MOJ
eISSN: 2471-139X


Research Article Volume 5 Issue 3
University Clinic of Surgery St. Naum Ohridski Skopje, Macedonia
Correspondence: Antonio Gligorievski, University Clinic of Surgery St. Naum Ohridski Skopje, Macedonia ul. Vasil Gjorgov br. 28/25, 1000, Skopje, Macedonia
Received: May 10, 2018 | Published: June 22, 2018
Citation: Gligorievski A. US diagnosis of acute appendicitis. MOJ Anat & Physiol. 2018;5(3):225–229. DOI: 10.15406/mojap.2018.05.00198
Introduction: Acute appendicitis is the commonest condition requiring acute abdominal surgery. The perforation of the appendix is the most common complication. The fast and accurate diagnosis, as well as the timely surgery could decrease the risk of rupture and minimize the consequences.
Aims: The aim of the study was to demonstrate the value of the ultrasound (US) as an excellent diagnostic modality in evaluation of the appendix as well as to assess further treatment of acute appendicitis based on US study.
Methods: We present 97 cases, which were undergone on US examination of the abdomen with special accent on appendicle region. For exploration of the appendix, we used a linear probe from 7, 5 MHz.
Results: According of US findings the patients were divided into two groups: I (A) group with the signs of acute appendicitis - 61 cases and II (B) group where the signs of acute appendicitis were absent - 36 cases. From the group I (A) 57 patients were undergone on operative treatment and the US diagnosis of acute appendicitis was confirmed. From the group II (B) 7 patients underwent on operative treatment. We made the comparison between the US findings, operative and histology findings and our results correlated with the results from the literature data.
Conclusion: US are an extremely valuable diagnostic method in evaluation of the appendix with high diagnostic accuracy especially in the presence of acute inflammatory changes, with possibilities to plan further operative treatment.
Keywords: appendix, uncompressible appendix, acute appendicitis, US
Acute appendicitis presents as an acute inflammation of the appendix and it is the commonest condition requiring acute abdominal surgery.1 About 7% from the population will have inflammation of the appendix during their lifetime, and the peak incidence is in the second and third decades of life.2,3
The classic symptoms of the acute appendicitis for the first time were described by Fitz in 1886. According the histology there are different stages of the acute appendicitis as follows: early appendicitis (appendicitis acuta recens); appendiceal phlegmon (appendicitis suppurativa acuta), gangrenous appendicitis (appendicitis acuta gangraenosa) with perforation that follows.
Anorexia, nausea, vomiting and pain are the commonest symptoms related to the acute appendicitis. The pain begins in the epigastria, gradually moves to the periumbilical region and finally over a period of 1-12 hours, localizes in the right lower quadrant in more than 50% of the patients i.e. with sensitivity and specificity of 80%. The pain becomes diffuse in peritonitis with the direct or rebound tenderness of the abdominal muscles. The duration of the symptoms longer than 36 hours is unusual in unperforated appendix.1
The obstruction of the lumen of the appendix is the principal cause for distension of appendix due to accumulation of intraluminal fluid. The obstruction has multiple causes, including lymphoid follicular hyperplasia, fechaliths, appendicoliths, parasites, foreign bodies, Crohn’s disease, primary or metastatic cancer, and carcinoid and cecum cancer.
The lymph and venous drainage allow bacterial invasion into the bowel wall and at the late stages perforation and penetration of the pus into the peritoneal cavity.
The diagnosis of the appendix is based on history, physical examination, laboratory findings, but one third of patients with acute appendicitis have atypical history and physical examination. In this group of patients the radiological methods have important clinical role.
Puylaert1 described technique for exploration of the appendix with dosed compression over the appendix using transabdominal transducer and he established the criteria that allow standardization of the ultrasound (US) study of the appendix. The criteria for the inflammation of the appendix are as follows: outer diameters that exceed 6mm; uncompressible appendix; absence of peristalsis; presence of the periappendicular fluid; appendicoliths; periappendicular infiltrate. The normal appendix cannot be visualized, but in most of the cases the inflammated one can be.
