MOJ
eISSN: 2381-179X


Case Report Volume 4 Issue 1
Department of Orthopaedic Trauma, Ulm University, Germany
Correspondence: Schicho A, Department for Orthopaedic Trauma, Ulm University, Germany, Tel +49 (0)731 500-54571, Fax +49 (0)731 500-54502
Received: October 29, 2015 | Published: January 29, 2016
Citation: Schicho A, Riepl C, Scola A. A typical case of paradox cerebral embolism during cemented total hip arthroplasty. MOJ Clin Med Case Rep. 2016;4(1):11-12. DOI: 10.15406/mojcr.2016.04.00076
It is known that implantation of hip endoprosthesis, especially when cemented, is accompanied by the risk of fat embolism to the pulmonary circulation. We here report the case of a paradox embolism in a patient with a persistent foramen ovale in the heart.
A 77-year old man with a known multiple myeloma fell on his hip and suffered a femoral neck trochanteric fracture (AO 31.B3). A cemented total hip arthroplasty was performed and the greater trochanter was stabilised by cerclage. After surgery, slurred speech and a deviation of the eyes were observed. Magnetic resonance imaging (MRI) of the brain showed ischemia in the dorsal flow area of the cerebellum on both sides, especially in the pica flow area, the left thalamus, left temporal and occipital due to multiple embolisms. Trans esophageal echo-cardiography showed a persistent foramen ovale (pfo) with free flow. Intensive specialized physio and ergotherapy was initiated with good results. Upon control three and a half years later the patient showed no neurologic sequelae and a stable hip prosthesis.
Keywords: hip endoprosthetics, paradox embolism, cerebellar ischemia, persistent foramen ovale
In the past decades, hip endoprosthetics became one of the most successful standard procedures in orthopaedic and trauma surgery. Improvement of surgical techniques and implants yield better results and less morbidity, each year more than 200.000 hip endoprosthesis are implanted in Germany.1
Nevertheless, the cardio-pulmonal system is put at risk especially in cemented prostheseis by fat embolism.2 In most cases the embolism is clinically in apparent or leads to mild fluctuations of the blood pressure. A more severe complication based on a patho-mechanism believed to be rare was seen in the following case.
A 77-year old man with a known multiple myelomas fell on his hip and suffered a femoral neck trochanteric fracture (Figure 1). He was administered to our hospital. Due to the type of the fracture (AO 31.B3) as well as a metastasis in the neck and acetabulum a cemented total hip arthroplasty was performed. The greater trochanter was stabilised by cerclage (Figure 1).
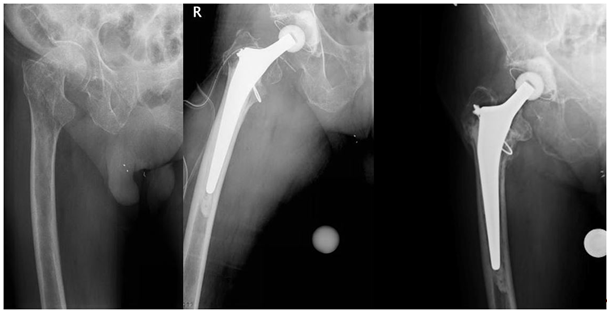
Figure 1 Femoral neck trochanteric fracture (AO 31.B3), control after cemented total hip arthroplasty, and follow-up 3.5 years after surgery.
The procedure was performed under general anaesthesia. Both cup and stem were cemented. While implanting the cemented stem the heart beat raised from 60bpm to 95bpm and the blood pressure dropped to 90/45mmHg (Figure 2). To the end of the procedure the patient had recovered and was extubated showing stable vitals.
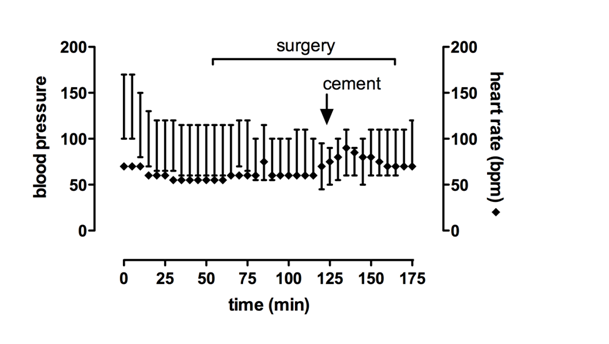
Figure 2 Blood pressure and heart rate during surgery. Changes of blood pressure and heart rate precede cement implantation, possibly indicating fat embolism through reaming.
