MOJ
eISSN: 2471-139X


Research Article Volume 11 Issue 1
1Federal State Budgetary Educational Institution of Higher Education, Novosibirsk State Pedagogical University, Novosibirsk, Russian Federation
2JSC NPK “IMPULSE-project”, Novosibirsk, Russian Federation
Correspondence: Aizman Roman Idelevich, Doctor of Biology. Sciences, Professor, Head of Department, Scientific Research Institute of Health and Safety, Novosibirsk State Pedagogical University, Russia
Received: April 22, 2024 | Published: June 4, 2024
Citation: Golovina KO, Golovin AM, Aizman RI. The influence of the disk pump of assisted circulation of the left ventricular bypass on hemolytic blood parameters. MOJ Anat Physiol. 2024;11(1):20-24. DOI: 10.15406/mojap.2024.11.00344
Over the past two decades, rotary circulation pumps have been effectively used to treat patients suffering from chronic heart failure (CHF). However, prolonged contact of blood cells with a foreign surface of the pump can cause hemolysis, thrombosis, bleeding and other disorders. A possible solution to reduce the level of blood cells damage may be the introduction into clinical practice the pumps for maintaining blood circulation with a lower rotor speed - 2000-3000 rpm The purpose of this study was to study the effect of a developed by us disk pump for auxiliary circulation of the left ventricular bypass on hemolytic blood parameters.
Methods: A study of the effect of a disk pump of auxiliary blood circulation on human donor blood parameters was conducted using a special simulation stand (n=6) and experiments on laboratory animals (n=3).
Results: In studies on donated blood, the level of free hemoglobin (FreeHb) was 0.03±0.1 g/l for 4 hours of the experiment.
In animal studies, in the first two days after implantation of the pump, an increase in FreeHb was observed in the range from 0.01±0 to 0.05±0.1 g/l. Further, from the third day to the end of observation, fluctuations in FreeHb in the blood were in the range of 0.03–0.04 g/l. During the same period (1-3 days), there was a significant decrease in hematocrit (Hct), which was restored to background values by the 4th day. The concentrations of sodium, calcium, chlorine ions and blood pH remained virtually unchanged throughout the experiment, and the concentration of potassium tended to increase by the 5th-7th day.
Conclusion: The developed prototype of a disc-type auxiliary blood circulation pump for left ventricular bypass did not cause significant hemolytic, electrolyte and acid-base disorders in the blood during 240 minutes of experiment on the stand (in vitro) and during 7 days in an in vivo experiment. It allows to recommend this type of pump for short-term use as a promising heart replacement like a “bridge” to organ transplantation or for unloading the heart in patients with CHF.
Circulatory assist pumps provide minute volume of blood flow in patients suffering from end-stage chronic heart failure (CHF). In this case, long-term mechanical support involves prolonged contact and collision of blood cells with foreign surfaces, as well as very high mechanical loads caused by the rotation of the pump rotor.1 Despite the high resistance of erythrocytes to mechanical shear stress, prolonged exposure to the pumps circulatory assist causes cellular changes that are similar to the physiological changes that occur in aging erythrocytes during normal circulation, but they occur at an accelerated pace. Such changes lead to thinning of cell membranes, loss of phospholipids, increased membrane permeability, and leakage of lactate dehydrogenase (LDH), hemoglobin, which causes hemolysis.2 Hemolysis is a frequent complication, occurring in 60% of patients by 6 months of implantation.3 The main causes of hemolysis include: turbulent blood flow developed by the pump; high rotation speed of the pump rotor (more than 13,000 rpm); contact of blood cells with a foreign, insufficiently biocompatible implant surface; low or negative pressure in the flow, leading to cavitation.
Over the last two decades, rotary pumps have been predominantly used for mechanical circulatory support.4 Their distinctive feature is high rotor speed (7000-10000 rpm), which, as we believe, leads to erythrocyte injury. A possible solution to reduce the level of injury to blood cells may be the introduction into clinical practice of circulatory support pumps with a lower rotor speed of 2000–3000 rpm. But, on the other hand, a low rotor speed can provoke more intense thrombus formation. Pumps that provide a physiological blood flow volume of 5–6 l/min, as a rule, have a rotor speed of 7000–10,000 rpm. Accordingly, an assisted circulation pump with a rotor speed of 2000–3000 rpm should provide no less volume of minute blood flow. The purpose of this study was to study the effect of a circulatory assist disk pump with a low rotor speed on hemolytic blood parameters.
Description of the circulatory assist disk pump of left ventricular bypass
For research, a prototype of a disk pump for assisted circulation of the left ventricular bypass was used (Figure 1, 2). Figure 1 shows a schematic representation of a disc pump, Figure 2 shows its appearance.
