. Studies reporting the type of suprascapular notch are many.17,18 However reports of abnormal suprascapular foramen are few. Presence of such rare anomalous suprascapular foramen with ossified STSL may lead to an unfortunate sequel of compression of suprascapular nerve. Knowledge of such anatomical variations of suprascapular foramen is essential in surgical procedures that involve decompression of the nerve at suprascapular notch to restore shoulder function.
It is our humble assumption that knowledge of such anatomical variations as reported in the present case may be of great help during arthroscopic decompression of entrapped suprascapular nerve. Cadaveric studies show evidence that the suprascapular nerve may pass either above or beneath an accessory band of the STSL. The nerve may also give branches in advance. One branch may be located above and the other below this band.8,18 Studies report a ‘sling effect’ to describe the mechanism of injury against the sharp inferior border of STSL due to inadequate size of suprascapular notch.7
The present study is of utmost relevance for radiologists, neurosurgeons and orthopedic surgeons. Identification of suprascapular foramen during preoperative radiological examination or intraoperatively is imperative as its presence may modify the surgical approach during open or arthroscopic decompression of suprascapular nerve.
None.
The author declares no conflict of interest.

©2017 Arora, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.