After surgery a slurred speech and a deviation of the eyes were observed. The MRI (1,5 T, T1w SE sagittal, FLAIR coronar, T2w TSE transversal, bleeding- and diffusions sensitive sequences T2w TSE sagittal TOF angiography and secondary multiplanar reconstructions) showed multiple ischemic regions in the dorsal flow area of the cerebellum on both sides, especially in the pica flow area, the left thalamus, left temporal and occipital due to multiple embolisms (Figure 3). Space occupying cerebral edema was not found.
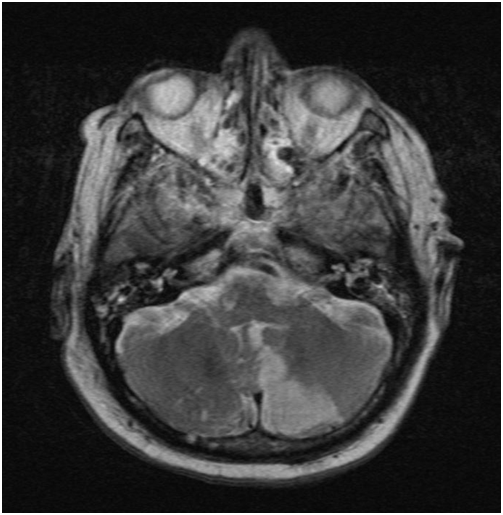
Figure 3 Cerebral magnetic resonance imaging. The diffusion sensitive sequences (T2w TSE) show a left sided ischemia of the cerebellum following surgery.
Transthoracic echo-cardiography was performed without pathology. Transesophageal echo-cardiography showed a persistent foramen ovale (pfo) with free flow even without Valsalva maneuver. No intracardial thrombi or a major sclerosis of the aorta could be found. Duplex sonography ruled out deep vein thrombosis or pathological flow in the carotids. CT-scans of thorax and cranial MR-angiography excluded pulmonary embolism as well as cerebrovascular diseases, especially of the basilar artery.
A follow-up CT-scan of the brain was performed 6days after surgery. The ischemia right parietal, in the left thalamus and in the left cerebellum marked clearly. At this time the patient was stable on ward and his neurologic deficits reduced significantly under intensive ergo- and physiotherapy. After two years, the patient returned to our outpatient department after a fall; the hip was stable and no residual neurologic deficits were observed. Upon control three and a half years after the embolism the patient showed no signs of neurologic sequelae and no loosening of the implant (Figure 1).
The first description of a paradox embolism was by Cohnheim in 1877. Pathophysiological a right to left shunt is mandatory for the transition of veinous embolic material into the arterial circulation.3 The most common path therefore is a persistent foramen ovale (pfo). In an anatomic study of 1100 hearts the incidence of a pfo was 35%.4 Usually the foramen ovale closes after birth due to changes of the pressure conditions in the pulmonary circulation. Despite the high incidence of pfo the rate of paradox embolism as a cause of cerebral ischemia is rare.5
Pulmonary or intracranial embolism as a complication following and endoprosthetic procedure are figured 0.5-2% in current literature.6 Most cases of paradox embolism are based on deep vein thrombosis or formation of a venous thrombus at another location6. With intra operative trans esophageal echo-cardiography while reaming the femoral bone for implantation of an intra medullary nail as well as while inserting the stem of an hip arthroplasty, embolic events actually were shown in the majority of the cases.7,8
In bone cement associated complications especially pulmonary embolism is not a rare event. While most embolic events following hip arthroplasty are clinically inapparent, paradox embolisms are very rare but serious and possibly life threatening.3,9 A study comparing cemented versus non cemented stems in hip arthroplasty showed a significant higher rate of fat embolism in cemented stems.2 This has to be taken into account when opting for arthroplasty and choosing a prosthesis model. In our case, changes in heart rate and blood pressure preceded cement implantation; this may indicate fat embolism through femoral stem reaming, or inserting the (cemented) stem.
In conclusion paradox embolism is a rare but severe complication of hip arthroplasty. It is caused by insertion of the (cemented) stem or reaming of femur and tibia and is a possible complication whenever manipulating bones marrow. In patients with a known pfo a thorough discussion of therapeutic options is mandatory.4
None.
The author declares no conflict of interest.

©2016 Schicho, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.