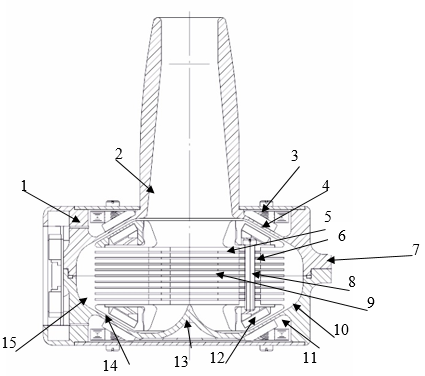
Figure 1 Disc pump for assisted circulation of the left ventricular bypass.
Where: 1 - upper half of the housing; 2 – inlet pipe; 3 – upper stator winding; 4 – upper stator; 5 – upper half of the rotor; 6 – connecting bushings; 7 – outlet pipe; 8 - fasteners; 9 – rotor discs; 10 – lower half of the housing; 11 - lower stator winding; 12 - lower stator; 13 – lower magnetic core; 14 – lower permanent magnets; 15 – lower half of the housing.
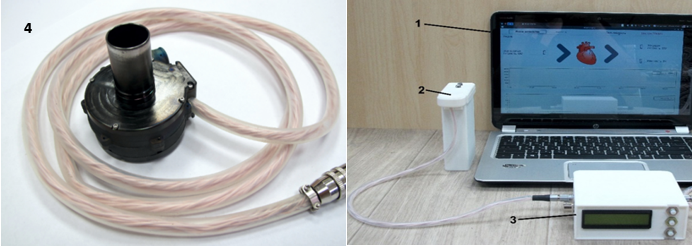
Figure 2 External view of the disk pump for assisted circulation of the left ventricular bypass.
Where: 1 - monitor, 2 - batteries, 3 - control system, 4 - disk pump.
The developed device consisted of an implantable disc pump and a control system. The disc pump casing consists of two parts - upper and lower. The casing is equipped with inflow and outflow cannulas. A combination of construction elements - stator with windings and rotor - make up the electric motor of the pump. The space between the discs of the rotor, as well as the space formed around the rotor inside the casing, serves for pumping blood. During the operation of the pump, the rotor rotates.
The control and power supply signals are applied to the stator windings via the power and control output.
An implantable disk assisted circulation pump is connected through an inflow cannula to the apex of the left ventricle and discharges the blood flow entering it into the ascending aorta. Thus, the pump ensures that blood is taken from the left ventricle and enters the systemic circulation. The device is intended for long-term support of the left ventricle of the heart of patients with progressive heart failure.
In our study, we evaluated the effect of a disc pump of the assisted circulation on several blood system parameters: bilirubin (ctBil), lactate (cLac), hematocrit (Hct), hydrogen index (pH), free hemoglobin (FreeHb), lactatedehydrogenase (LDH) and electrolyte concentrations of potassium (K+), calcium (Ca2+), sodium (Na+) and chlorine (Cl-).
The modified hemolysis index (MIH) and the normalised hemolysis index (NIH) are used to objectively assess the hemolysis characteristics of the pumps.
MIH is usually calculated using the formula:5
where Hb represents the total hemoglobin concentration in the blood at time zero (mg/l); Δ free Hb – increase in free plasma hemoglobin (mg/l) over the sampling time interval; V – circuit volume (l); Q – flow rate (l/min); Ht – hematocrit (%); T – sampling time interval (min).
In most of the works, the following formula has been used in normalised hemolysis index (NIH) calculations:6–11
Two types of studies were carried out: 1) on human donor blood, with a shelf life of no more than one day, using a stand that simulates the systemic circulation (n=6); 2) on laboratory animals in vivo (n=3).
Description of the experiment on a bench simulating the great circle of blood circulation
The appearance of the used stand is shown in Figure 3.
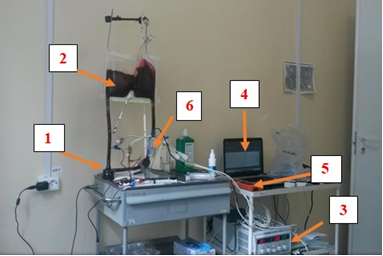
Figure 3 General view of the stand for studying the hemolytic properties of a disc-type circulatory support device.
Where: 1 – disk pump for auxiliary circulation; 2 – reservoir with blood; 3 – system for measuring pressure; 4 – laptop with control unit and software; 5 – flow meter; 6 – heat exchanger.
