MOJ
eISSN: 2381-179X


Osteomyelitis as a consequence of an infected diabetic foot ulcer is a complication of diabetes and an important risk factor for lower extremity amputation. Thus, the administration of antibiotics is mandatory.
We report a case of a 72-year-old man with a history of type 2 diabetes mellitus admitted to our hospital due to osteomyelitis complicating an infected ulcer of the first toe of the right limb. Although afebrile, he had leukocytosis and dyspnea (PEDIS 4 infection according to IWGDF). He received intravenous treatment with antibiotics. From the second hospital day, he presented redness, edema and warmth of his left leg and foot. Inflammation signs worsened during the next days (redness more intense, with eczematous plaques at the margin and small white patches). He was misdiagnosed with severe cellulitis of the left limb, and another antibiotic was added to regimen. However, since his general condition was ameliorating, photo dermatitis was though to be an alternative diagnosis. Indeed, his left limb was exposed to sun due to his bed placement. His bed was moved away from window and he was instructed to avoid direct sunlight. On the following days, he presented a dramatic improvement of his left limb clinical image, so photo dermatitis diagnosis was established. The drug that was incriminated was levofloxacin. Patient was discharged in good shape, still on quinolone antibiotics, to complete three months’ osteomyelitis treatment.
Keywords: diabetes mellitus, diabetic foot, diabetic foot infection, antibiotics, photosensitivity, photoallergy, drug adverse reactions, quinolones, levofloxacin
Diabetic foot ulcer (DFU) is a chronic and common complication of diabetes mellitus which is a major health care problem with significant socioeconomic burden. DFU’s yearly incidence ranges from 2% to 4% in developed countries.1
DFU complications are a significant source of morbidity and mortality. With appropriate wound care, off-loading and diabetic treatment regulation, DFU can heal. Osteomyelitis is one of the most common expression of diabetic foot infection and an important risk factor for minor or major lower-extremity amputation. The primary aim of treatment of diabetic foot problems is limb preservation. Thus, the administration of antibiotics for the treatment of osteomyelitis is mandatory.2
Unfortunately, many antibiotic agents are associated with skin minor or major adverse events. Fluoroquinolones often cause photosensitivity reactions.3–5 Nalidixic acid, the prototype of quinolones, is a well-known photosensitizer. Other members of this group also posses a similar adverse effect. Ciprofloxacin has an estimated incidence of skin adverse effects in about 1% of patients, most commonly skin rashes or pruritus, generally mild to moderate in severity. Clinically, photosensitivity reactions mimic those of sunburn, with erythema and edema in the milder forms, and painful blistering with subsequent peeling when severe. Photosensitivity reactions occur as a result of fluoroquinolone photodegradation, and the molecule's ability to generate free monovalent oxygen radicals. Halogenation at the C-8 position is responsible for many of the photosensitivity reactions that occur during fluoroquinolone treatment.6
Therefore, the treatment management of DFU and osteomyelitis may be difficult in patients who present drug-induced adverse events such as phototoxicity and photoallergy. Also, the clinician must be familiar with this skin adverse reaction, because it can be mistaken as contiguous soft tissue infection.
We present a case where the administration of levofloxacin to a patient with osteomyelitis upon Charcot foot syndrome caused dramatic limb phototoxicity reaction that was initially misdiagnosed as infection aggravation.
A 72-year-old man (BMI: 27kg/m2) with type 2 diabetes on glucose-lowering tablets (HbA1c=5, 3%) attending our Diabetic Foot Clinic was admitted to hospital due to an infected DFU of the first toe of the right lower extremity. The patient had a history of Charcot foot syndrome of the left lower extremity diagnosed four years ago, and amputation of the third toe and fifth toe/metatarsal of the right lower extremity due to DFU infection two years ago. He also had peripheral arteriopathy and had undergone angioplasty in both lower extremities.
The patient had an infected DFU of the dorsal surface of the first toe probed to bone. He had “sausage toe” (1st toe) suggesting osteomyelitis, and also soft tissue infection of the forefoot (Figure 1). Although afebrile, he had orthopnea and blood tests showed high levels of inflammatory markers {erythrocyte sedimentation rate (ESR)64mm/h, white blood cells (WBC) 12,080/μL, and C-reactive protein (CRP) 232mg/L (normal values:<3.14mg/L)}. Infection was therefore classified as PEDIS 4, according to International Working Group on Diabetic Foot.7 X-ray showed intraphalangeal joint and distal phalanx lesions of the 1st toe, and gas into soft tissues (arrows) (Figure 2A) (Figure 2B). He was started on diuretics, acenocoumarol, clopidogrel, pentoxyphylline, and intravenous antibiotics (levofloxacin - since he reported recent use of amoxicillin/clavulanate - and clindamycin).