The perforation of the appendix is the most common complication. The fast and accurate diagnosis, as well as the timely surgery could decrease the risk of rupture and minimize the consequences.4
With use of US and CT and with use of the established criteria the timely and accurate diagnosis is made up with reduction of the number of the unnecessary surgery and the number of appendiceal perforation as well.5–8
To demonstrate the value of the ultrasound (US) as an excellent diagnostic modality in evaluation of the appendix as well as to assess further treatment of acute appendicitis based on US study. The use of US in diagnosis of the acute appendicitis has an objective to decrease the number of perforation as a result of the late diagnosis as well as the number of unnecessary laparotomy as a consequence of false positive history and physical examination.
If the cause of pain in right lower abdominal quadrant according to the US findings is the inflammation of the appendix to suggest further treatment.
We show the cases performed as an emergency cases at the Institute of radiology in cooperation with the Clinic for Abdominal Surgery in Skopje in duration of sixth month period.
We demonstrate 97 cases with history and physical examination of acute appendicitis, aged 15-57, with peak incidence in second decade of life, 36 (37,1%) are male and 61 (62,9%) are female (Table 1). For the exploration of the appendix we used ultrasound apparatus Toshiba sonolayer SL-250 so linear transducer of 7,5 MHz, with dosed compression. The dosed compression makes the air go away from the bowel loops and decreases the distance among the transducer and the appendix, with what we have better visualization of the appendix. The careful exploration of the ileocecal region is performed, and the leading points are: umbilicus, inguinal ligament Pupartty, ileopsoas muscle, cecum and the iliac artery and vein. After each exploration of the appendiceal region we performed examination of whole abdomen using 3,75 MHz transducer.
Age |
11-20 y. |
21-30 y. |
31-40 y. |
41-50 y. |
51-60y. |
Total |
Male |
19 |
11 |
3 |
2 |
1 |
36 |
Female |
36 |
16 |
5 |
3 |
1 |
61 |
Total |
55 |
27 |
8 |
5 |
2 |
97 |
Table 1 According to the gender and age of patients
Dominant age is between 11 and 20 years with 55 cases (56.7%) and females with 36 cases (37,1%).
The classic history of acute appendicitis is: pain in the right lower quadrant in all patients, nausea, vomiting and anorexia in most of the patients, slightly elevated temperature in 46 patients, peritoneal sign, localized tenderness on percussion in 12 patients; positive Rovsing sign, pain at the right lower quadrant during palpation, pain at the left lower quadrant in 23 patients, psoas sign during extension of the right thigh in 5 patients, obturator sign during internal rotation of the flexed right thigh in 3 patients and Dunfi sign of pain at the right lower quadrant in 7 patients. The duration of the symptoms is lesser then 48 hours in 80%, but it can be longer in elderly with appendiceal perforation.
From laboratory studies characteristic is moderate leukocytosis in 74% of patients from 10000 to 14000, and 26% had normal white blood cell count.
The basic US criteria for the diagnosis of acute appendicitis that we use are as follows: visualization of distended appendix fluid filled, appendix with diameter that exceed 6mm; appendiceal wall thicker then 3mm; absence of peristalsis and uncompressible appendix; forming of infiltrate around the appendix and free fluid into the appendiceal surrounding or into the abdomen.
In patients that we did not visualize the appendix, based on the US criteria there is no presence of acute appendicitis; and it is possible to obtain false negative results.
The inflammated appendix is visualized medial and inferior from the cecum, sausage-like, blind ending structure at the longitudinal plane or target sign (bull’s eye appearance) at axial plane.
