MOJ
eISSN: 2381-179X


Case Report Volume 8 Issue 1
ENT, King Fahad Specialist Hospital, Saudi Arabia
Correspondence: Ali Al Momen Affiliation, Consultant, ENT, Rhinology and skull base surgery, King Fahad Specialist Hospital, Dammam, Saudi Arabia, Tel 966505843702
Received: January 29, 2018 | Published: February 6, 2018
Citation: Eid MA, Nassir BA, Momen AA. Aggressive fibromatosis of the neck: a case report and review of the literature. MOJ Clin Med Case Rep. 2018;8(1):22-24. DOI: 10.15406/mojcr.2018.08.00232
We present our experience with a very large painless slowly growing neck mass extending from mid neck to the clavicle displacing the trachea to the other side. FNA and incisional biopsy did not confirm the diagnosis. A complete excision of the lesion with the invaded internal jugular vein confirms the diagnosis of Aggressive Fibromatosis. Different modalities of the treatment will be discussed.
Keywords: aggressive fibromatosis, desmoid tumor, neck mass
Aggressive Fibromatosis, also called desmoid tumor, is a rare benign with local aggressive behaviour that originate from musculoaponeurotic structures. Reported most common cases between the ages 20-40yrs with female predominance 2:1. The rate of recurrence after surgical resection ranges from 36 to 77%.1 We report the case of a 24 years old female patient with aggressive fibromatosis with invading of internal jugular veins that confirm our diagnosis.
A 24years old female patient, presented with a history of painless left sided neck mass, which has been gradually increasing in size (Have been reported to another hospital 6months prior to presentation). She also gave a history of mild odynophagia and difficulty in neck movement. There was no history of dysphagia, change of voice, or dyspnea. Her weight and vitals were normal.
On physical exam, the mass was large, firm, non-tender and non- pulsating. Filling the left aspect of the neck extending from the mid neck to the clavicle and from the posterior triangle to the midline displacing the trachea to the right side. The mass was fixed to the underlying structures but the covering skin was freely mobile. There was no palpable cervical lymphadenopathy.
On radiological evaluation, computerized tomography scan of neck showed a large mass evolving the left prevertebral muscle from the mid neck to the thoracic inlet causing a displacement of the carotid and the jugular vein in anterior direction (Figure 1).
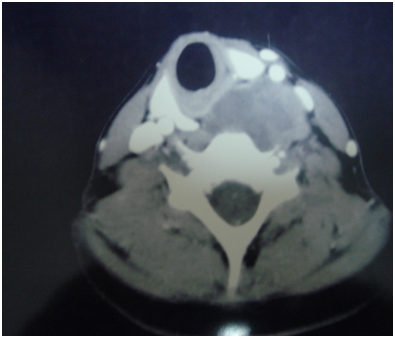
Figure 1 CT scan of neck, axial view, showing a large mass involving the left prevertebral muscle from the mid neck to the thoracic inlet displacing the carotid and the jugular vein anteriorly.
The patient was taken up for further investigation; FNA biopsy was obtained followed by incisional biopsy. The histopathological evaluation of biopsies showed Spindle cells, fibrohystiocytic lesion, favour benign without evidence of malignancy. There was no definite diagnosis yet.
On the basis of radiological and histopathological findings with no definitive diagnosis, a wide surgical excision of the lesion was performed under general anaesthesia (Figure 2). The lesion aggressively invaded the internal jugular vein, which has been resected with the lesion. Final pathological evaluation revealed 10x6x5cm mass with local infiltration to prevertebral muscle (Figure 3). No postoperative complications were experienced.
Unfortunately, after 6months follow up recurrence occur, complete surgical excision done. Local radiotherapy treatment was considered but the patient refused. The patient remains free of the disease for over 2years with closing follow up.
Aggressive fibromatosis is a proliferation of fibrous tissue that arise from fascia, periosteum and musculo aponeurotic structures, it is derived from mesenchymal cells. And characterized by a tendency to infiltrate surrounding tissues and to recur locally after surgical excision.2,3
The nomenclature to describe fibromatosis in the literature can be confusing. Synonyms; Desmoid tumor, Desmoid fibromatosis, Grade I fibromatosis (desmoid type) and Desmoplastic fibroma.
Most cases are sporadic, but can occur in association with familial adenomatosis polyposis, osteomas of the skull bones as a part of Gardner Syndrome.4–6 There has been an observed incidence of trauma of about 19–49% preceding the development of cases of aggressive fibromatosis. The pathogenesis is thought to involve abnormal response of healing with persistent immature fibroblast formation which later gives rise to the tumor. Steroid sex hormones are also believed to play a role in pathogenesis.7 Fibromatosis can occur at any age but is most common between the ages 20-40yrs.8 Most series report a female predominance 2:1. The rate of recurrence after surgical resection ranges from 36 to 77%.1 Most recurrences occur within 2years.
Approximately 9-27% of Aggressive Fibromatosis are located in the head and neck region. Fibromatosis usually present as painless masses, however, pain is not an unusual symptom. In the head and neck area, functional deficits, including trismus, speech impairment, dysphagia, nasal obstruction and difficulty in closing the eye, have been reported.1
A representative tissue biopsy is required for diagnosis.9 Histological spindle shaped uniform cells surrounded by abundant collagen, the degree of cellularity is moderate but can vary from area to area within the tumor. Nuclei are never at typical or hyperchromatic and mitosis can occur but are never abnormal (Figure 4).
The differential diagnosis for pathologists includes: Fibrosarcoma, Reactive fibrosis, Nodular fasciitis, hypertrophic scars and keloids.10 MRI is the investigation of choice to assess the extension of the disease and for follow up, because of superior soft tissue representation in comparison with CT.11,12 No clinical trials have been performed to clarify the best approach to treating fibromatosis. Most authors recommend surgical excision as the initial approach, with radiotherapy and chemotherapy used adjunctively.
The aim of surgery is complete excision with tumor-negative margins. Because fibromatosis tend to infiltrate surrounding tissues, microscopically complete excision is often not possible. This is especially true in the head and neck region and particularly the skull base, where the density of vascular and neural structures often prevents complete excision. Head and neck fibromatosis demonstrate a recurrence rate of 40-70% after resection. The majority of which occur within 18months of excision.13
The age of the patient and tumor site are the known factors associated with recurrence.14 The role of the microscopic status of tumor margins is more complex. Some large retrospective studies showed high local recurrence rate with microscopically positive margins,15,16 other studies failed to demonstrate an effect of microscopic margins on recurrence.17,18
Several series have reported that radiotherapy can improve the local control of the tumor. In the series of studied by Plukker et al.19 1998, patients with incomplete resection or recurrent disease were treated with at least 50Gy of wide field radiotherapy.19
Chemotherapy has also been used successfully to fibromatosis, primarily in the pediatric population. Goeprfert et al. 1998 reported the treatment of six children with desmoid fibromatosis of the head and neck with one or two chemotherapeutic regimens. Because tumor cell expression of estrogen receptors has been demonstrated in Aggressive fibromatosis, hormonal therapy with Tamoxifen has been attempted.20 Transformation of Aggressive fibromatosis to malignant sarcomas is exceedingly rare. Only a few cases of transformation have been reported in the literature. Death is uncommon but may occur as a result of compression of vital structures, such as the trachea and major blood vessels of the neck.
Patient consent related case report take the permission from concerned patient.
None.
The author declares no conflict of interest.

©2018 Eid, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.