The circulatory circuit consisted of a 1-litre elastic blood reservoir and Tygon tubes, a heat exchanger integrated between the inflow and outflow lines. After installation, the circuit was filled with Ringer's solution in the volume of 500 ml with the addition of 10,000 units of heparin as an anticoagulant.12 In order to remove air bubbles in the stand system, the pump was started at a speed of 500 rpm. Next, half of the Ringer's solution (250 ml) was drained and donor blood in a volume of 450 ml was added to the system. The apparatus was operated at 2500 rpm with a capacity of 5±0.5 l/min in constant flow mode. In order to create hydraulic resistance, a screw clamp was used for dosed compression of the outflow line. The temperature was maintained at 37 °C using a heat exchanger. Before the start of each experiment, a baseline blood sample (zero sample) was taken to determine the initial level of controlled blood parameters: ctBil, cLac, Hct, pH, FreeHb, K+, Ca2+, Na+ Cl–. Characteristics of the level of hemolysis were assessed using the above formulas.6,13
Description of the in vivo experiment
In vivo experiments were performed on male calves of black and grey breed, average age 4 months, average weight 90 kg. The calves were monitored for 7 days.
During the experiment, the animal was under anesthesia. Tracheal intubation was performed with a tube with a diameter of 9 mm, after which it was fixed to the upper jaw of the animal and connected to the respiratory circuit of the anesthesia-respiratory apparatus for mechanical ventilation. Forced ventilation of the lungs was carried out with an oxygen-air mixture in a ratio of 50:50 with a sevoflurane content of 4-5 vol%. For assisted ventilation of the lungs, 100% oxygen with a similar content of sevoflurane was used until 100% oxygen saturation was achieved. A pulse oximetry sensor was fixed on the tail of the animal, sensors for recording ECG were attached to the chest, and a passive coagulator electrode was attached to the back.
Registration of functional vital parameters was carried out using an IntelliVueMP70 monitor (Phillips). During the experiment, central venous pressure (CVP) was monitored by catheterization of the right external jugular vein; blood pressure (BP) - by catheterization of a peripheral artery (ear, brachial). The pump was connected to the animal heart paracorporeally according to the scheme "apex of the left ventricle - descending section of the thoracic aorta". In order to form the outflow tract, an anastomosis was made between the vascular prosthesis and the aorta. The second end of the vascular prosthesis was connected to a Tygon silicone tube and the outflow tract was withdrawn (Figure 4).
All manipulations with animals were performed in accordance with Directive 2010/63/EU of the European Parliament and the Council of the European Union for the protection of animals used for scientific purposes, with the permission of the ethical committee of the National Medical Research Center. acad. E.N. Meshalkina. The first blood samples were taken from the animals before connecting the pump. After connecting the pump, blood samples were taken every 30 minutes for 4 hours. Subsequently, on the 1st day of connection - every hour, from the 2nd day of observation - 1 time per day. The blood test was carried out in the laboratory of the National Medical Research Center named after. acad. E.N. Meshalkin. A RADIOMETR ABL800 FLEX blood gas analyzer was used to process the samples. Statistical processing of the obtained results was carried out in MatLab programme. For each indicator, the mean value for the entire observation period and its error were calculated. The reliability of differences between groups was assessed by the parametric Student's t-criterion at p<0.05.14
At the end of six bench experiments, when the pump was operating at 2500 rpm, the pump capacity was 5±0.5 L/min, the outlet line pressure was 99.7±2.1 mmHg, the inlet line pressure was 12.1±2.1 mmHg, and the mean free hemoglobin (FreeHb) level was 0.03±0.01g/L (Table 1). Free hemoglobin indicating the level of hemolysis did not change during the time of the experiment on the stand (Figure 5).