The appendix on US study is demonstrated by: hypo echoic lumen, hyper echoic mucosa, iso echoic lamina propria, hyper echoic submucosa, hypo echoic muskularis and hyper echoic serosa. The increased size of the appendix is a sign for phlegmonous or gangrenous appendicitis (Figure 1). The present appendicolith is demonstrated as hyper echoic mass that fills in the lumen and gives acoustic shadow (Figure 2B). When the appendicolith should be visualized, the wall thickness and the compressibility are not the features for making the diagnosis of acute appendicitis. The gangrenous appendicitis has changes in echogenity in all layers and the same are with the uniform echogenity and cannot be distinguished (Figure 3A). If the ill defined or hypo echoic mass is seen that surrounds the appendix that presents the periappendiceal inflammation (Figure 4). The ill defined appendiceal wall is suggestible, but not diagnostic for the periappendiceal process. The fluid presence into the appendiceal surrounding, with appendiceal wall echogenity changes is US feature for perforation (Figure 3B). The positive lymph nodes are oval hypo echoic and they don’t change the shape on compression.
The patients based on the US findings are divided into two groups: I (A) group with the signs of acute appendicitis - 61 cases and II (B) group where the signs of acute appendicitis were absent - 36 cases (Table 2). From the group I (A) 57 patients were undergone on operative treatment and the US diagnosis of acute appendicitis was confirmed. From the group II (B) 7 patients underwent on operative treatment.
In terms of the size of the appendix we divided the patients into two groups: group with the diameter up to 12mm where we have 39 patients and group with diameter greater then 12mm in size where we have 22 patients, from which 7 patients were with diameter greater than 17mm. In terms of the appendiceal wall thickness in 43 cases it was between 3 to 5mm, and in 18 it was greater than 5mm. In 13 patients we detected appendicoliths into the lumen of the appendix.
In all cases obstruction of the appendiceal lumen was caused by follicular hyperplasia, bowel contents, appendicolithes, except in one case where obstruction was caused by cancer of the cecum.
Based on the US finding we have 14 patients with early appendicitis (Figure 5), 31 patients with appendiceal phlegmon (Figure 2A) and 12 with gangrenous appendicitis (Figure 3A) from which 4 cases are with appendiceal perforation (Figure 6).
The group of patients that are with no remarkable signs for the presence of acute appendicitis, we have 7 cases with mesenterial lymphadenitis, from which 2 patients had clear US finding of acute appendicitis one month thereafter.
The correlation is done among the preoperative US diagnosis and the operative and histology findings with the accuracy: for the early acute appendicitis is 11/14, for the suppurative appendicitis is 25/31, for gangrenous appendicitis is 7/8 and for perforated appendicitis is 4/4, or in total 47/57 (82,45%) (Table 3).
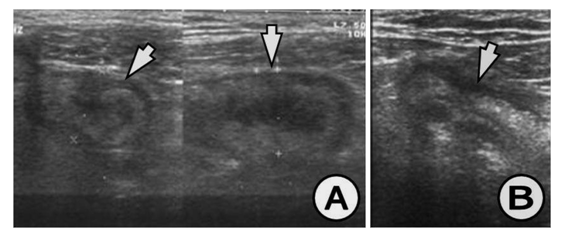
Figure 1 (A) Appendix increased in size, 17 mm in diameter, thickened wall greater than 6 mm, (B) Appendix with widened lumen with dense contents, with 18 mm in diameter and thickened wall greater than 5 mm. US finding for appendiceal phlegmon.

Figure 2 (A) Appendix increased in size, thickened wall, widened lumen, US finding for appendiceal phlegmon, (B) Clearly visualized appendicolith into the lumen of the appendix, which is with thickened wall and widened lumen, US finding for appendiceal phlegmon.

Figure 3 (A) Appendix in saggital and coronal plane, thicken and oedematous wall, with widen lumen, disturbed appendiceal architecture and surrounding infiltration, US finding for gangrenous appendicitis, (B) Appendix with thickened wall, widened lumen and periappendiceal fluid, US finding for gangrenous appendicitis.
