MOJ
eISSN: 2381-179X


Background: Inguinal hernia is one of the more frequent pathology to be treated by general surgeons. The presentation of urinary bladder herniation is less common, with a reported incidence near 0.36%-1% of cases. Most cases course asymptomatic, but urinary symptoms could be presented and in a few cases acute renal failure have been reported.
Case: We present the case of a 52-year-old man with a giant left inguino-scrotal incarcerated hernia. He has pathological background including multiple urinary tract infections and 2-years of evolution with a left inguinal hernia. He refers dysuria, urinary frequency, pushing, urgency and voiding in two times, needing partial reduction of inguinal hernia to complete (Mery sign). Previous 12hours presented acute urine retention, with increasing left inguino-scrotal volume, in duration and severe pain, reason why he looked for hospital attention. At physical exam with analgesic position, glasgow 15, arterial tension 240/140mmHg, 96 beats per minute, 26 breaths per minute, abdomen without compromise, left inguinal region with inguino-scrotal no-reductible hernia, painful at maneuvers and edematized, without vascular compromise signs. Both legs with edema ++/+++, normal tendon reflexes and distal perfusion. Acute urine retention was solved by a 18 French foley without complications. Blood chemistry evidence acute kidney injury reporting Creatinine 1.5mg/dL, Urea 75mg/dL, and BUN 35mg/dL. Hematological parameters reports systemic inflammatory response with white blood cells 16200/mm3 without neutrophilia and other parameters within normal values as hemoglobine 13.8g/dL, hematocrit 43% and platelets 448000. Urine general exam with infection data including leucocites>10 μL, Nitrites+, Proteins 4g. Prostate Specific Antigen <2.5ng/mL. Renal, bladder, inguinal and testicular ultrasounds were practiced and reported: Bladder displacement by left inguinal canal and scrotum. Both kidneys, ureters and testis with normal characteristics. For the high suspect of urinary bladder herniation as the acute renal failure origin a retrograde cystogram was scheduled, finding in filling plate contrast material in urine bladder with 90% displacement to the scrotum by left inguinal canal. In post voiding projection residual urine is observed in left scrotum. During hospitalization the emergency hypertensive crisis was solved during first 24hours and Lichtenstein hernioplasty was scheduled. A giant paraperitoneal scrotum cystocele was found, without ischemic signs. After three days renal function was normal with creatinine reduction to 0.8mg/dL, and antihypertensive medication were diminished progressively until day 15 when was suspended and foley removed. At six months follow up he remains asymptomatic.
Conclusion: In big inguino-scrotal hernias with urinary symptoms, bladder herniation must be suspected for the high rate of complications associated ranging from repetitive urinary tract infection to acute or chronic renal failure. Diagnosis confirmation allows surgery planning and diminishes associated morbidity.
Keywords: herniation, acute renal failure, hernia complications, giant hernia
Inguinal hernia is one of the most frequent diseases to be treated by general surgeons. It comprise 70 to 75% of all abdominal wall hernias, are more common in men, 96% of groin hernias are inguinal and 4% femoral. The risk of inguinal hernia development along life is 25% in men of all ages.1 The acute presentation could include herniation of intra abdominal structures like omentum, small bowel or colon. Bladder herniation have been reported in a few cases, some of them associated with big inguinal hernias or diverticular deformation of bladder wall included in the sac, sometimes with acute or irreversible renal failure.2 Acute kidney injury (AKI) is a condition that affects kidney structure and function, defined by an abrupt decrease in kidney function that includes, but is not limited to, acute renal failure. The etiologies include a broad spectrum of causes including acute postrenal obstructive nephropathy. AKI include 3 stages taking in account serum creatinine and urine output, with the first stage characterized by an increase in serum creatinine 1.5-1.9 times baseline or >0.3mg/dl increase or an urine output increase of <0.5ml/kg/h for 6-12hours.3
Case
We present the case of a 52-year-old man presented to emergency room with a giant left inguino-scrotal incarcerated hernia. He has pathological background including multiple urinary tract infections and 2-years of evolution with the left inguinal hernia with progressive growth. He refers dysuria, urinary frequency, pushing, urgency and voiding in two times, needing partial reduction of inguinal hernia to complete (Mery sign). Previous 12hours presented acute urine retention, with increasing left inguino-scrotal volume, induration and severe pain, reason why he looked for hospital attention. At physical exam with analgesic position, Glasgow 15, arterial tension 240/140 mmHg, 96 beats per minute, 26 breaths per minute, abdomen without compromise, left inguinal region with inguino-scrotal no-reductible hernia, painful at maneuvers and edematized, without vascular compromise signs. Rectal examination with prostate gland 30g, without malignancy signs. Both legs with edema ++/+++, normal tendon reflexes and distal perfusion.
