MOJ
eISSN: 2471-139X


Case Report Volume 11 Issue 1
1Department of Propaedeutics and Integrated Clinic, Federal University of Bahia (UFBA), Brazil
2Department of Dental Radiology and Imaginology, São Leopoldo Mandic, Brazi
Correspondence: Hannah Barros Simões, Department of Propaedeutic and Integrated Clinic, Federal University of Bahia (UFBA), Salvador, Bahia, Brazil., Tel +55(71)3283-9000
Received: January 27, 2024 | Published: February 9, 2024
Citation: Campos PSF, Barros H, Prado GD, et al. Uncommon size of a posterior stafne bone defect: case report. MOJ Anat Physiol. 2024;11(1):7-8. DOI: 10.15406/mojap.2024.11.00341
Introduction: The Stafne bone defect (SBD) is described as a well-defined, unilateral radiolucent area, usually in the region close to the angle of the mandible and below the mandibular canal. This asymptomatic condition, diagnosed in routine radiographic examinations, affects males between the 5th and 7th decade of life and does not require surgical intervention. The etiology of the condition is uncertain; however, the occurrence of SBD is often associated with salivary gland hypertrophy/hyperplasia.
Case presentation: On this report, we present a case of SBD, the posterior variant, exhibiting uncommon dimensions.
Conclusion: The Stafne bone defect is most often the result of failure of mandibular ossification.
Keywords: mandible, radiology, bone and bones, tomography
The Stafne bone defect (SBD), first described in 1942, is a rare, asymptomatic, usually unilateral condition, located in the posterior region of the mandible and below the mandibular canal. It more frequently affects men and presents radiographically as a radiolucent, circular or ovoid area with well-defined margins.1
Although the most common localization of SBD is the posterior region of the mandibular body and angle (posterior variant - SBDp), this type of defect may also manifest in the anterior region (anterior variant - SBDa) and in the mandibular ramus (variant of the mandibular ramus - SBDr).2 The prevalence of SBD varies between 0.1% and 0.48% and the condition most often affects males between the 5th and 7th decade of life.2
Considering depth and content, respectively, Ariji et al.,3 classified SBDp as Type I (depth of the defect does not reach the buccal cortex of the mandible), Type 2 (the defect reaches the buccal cortex, without distending it) and Type 3 (the defect reaches the buccal cortex and leads to its distension); Type F (fat-filled defect), Type S (defect filled with soft tissue - lymph node and/or connective tissue) and Type G (defect filled with glandular tissue). This classification is also valid for SBDa and SBDr.
The present article aims to report a case of SBD, the posterior variant, exhibiting uncommon dimensions, and to discuss its etiology.
The patient, a 41-year-old asymptomatic male, was submitted to multislice computed tomography for the purpose of evaluating a lesion on the right side of the mandible. The images revealed a bone defect on the lingual surface of the right mandibular body (SBDp), in the molar region, which extended from the base of the mandible to above the mandibular canal in the craniocaudal direction, and in the anteroposterior direction, from the height of the root of tooth 46 to close to the antegonial notch (Figure 1). The bone defect was observed to be filled with fibrous tissue, blood vessels, fat and a cervical lymph node of level IB (Figures 1–3). According to Ariji et al.,3 the defect was classified as Type 2S.
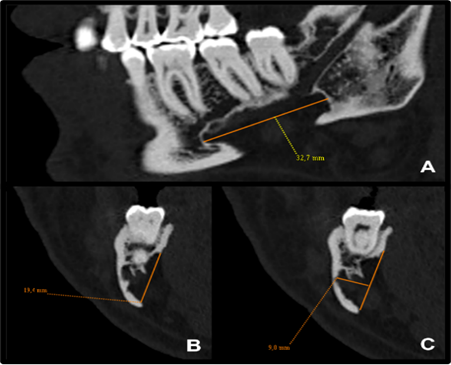
Figure 1 Sagittal (A) and coronal (B-C) multislice CT images, bone window, showing a posterior bone defect (SBDp) of unusual proportions (32.7 x 19.4 x 9.0mm).
Posterior SBDs are most commonly those with the largest dimensions. As they normally manifest below the mandibular canal, this fact supports the theory that an eventual increase in volume of the submandibular gland would lead to cavitation of the medial face of the mandible. Type 3G defects with buccal cortical distention3,4 have clearly made the relationship between the submandibular gland and the bone defect unquestionable, nevertheless, this type of defect is uncommon. Therefore, in the majority of cases, it is more reasonable to assume that the submandibular gland passively occupies the bone cavity.
Philipsen et al.2 considered the congenital origin of SBD unlikely, since there is no occurrence of these defects in children. However, we believe that it is not possible to rule out a congenital origin, since the bone defect would evolve with skeletal development, which is why it would only become visible later.
Stafne himself5 abandoned the hypothesis of congenital origin, supported by two cases of SBDp that developed in a middle-aged male patient over a period of ten years. Wolf et al.,6 also described a case of SBD in a middle-aged male patient, which developed over a period of eight years. Considering the age and sex of these patients, it is plausible to hypothesize that the development of SBDs occurred as a result of superficial ischemic bone necrosis, which would result in the formation of a progressively larger and radiographically visible cavity defect.
Despite the unusual dimensions of the case of SBDp presented in this report, the lesion did not reveal any glandular tissue within it, which reinforces the hypothesis that SBD was, in fact, an ossification defect of the mandible.7
The literature has reported that exploratory surgeries have usually harvested glandular tissue within the posterior variant of the Stafne bone defect,2 and this glandular tissue has occasionally been interpreted as being an ectopic parotid gland.8 We must remember that the submandibular gland is seromucous, but is of a predominantly serous nature, so that the anatomopathological examination may reveal only serous acini, which should not be interpreted as an ectopic parotid gland.
We must also bear in mind that sialoadenitis and pleomorphic adenoma (the most common benign tumors of the salivary glands) do not usually produce cavitation similar to that found in the Stafne bone defect. This fact weakens the hypothesis of the cause/effect relationship between the increase in gland volume and the manifestation of the Stafne bone defect even further because the gland expands to the side on which the resistance is lower. That is, it expands into the surrounding soft tissues.
In conclusion, we would say that the Stafne bone defect is most often the result of failure of mandibular ossification; it may also be a consequence of superficial bone ischemia and more remotely, a consequence of bone erosion caused by hypertrophy/hyperplasia of the salivary gland.
None.
Ethical approval: Not applicable.
Consent to participate: Informed consent was obtained from the subject described in this report.
Written consent for publication: Consent was obtained from the subject described in this report.
Availability of data and materials: There data are part of the personal collection of Professor Paulo Sergio Campos Flores.
Code availability: Not applicable.
Author contribution: PSF: Project development, data collection, data analysis, manuscript edit; HB: Project development, manuscript writing; GDP: Data analysis, manuscript writing; BSSF: Data analysis.
The authors declare that they have no conflict of interest.
There was no receipt of funds.

©2024 Campos, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.