MOJ
eISSN: 2381-179X


Rheumatoid arthritis is an inflammatory condition that causes a negative effect in patient well-being. Fibroblast growth factor participates in the pathology of rheumatoid arthritis through its proliferative, inflammatory and angiogenic activities. Dobesilate, an inhibitor of fibroblast growth factor shows marked anti-proliferative, anti-inflammatory, and anti-angiogenic activities. Our study shows that intraarticular application of dobesilate is effective in reducing symptoms and signs in patients with chronic knee rheumatoid arthritis.
Keywords: rheumatoid arthritis, dobesilate, etamsylate, intraarticular application, fibroblast growth factor
Inflammation contributes to the pathogenesis of rheumatoid osteoarthritis through formation of various catabolic and pro-inflammatory mediators which alter the balance of cartilage matrix degradation and repair.1 In this condition, disturbed synovial and granulation tissue (so-called pannus formation) erodes and destroys the articular surface, and also invades subchondral bone tissue in part through osteoclast-like giant cells activity. Treatment of arthritis aims to control pain and maintain or improve physical function and quality of life. Currently, guidelines for the treatment of refractory knee rheumatoid arthritis recommended the use of intraarticular glucocorticoids. However, there is a big amount of data showing that this treatment frequently produces insufficient benefit with the associated risk of undesirable side effects.2 Drugs that inhibit joint destruction are known as disease-modifying antirheumatic drugs (DMARDs) such as sulfasalazine, antimalarials, penicillamine, gold, methotrexate, azathioprine, leflunomide and cyclophosphamide.3 These drugs are not always effective and frequently may lose effectiveness with time or may cause adverse effects. Therefore alternative DMARDs are needed and one class of new biologics agents have been developed as tumor necrosis factor alpha (TNF-α) inhibitors (adalimumab, etanercept, infiximab). However, a high risk of serious infection could be associated with anti-TNF-α therapy.4 Furthermore; the cost of anti-TNF-α therapy could limit its use. For all these reasons, novel but safe and efficient new therapy seems desirable for treating rheumatoid arthritis and its sequelae. Since clinical and animal data have been supporting a key role of fibroblast growth factor (FGF) in arthritis pathophysiology,5–11 its inhibition may be an attractive mean for arthritis treatment. In this context, we evaluated the local administration of dobesilate in solution, an inhibitor of fibroblast growth factor (FGF) activities, whose anti-inflammatory and anti-angiogenesis activities have been shown recently in several diseases and animal models.12–15 Dobesilate is a synthetic vasoactive drug that has been used orally as vasculotropic, for many years with a good safety profile.16 However oral administration is not the best choice for dobesilate to reach the adequate concentration at the joint cavity. Dobesilate has a very low solubility at the acidic pH of the stomach, and further, readily oxidises at the duodenal pH. Accordingly, a local delivery seems a better choice in order to reach appropriate therapeutic concentrations of dobesilate in the case of well-delimited targets, as is the case of knee rheumatoid arthritis. We report here that local intraarticular application of dobesilate solution improved symptoms and signs in knee rheumatoid arthritis.
Five patients with chronic knee rheumatoid arthritis joint participated in this study. After approval of our ethical committee, patients signed an informed consent form, which includes a comprehensive description of the proposed procedure with dobesilate. Clinical assessment of rheumatoid arthritis was evaluated at baseline, seven days and two months after dobesilate injection according to the concepts of the World Health Organization’s International Classification of Functioning Disability and Health (Geneva 2001). Temperature, hyperaemia, effusion/swelling and pain were evaluated. Temperature was measured using a contactless infrared thermometer. Clinical signs were graded using the following scale: 0: no signs of involvement, 1: moderate, 2: high and 3: severe. Intraarticular dobesilate injection was administered into a single knee as a 12.5% solution (2ml) of diethylamonium2, 5-dihidroxy benzenesulfonate (etamsylate, Dicynone®, Sanofi-Aventis. Paris, France). Mean clinical scores before and after one week of treatment with dobesilate were compared by paired t-test. A p<0.05 was considered significant.
After one week of treatment all clinical scores were significantly reduced (Figure 1) and the clinical improvement was maintained after two months follow-up. Patients did not show any apparent side-effect that may be attributed to the treatment. Rheumatoid arthritis is an inflammation-dependent disease. The hallmark of this condition is the progressive destruction of articular joints characterized by invasive synovial hyperplasia and pathological neovascularisation.1,2 Fibroblast growth factor (FGF) derived from synoviocytes may play a role in rheumatoid arthritis in stimulating their proliferation and angiogenesis.5–11 It has been reported in an animal arthritic model that FGF over expression accelerated disease severity by increasing inflammation, swelling, angiogenesis and osteoclasstogenesis, suggesting that FGF may affect disease progression.8 In addition, administration of an anti-FGF antibody in rats attenuated arthritic clinical symptoms and histopathological alterations.8 Furthermore increased synovial fluid levels of FGF are associated with greater disease severity.7 Thus, local inhibition of FGF may represent an attractive approach for the treatment of rheumatoid arthritis. Dobesilate is a powerful inhibitor of FGF that shows a markedly anti-inflammatory, anti-proliferative and anti-angiogenesis activity in several inflammations and angiogenesis-dependent diseases.12–16 It seems obvious that all these activities may contribute to the clinical improvement of dobesilate in knee arthritic patients. Furthermore, the consequences of inhibition of FGF production by dobesilate are the direct inhibition of cell proliferation and angiogenesis. Consequently, FGF deserves further attention as a possible therapeutic target for the treatment of subject with rheumatoid arthritis.
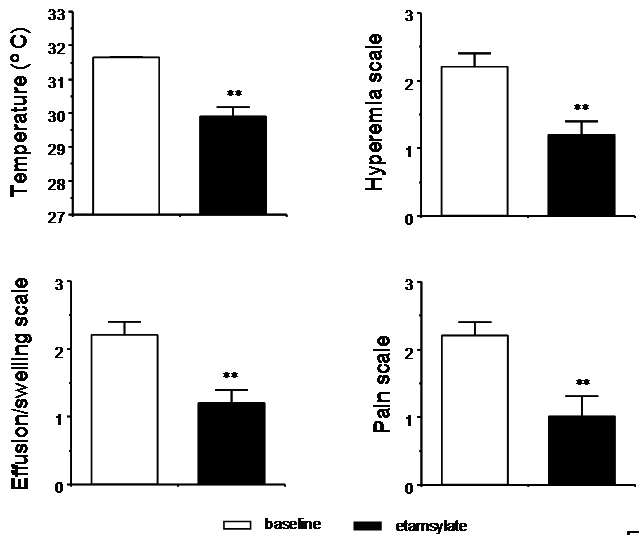
Figure 1 Effect of etamsylate in knee rheumatoid arthritis. Improvement of clinical manifestation of knee rheumatoid arthritis by single intraarticular injection of etamsylate in five patients. Data collected before and seven days after injection are expressed as mean SEM. Results were compared by paired t-test.*** indicates p<0.01 vs baseline.
In this report we present a preliminary assessment of the efficacy of the local administration of dobesilate in patients with chronic knee rheumatoid arthritis. We show that intraarticular dobesilate relieves the signs and symptoms in patients as early as one week after treatment. No relevant safety issues were observed along the study, in agreement with the good safety profile of this drug. Large scale therapeutic trials are obviously needed for more definitively establishing the efficacy of this treatment.
None.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.