Acute urine retention was solved by a 18 French foley without complications. Blood chemistry evidence acute kidney injury reporting Creatinine 1.5mg/dL, Urea 75mg/dL, and BUN 35mg/dL. Rest of chemistry report albumin 1.9g/dL, total proteins 5.3g/dL, cholesterol 264mg/dL, trigliceridos 369mg/dL. Hematological parameters reports systemic inflammatory response with white blood cells 16200/mm3 without neutrophilia and other parameters within normal values as hemoglobine 13.8g/dL, hematocrit 43% and platelets 448000. Urine general exam with infection data including leucocites >10μL, Nitrites +, Proteins 4g. Prostate Specific Antigen <2.5ng/mL.
Renal, bladder, inguinal and testicular ultrasounds were practiced and reported: Bladder displacement by left inguinal canal and scrotum. Both kidneys, ureters and testis with normal characteristics. For the high suspect of urinary bladder as the acute renal failure origin a retrograde cystogram was scheduled, finding in filling plate contrast material in urine bladder with 90% displacement to the scrotum by left inguinal canal (Figure 1A). In post voiding projection residual urine is observed in left scrotum (Figure 1B).
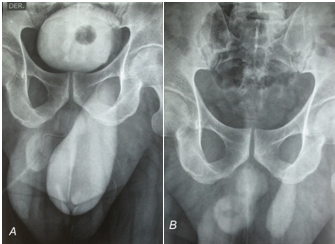
Figure 1 A. Excretion Urography showing urinary bladder incarceration.
B. Post void view with residual urine in herniated bladder.
During hospitalization the emergency hypertensive crisis was solved during first 24hours with three antihypertensive drugs and hernioplasty was scheduled. We perform a transverse suprapubic incision and dissect the planes until spermatic cord was shown. This structure had a 3cm diameter. Dissection of the spermatic cord and reference of it was done digitally, the cremaster muscle was opened longitudinally and dissected out of the reference. An indirect inguinal sac and a giant paraperitoneal scrotum cystocele was found, without ischemic signs, a deep inguinal ring diameter >4cm with epigastric vessels displacement and weak inguinal floor. After dissection of the urinary bladder (Figure 2), it was reduced with the sac to abdominal cavity, a simple stitch of polypropylene 3-0 to close deep inguinal ring and a Lichtenstein hernioplasty with a 10x5cm mesh was scheduled. After three days renal function was normal with creatinine reduction to 0.8mg/dL and antihypertensive medication were diminished progressively until day 15 when was suspended and foley removed. At six months follow up he remains asymptomatic.
Bladder herniation pathology includes inguinal hernias factors like inguinal floor weakness, bladder wall weakness with pericistitis and distal urinary flow obstruction that predispose intrabladder high pressure, for this reason prostatic hypertrophy is frequently associated. For this reason the incidence about 0.36-3% increase to 10% of cases in patients older than 50years, with high prevalence in male sex (27% vs 3%, male vs female).4
Some patients could course asymptomatic.5 Symptomatic patients would refer urinary symptoms like dysuria, urgency and frequency of voiding, the last of these presented in two times, requiring hernia partial reduction to complete voiding (Mery sing). Less frequent signs include ipsilateral nephric colic, hematuria and in a few cases renal failure.6
Given the patient duration of signs, age and progression in size of the inguinal hernia as acquired cause is most likely than congenital one.7
The diagnostic procedures include ultrasound to confirm bladder location in cases of inguinal hernia with clinical history of urinary symptoms. Excretory urography and retrograde cystography could be a valuable resource too previous to surgery and have been used along history. In this case by the acute kidney injury an excretory urography can’t be done. The best image study in this case is CT scan.8
Treatment must include and extra peritoneal hernioplasty with mesh, associated with correction of any obstructive process in the inferior urinary tract, and, if renal impairment persist the use of peritoneal dialysis or hemodialysis must be started.9In our case after urine acute retention was solved and inguinal hernioplasty done, renal function improved in a few days and do not require other procedures.
Bladder herniation is an infrequent pathology that could increase morbidity associated with inguinal hernia, and must be highly suspected in cases of urinary symptoms associated. The better diagnostic imaging to confirm include retrograde cystography and computed tomography to confirm bladder inclusion and surgery planning. In cases of bladder herniation diagnosis surgery must be scheduled immediately for the high risk of repetitive urinary infections and renal injury by distal obstruction, with or without correction after hernioplasty depending on evolution time.
None.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.