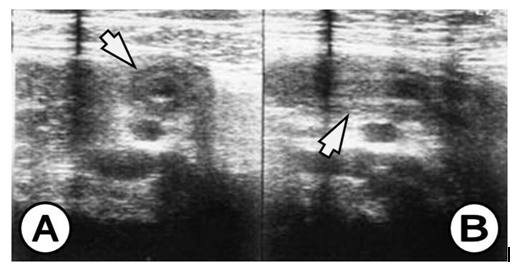
Figure 4 (A) Coronal view, appendix with thickened wall and surrounding infiltration, (B) Saggital view, appendix with thickened wall and surrounding infiltration, US finding for appendiceal phlegmon.

Figure 5 (A) Clearly visualized appendix, with diameter of 8,7 mm and thickened wall of 3,5 mm, US finding for early appendicitis, (B) Thicken wall of the appendix and widen lumen, US finding for early appendicitis.
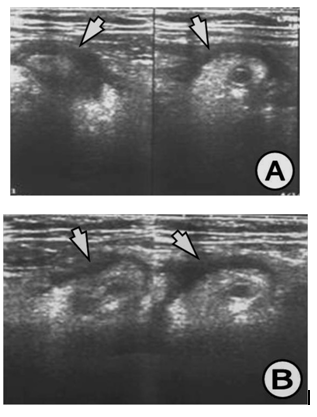
Figure 6 (A) US of acute appendicitis. (B) Appendix with widened lumen and thickened wall, disturbed echogenity, periappendiceal fluid, US finding for perforated gangrenous appendicitis.
US findings |
Surgery findings |
|
I (A) group (61 cases) |
Positive in 61 |
Positive in 57 |
II (B) group (36 cases) |
Negative in 36 |
Positive in 7 |
Table 2 According to the US findings and surgery findings
According to the US findings the patients were divided into two groups: I (A) group with US findings for acute appendicitis in 61 cases, surgery confirms 57 cases and II (B) group with negative US findings for acute appendicitis in 36 cases, which from 7 cases were false negative.
US findings |
Histology findings |
||||
EA |
APh |
GA |
PA |
Total |
|
EA |
11 |
3 |
|
|
14 |
APh |
2 |
25 |
4 |
|
31 |
GA |
|
1 |
7 |
|
8 |
PA |
|
|
|
4 |
4 |
Total |
13 |
29 |
11 |
4 |
57 |
Table 3 According to the US findings in correlation with histology findings
Abbreviations: EA, early appendicitis; APh, appendiceal phlegmon; GA, gangrenous appendicitis; PA, perforated appendicitis.
Acute appendicitis remains one of the most common surgical emergencies with a lifetime occurrence of 7%.9,10 We could tell that with the use of US in the diagnosis of the acute appendicitis there is decreasing of the unnecessary surgery, decreasing the number of the false negative findings and postponing the surgery only based on the history and physical examination. Early ultrasound detection and surgical intervention is the best way to manage acute appendicitis in order to reduce complications and mortality.10–13 Lee et al.,10 showed that the incidence of acute appendicitis increased in patients younger than 10 years and older than 50 years. The highest rate of acute appendicitis in our sample was found in the age group 11–20 years.
More publications suggest that the US has great diagnostic value in acute appendicitis. The prospective studies showed that in 18% to 26% of patients final diagnosis could be established with US and should undergo on surgery.1 With this method the number of the negative appendectomies is reduced on 8,5% do 13,2%.1 Skaane et al.5 Suggest high correlation among the operative and histology finding, and the sensitivity of the US method into the diagnosis of the inflammated appendix is 78,92%, and the specificity is 87 Dreuw et al.,4 in their study the US finding compare with the clinical diagnosis and the histology finding. For the appendiceal region mass the sensitivity is 100% and for appendiceal phelgmon is 88%. The specificity of the method is 97%, positive predictive value is 97%, and the negative predictive value is 47%. The US finding correlates with the operative finding in 87%.4
In most of the cases that valorize the contribution of US into the diagnosis of the acute appendicitis the sensitivity is from 75-90%, and specificity is from 86-100% and the diagnostic accuracy is from 87-96%.1,3,6,7,14,15
Most of the newly publications demonstrated that the greatest diameter of the appendix is >6mm, there is about inflammation in 93% of the cases.
