MOJ
eISSN: 2381-179X


Case Report Volume 9 Issue 2
1Department of Anesthesia, Consultant Anesthetist, SMBB Trauma Centre, Pakistan
2Professor, Department of Anesthesia, SMBB Trauma Centre, Saudi Arabia
Correspondence: Mussarat Afzal MD, Consultant Prince Mohammed bin Abdulaziz Hospital, KSA-Riyadh, Saudi Arabia
Received: April 17, 2019 | Published: April 22, 2019
Citation: Naz A, Aftab S, Afzal M. A case of open degloving injury in a pregnant patient. MOJ Clin Med Case Rep. 2019;9(2):44-46. DOI: 10.15406/mojcr.2019.09.00300
Degloving injuries of lower limb are very common but abdominal wall degloving injuries are seldom reported .here we report a case of young female 24week pregnant with extensive lower limb and abdominal wall degloving skin.
Keywords: soft tissue, degloving injury, VAC dressing, split thickness, skin graft
Road traffic accidents are taking lives of approximately 1.25million people in the world annually. Trauma during pregnancy is also quite common in developing countries but it is not frequently reported. Mothers in 3rd trimester are most vulnerable for trauma due to unstable gate and shift of center of gravity.1,2 Degloving injuries are one of very common devastating injury associated with road traffic accident. It is a type of avulsion in which rotational force causes skin and subcutaneous tissue to be torn completely from underlying muscle and fascia3 .It can be open or closed .It is most common in males and main sites are lower limb, trunk, scalp and face. Diagnosing degloving injury is also a challenging decision .most of the time it’s clinical or by ultrasound or CT scanning.3,4–9
Extensive degloving injuries can be associated with other trauma like fractures, head injuries or visceral injuries, which increase the disease course, hospital stay and increase risks of complications like infections including necrotizing fasciitis and carry high morbidity and mortality.
Usually degloving soft tissue injury are high energy trauma. Abdominal wall degloving injuries are associated with lower limb and pelvic fractures, genitourinary, anorectal and abdominal viscera injuries. A multidisplinary approach involving plastic, orthopedic, general surgery and urology is needed.2,3
24 year old pregnant female patient presented to Emergency Room with history of road traffic accident bike versus trailer. On arrival she had tachycardia with heart rate of 111/min, BP 110/75mmHg, SpO2 99, RR18/min. On taking brief history she was gravida sixth 24weeks pregnant, with no known co morbid. Patient was assessed by general surgery, plastic surgery, orthopedic and obstetric team she was conscious oriented, with regular breathing pattern, and hemodynamically stable with severe pain recorded on Visual Analogue Scale as 8/10. She had inferior pubic rami fracture on X-Ray. E-FAST was negative. She was diagnosed with extensive degloving injury of lower abdomen involving lower abdomen and right thigh (Figure 1) Patient was resuscitated with fluids; multimodal analgesia was given to reduce pain and was shifted to high dependency unit. Multiple teams were involved including Orthopedic, Plastic, General surgery and Gyne Obs. All came on final decision for keeping the baby as it was healthy and viable and not causing immediate threat to mother life. Anesthetic management included arterial line in left radial artery, central line was passed in right internal jugular vein. Induction done with fentanyl, propofol and rocuronium. Standard monitoring done eg, ECG, pulse oximetry, invasive blood pressure, temperature and end tidal CO2 Serialdebridement with wound washouts were done combine by orthopedic and plastic surgery team, after 7 sessions of debridement VAC dessing was applied which was changed alternate days. After 25days of admission wound become healthy and granulating then plastic surgery took the decision of doing Split thickness skin graft (Figure 2). Patient develop pseudomonas graft infection (Figure 3), Inj. Imipenem was started. Patient responded to treatment. Patient was mobilized on 30th day after discussion with orthopedic about weight bearing.
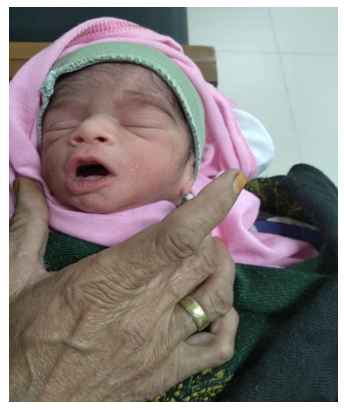
Figure 3 Elective c section (due to breach presentation on 34week) was done via vertical incision above graft.
Elective c section (due to breach presentation on 34week) was done via vertical incision above graft on 27Oct 2018 and baby girl 2kg delivered. She was discharged on 5th postoperative day.
The management of obstetric trauma can be quite complicated to be managed and especially if it is associated with other injuries like degloving of extremities, abdominal wall and orthopedic because it is associated with acute and long term consequences.1,2 For degloved skin primary goal is to save the remaining salvageable skin and prevention of infection and serial debridement’s and then reconstruction. Multidisciplinary approach is required for patients, which unit will take the patient is the major problem of conflict. Initial assessment and management is crucial for the long term outcome of patient.3,5 There are other many ways to manage extensive degloving injuries including using cryopreserved split-thickness skin grafts acquired from degloved flaps, artificial dermal replacement, or VAC therapy. VAC dressing helps in developing healthy bed before grafting and better reattachment of avulsed skin and placement of graft post grafting. The important point is to decide which tissue should be protected and which should be removed.4,8 Some authors have reported using a ring fixator to manage lower-limb degloving injuries; the fixator eventually helps prepare the wound bed for grafting, eases the application of graft tissue, facilitates graft care, and allows for passive mobilization of joints. But still, the more common technique is radical debridement followed by immediate application of a full-thickness skin graft.5,6,7
In this case patient had lower limb abdominal degloving injuries along with viable pregnancy so she was admitted in HDU after mutual discussion with all teams involved and serial debridement’s done timely, VAC dressing helped in making bed for the graft, and then split thickness graft helped in covering the wound. As baby was breech on ultrasound decision of vertical C section was taken by obstetrician to avoid affecting skin graft. Moreover the emergency duty doctor should always think of the possibility of a co-existing pregnancy whenever managing any woman within the reproductive age group involved in RTAs.
None.
The author declares that there is no conflict of interest.

©2019 Naz, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.