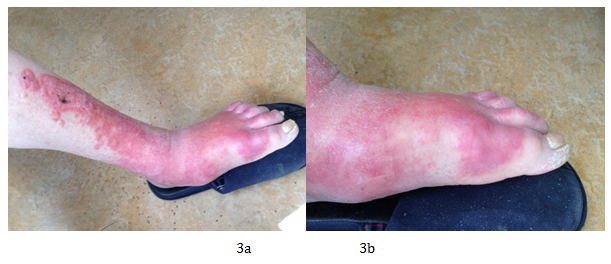
The day after admission, orthopnea hadsubsided, but patient presented redness, edema and warmth of the external part of his left leg and foot. Four days later, right foot inflammation had dramatically improved, but, on the contrary, left foot condition had worsened. Linezolid was added to the therapeutic regimen and clindamycin was switched to metronidazole. Ulcer cultures revealed methicillin-sensitive Staphylococcus aureus (MSSA), sensitive to quinolones. On the 8th hospitalization day, plain X-ray was without gas, CRP was reduced to nearly half (148mg/L), right foot had improved but left leg and foot were worse, with redness more intense, with eczematous plaques at the margin, while small white patches were included (Figure 3A) (Figure 3B). Then, since patient’s health was ameliorating, photo dermatitis was thought to be an alternative diagnosis to severe left lower extremity cellulitis. Indeed, patient’s bed was by the window, weather in Athens was warm and sunny at that time of year, and red leg part was facing towards the window and exposed to sun. He was moved to another bed away from window, and instructed to avoid direct sunlight. Also, levofloxacin was changed to ciprofloxacin. Three days later, lower extremity redness had dramatically improved, so photosensitivity diagnosis due to levofloxacin was established. There was no need of topical or systematic corticosteroid use.
Fifteen days after admission, patient was discharged in good shape (Figures 4A-4C), while inflammatory markers were significantly reduced (ESR=52mm/h, WBC=9210, CRP=25mg/L). He was given instructions to avoid sun exposure, offload right leg and wear customised shoes. He received moxifloxacin and clindamycin petros as outpatient. After three months’ total duration of antibiotic therapy as for 1st toe osteomyelitis, the patient presented with complete healing of his DFU and his symptoms of photo dermatitis had completely disappeared.
Unfortunately, diabetic foot soft tissue infection with or without osteomyelitis consist a common complication of diabetes mellitus. Osteomyelitis as a result of an infected DFU may lead to amputation and limb functionality loss. Additionally, the presence of Charcot foot syndrome is a serious and limb-threatening lowerextremity complication of diabetes. A lot of patients with a history of diabetes present DFU one or more times during their lives and unfortunately their therapeutic management, especially in the presence of osteomyelitis, is very difficult. These complications require the administration of antibiotic agents that, like all drugs, are associated with minor or major adverse events.
This case report has to do with a not very common skin adverse event of levofloxacin, and more specifically photosensitivity. It is known that in general, fluoroquinolones may cause phototoxic or photoallergic reactions as adverse events. Several studies have reported these adverse events. Unluckily, these adverse events may complicate the management of an already difficult situation such as DFU and osteomyelitis. As a consequence, the choice of the ideal antibiotic agent is quite difficult due to antibiotic agent’s adverse events and antibiotic resistance.
Regarding our patient, photosensitivity reaction caused by quinolone levofloxacin differed from classical sunburn, consisting of intense redness and edema with eczematous plaques at the margin, while small white patches were included. It was strictly limited to sunlight-exposed areas of unilateral leg and foot. Photosensitivity reaction was initially misdiagnosed as severe soft tissue infection, and this misguided us to add another powerful but expensive antibiotic, i.e. linezolid, to the therapeutic regimen.
We report a case where the administration of quinolone antibiotic levofloxacin to a patient with an infected DFU and osteomyelitis caused severeleg anf foot photodermatitis, that was initially misdiagnosed as severe soft tissue infection. Clinician must always bear in mind quinolone photosensitivity reactions, and instruct quinolone-treated patients to take direct sunlight precautions.
This study report work has supported under the unparallel supervision and guidance of Hon'ble Dr. Ramesh S. Paranjape (Former Director & Renowned Scientist National AIDS Research Institute, Pune). I express my sincere gratitude towards him for motivation and being great knowledge source for this work.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.