According to Lane et al.,8 the sensitivity of the CT in diagnosis of the acute appendicitis is 90%, specificity is 97%, while the new publication demonstrate sensitivity of 96% and specificity of 98-99%.
According to Balthazar et al.,16 who analyzed the data from CT and US the sensitivity is 96% over 76%, specificity is 89% over 91%, accuracy is 94% over 83%, PPV is 96% over 95% and NPV is 95% over 76%.
Al-Ajerami17 report the overall specificity and sensitivity of 84.8% and 83.3% respectively, which showed that ultrasound has a relatively high specificity and sensitivity in diagnosing appendicitis especially with patients of normal weight. Our results compare well with other studies reported sensitivity 75%–98%, specificity 86%–100% with positive and negative predictive values of 91%–100% and 89%–99%.18–20
The barium enema in diagnosis of the appendix is with sensitivity of 80-100%. Its advantage is that the examination is simple with using simple materials and allows to be diagnosed other diseases such as Crohn’s disease, colon cancer, ischemic colitis that might simulate appendicitis. The disadvantages are: radiation, non diagnostic examination, insufficient examination and invasive examination. Due to all these disadvantages the barium enema is not adequate as a screening method for the diagnosis of appendicitis, especially in the era of US. In spite of the diagnostic value of the barium enema study for appendicitis it is not used as screening method.
In most of the cases the appendix has intraperitoneal location, and it could contact the parietal peritoneum when it is inflamed. In 30% of the cases the appendix could be hidden from the anterior peritoneum due to its pelvic or retro colic location.6 The poster lateral approach is better for the exploration of the retrocecal region.
The differential diagnosis includes: endometriosis, ovarian cyst or torsion, tubo-ovarial abscess, degenerative fibroids of the uterus, diverticulitis, Crohn’s disease, colon cancer, cholecistitis, bacterial enteritis, mesenterial adenitis and torsion of the omentum.
The number of the negative appendectomies varied from 16,7% to 47,2%, with mean of 26,4%.2 The false negative diagnosis are explained by perforation of the inflamed appendix from 9,6% to 32,2%, with mean of 22,6%.2 Ultrasound may not detect the appendix when it is retrocaecally located or if it lies deep in the pelvis.21–23 Indications for CT after sonography included retrocecal appendicitis, nonvisualization of the appendix by sonography, an equivocal findings with secondary signs of appendicitis, and negative findings with clinical concern for appendicitis.22,23 The negative appendectomy rate can be significantly reduced by using ultrasound coupled with clinical assessment and evaluation.24–26
We can conclude that the US has great diagnostic value in acute appendicitis. The advantage consists of: easy performance, noninvasive method, no radiation, short examination duration, the possibility for detection of other causes of distal abdominal pain, especially in pregnant women. The disadvantage is that the finding depends on the operator. The non visualized appendix is interpreted as non inflamed appendix, so it is from great importance the examination to be performed by experienced radiologist with attention and he would be able to accomplish maximal sensitivity.
If the examination with the dosed compression of the right lower quadrant is positive for the appendicitis, the surgery is recommended. If the finding is unremarkable, it is not enough to exclude appendicitis. In that case if the pain and the history are still present the follow up US is recommended for further observation by the abdominal surgeon.
With use of US and with use of exact established standards and criteria the timely and accurate diagnosis of acute appendicitis is allowed. It will reduce the number of the perforations and unnecessary surgery.
Dr. Antonio Gligorievski declares that there is no conflict of interest.
There are no sponsors for this article.
Ethical approval was not necessary for this article.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written informed consent is available for review by the Editor in Chief of this journal on request.

©2018 Gligorievski. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.