MOJ
eISSN: 2381-179X


Case Report Volume 11 Issue 1
Department of Neurology, Clinical Hospital Centre Zagreb, Croatia
Correspondence: Katarina Blazina, Department of Neurology, Clinical Hospital Centre Zagreb, Croatia, Tel 00385 99 2491 104
Received: January 24, 2021 | Published: February 11, 2021
Citation: Blazina K. A case of a young patient diagnosed with the Hippel-Lindau disease c.571 C>G mutation (Croatian form) and multiple paragangliomas after developing ischemic stroke. MOJ Clin Med Case Rep. 2021;11(1):18-19. DOI: 10.15406/mojcr.2021.11.00373
Correlation between erythrocytosis and ischemic stroke is very common and not at least unusual. I present the case of a young patient who was first diagnosed with secondary erythrocytosis and after he developed an ischemic stroke more detailed diagnosis was made. He was then diagnosed with VHL c.571 C>G mutation (Croatian type). This case shows us the importance of scrutinizing cases, especially in very young patients.
Keywords: secondary erythrocytosis, hippel-lindau disease, c.571 C>G mutation, multiple paraganglioma, stroke
Erythrocytosis is one of the major risk factors for the ischemic cerebrovascular disease.1 In cases of the young-onset disease, we always have to keep in mind possible genetic mutations ( and it's subtypes) that have been identified over the last several years: VHL, RET, SDHB, SDHD.2 The Hippel-Lindau disease ( VHL) is usually associated with multiple endocrine neoplasms, neurofibromatosis type 1, medullary neoplasms ( MEN 2) and familiar paraganglioma, thyroid carcinoma, neuroblastoma or pheochromocytoma.2 The VHL gene product encodes VHL protein which is responsible for hypoxia-inducible factor 1 that leads to hypoxia dependent vascular tumor growth. The novel found VHL mutation in exon 2 is associated with polycythemia but not with cancer.3
A 31-years old caucasian man came to the neurology emergency department because of the sudden onset of right-sided palsy with sluttered speech. He reported no headache, dizziness or convulsions. After the initial workup, he was admitted to the neurology department. MRI showed subacute ischemic stroke in the posterior part od left insula and operculum. 3D- TOF MR angiography showed occlusion of one of the smaller branches in M2/M3 segment. We performed a doppler ultrasound of carotid and vertebral arteries that indicated vascularized parenchymal structure between ACI and ACE on the right side (Figure 1). Because of that, we did MRI of the neck that verified the inhomogenic structure at the bifurcation of carotid arteries od the right side, dimensions 2,6X1,8X1,9cm that resembles paraganglioma (Figure 2).

Figure 1 Ultrasound of the neck- tansversal plane. Arrows are marking internal carotid artery, external carotid artery and paraganglioma.
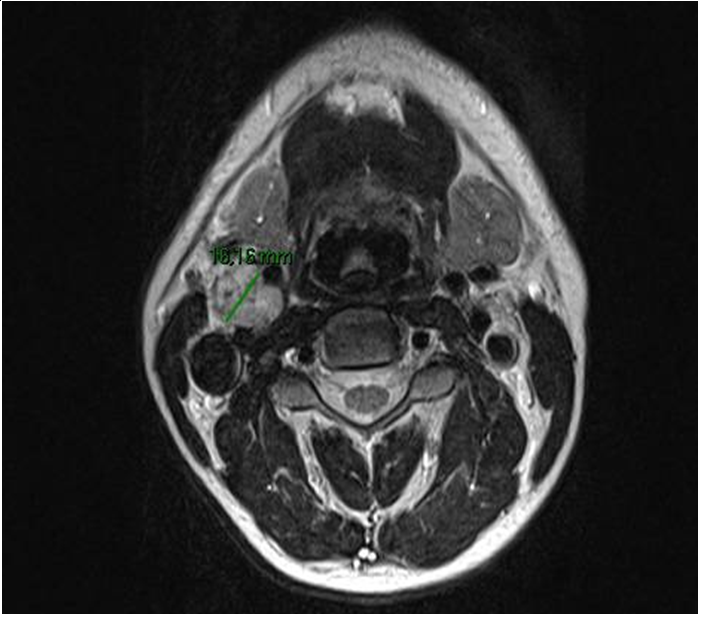
Figure 2 MRI of the patients neck showing large paraganglioma between internal and external carotid arteries.
In the patient's medical history we found erythrocytosis but premorbid history is not well known because he was treated abroad and diagnosed with secondary erythrocytosis due to increased affinity of hemoglobin to oxygen.
Haematologist was consulted and erythrocytapheresis was performed. He was dismissed from hospital without neurological deficit with recommended antiaggregant therapy with ASK 100mg/day. After dismission he continued with haematologic workup: PET /CT was performed that showed pathological metabolism of F-18 dopa on his neck on both sides and in the abdomen at the aorta bifurcation. Additional diagnostic workup didn̒t find abnormal hormonal activity (cortisol 458nmol/L, chromogranin A 84,0ug/L, eritropoerin 154mlU/L, 5-hydroxyindolacetic acid 20nmol/dU, metanephrine1.2umol/dU, normetanephrine 1.7 umol/dU, vanillylmandelic acid 12umol/dU, hemoglobin variant analysis 22umol/dU. Other laboratory findings were: E 9,66x10 (12), Hb146g/L, Htc 0,573L/L, MCV 57,9fL, MCH 15,1g/L, Tr 246x10 (9), RTC26/1000, JAK 2V617F was negative.
After that, the suspicion of von Hippel-Lindau syndrome was established. He continued with neck imaging follow-up without progression.
Molecular – genetic testing and sequencing confirmed homozygotic mutation for VHL c.571 C>G (Croatian form of mutation).4
In the meantime, he continued with erythrocytapheresis and went to hematologist abroad for a consultation about paraganglioma on the neck. At the beginning of 2019, the extirpation of paraganglioma of the right side of his neck was performed and for now, he is in regular hematological controls.
Erythrocytosis (and other polycythemia disorders) are well-known risk factors for developing ischemic stroke (not just cerebral). And because of that majority of patients underwent venepunctions (depend on laboratory results) and they all use antiaggregants in their therapy. But sometimes we have to investigate more thural especially when we have very young patients and from geographic area known for specific genetic mutations5 and genetic mutations in general because of their risk not only for erythrocytosis and it̒s consequences but because increased risk of developing tumors,1 when time is on essence in treating these patients.
After accidentally found paraganglioma on carotid ultrasound we extended our workup and after many years established concrete diagnose.
Mutation phenotype is necessary for establishing disease risk because some paragangliomas may be malignant.2 In the majority of cases paraganglioma of the neck are usually benign, non-hormonal secreting tumours, traditionally treated by excision.6
Our report emphasizes the importance of genetic testing in young patients with erythrocytosis/polycytosis and not just simply qualify condition as secondary because early diagnosis can prevent unwanted complications and detect eventual tumors on time.
Written informed consent was obtained from the patient for publication of this case report.
The author declares that there is no conflict of interest.
None.
None.

©2021 Blazina. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.