|
Indicator name |
Number of blood sample (time, min) |
||||||||
|
0 (0) |
1 (30) |
2 (60) |
3 (90) |
4 (120) |
5 (150) |
6 (180) |
7 (210) |
8 (240) |
|
|
Haematocrit, Hct, % |
24,3±2,1 |
24,1±1,9 |
24,1±1,9 |
24±2,1 |
24,2±2,1 |
24,2±2,1 |
24,2±2,1 |
24,3±2,1 |
24,3±2,1 |
|
Haemoglobin, ctHb, g/l |
76,1±7,1 |
75,5±6,6 |
75,5±6,6 |
75±7,2 |
75,3±7,1 |
75,8±7,2 |
75,5±7,2 |
75,3±7,1 |
75,5±6,9 |
|
Free haemoglobin level, FreeHb, g/l |
0,03±0,01 |
0,02±0,01 |
0,03±0,01 |
0,03±0,01 |
0,03±0,01 |
0,04±0,01 |
0,03±0,01 |
0,04±0,01 |
0,04±0,01 |
|
Bilirubin, ctBil, mmol/l |
7,5±1,1 |
7,3±1,2 |
7,8±0,9 |
6,1±0,9 |
8,0±1,1 |
8,1±1,1 |
6,8±0,9 |
8,5±1,1 |
8,6±0,9 |
|
Lactate, cLac, mmol/l |
1,6±0,2 |
1,6±0,2 |
1,6±0,2 |
1,5±0,2 |
1,5±0,2 |
1,9±0,2 |
1,9±0,3 |
2,0±0,2 |
2,0±0,1 |
|
Potassium, К+, mmol/l |
2,1±0,3 |
2,0±0,3 |
2,0±0,3 |
2,2±0,3 |
2,6±0,1 |
3,0±0,4 |
3,3±0,1 |
3,9±0,1* |
4,2±0,1* |
|
Sodium, Na+, mmol/l |
149,8±0,8 |
149,5±0,6 |
149,3±0,8 |
149,1±0,6 |
149,1±0,6 |
149,8±0,4 |
150,8±1,4 |
151±1,4 |
150,8±1,4 |
|
Chlorine, Cl–, mmol/l |
116,1±2,9 |
116,1±2,5 |
116,5±2,5 |
116,3±2,5 |
117±2,7 |
116,6±2,7 |
116,5±2,9 |
116,1±2,7 |
116,1±1,1 |
|
рН |
7±0,01 |
7±0,03 |
7±0,01 |
7±0,02 |
7±0,01 |
7±0,01 |
7±0,02 |
7±0,02 |
7±0,02 |
Table 1 Blood system parameters obtained during the study of the circulatory assist disk pump left ventricular bypass on the stand
* - significant differences from the 0 sample to the connection.
In bench experiments, it was found that a trend towards a gradual increase in the level of FreeHb in the plasma of donor blood began after two hours of pump operation (Fig. 3), although these changes were unreliable. This increase could be due to partial hemolysis of red blood cells. Parallel to the FreeHb’s increasing trend, there was a slight increase in ctBil concentration from 7.8±0.9 to 8.6±0.9 mmol/l and cLac from 1.9±0.2 to 2.0±0.2 mmol/l, respectively. The concentration of Na+, Ca+2, Cl– did not change throughout the experiment, and the concentration of K+ increased from the 210th, but within the reference values, probably as a result of partial destruction of erythrocytes.
The mean NIH value in the six experiments was 0.0018, the mean MIH value 2.18. We did not find reference values of NIH and MIH in the available literature. In the study by O.Y. Dmitrieva et al. NIH was 0.0057, MIH was 0.5738, which was considered normal.12 According to K Bourque et al.,15 MIH was 2.1, 3.5 and 2.3, which was also considered normal.15 The NIH value in the analysis of T. Nakazawa et al. was 0.0028.16
Based on these findings, the NIH reference range is likely to be 0.0028 to 0.00574; for MIH – from 0.57388 to 3.5. Our NIH and MIH data were within the reported values.
Blood parameters obtained from animal experiments are presented in Table 2.
|
Indicator name |
Before connection |
Observation period, days |
Reference values |
||||||
|
1 |
2 |
3 |
4 |
5 |
6 |
7 |
|||
|
Blood pressure, mm Hg. Art. |
85±0,3 |
91±2,4 |
93,6±1,3* |
94±2,4* |
92,6±2,4* |
88,6±0,3* |
85,6±2,0 |
86,3±2,4 |
70–90 |
|
HR, beats/min |
80±0,2 |
87,6±4,1 |
90,3±3,7* |
93,6±2,7* |
95±3,1* |
94,3±2,4* |
94±2,4* |
96,3±0,6* |
70–100 |
|
SpO2, % |
98±0,1 |
96,3±0,6 |
95,3±0,3* |
96,3±0,3 |
96,6±0,3 |
97,6±0,3 |
97,6±0,3 |
97,6±0,3 |
96–100 |
|
Haematocrit, |
43,3±0,6 |
37±1,5* |
37,4±0,3* |
39,8±1,7 |
40,8±1,0 |
40,9±1,0 |
41,9±1,0 |
42,3±1 |
35–45 |
|
Hct, % |
|||||||||
|
Hemoglobin, |
93±4,1 |
76,3±0,3* |
77,0±0,6* |
78,6±2,0* |
80,3±2,4 |
80±1,7 |
81±1,7 |
82,3±2,4 |
91–130 |
|
ctHb, g/l |
|||||||||
|
red blood cells, |
4,4±0,5 |
4,1±0,1 |
4,1±0,07 |
4,1±0,1 |
4,4±0,2 |
4,5±0,1 |
4,4±0,1 |
4,4±0,03 |
5–7,5 |
|
1012/l |
|||||||||
|
Platelets, 109/l |
449,0±2 |
449,3±1 |
449,0±0,6 |
454,6±7,5 |
457,3±5,5 |
461,3±8,9 |
467,3±10 |
466,3±9,6 |
260–500 |
|
Leukocytes, 1012/l |
5,9±0,4 |
6,4±0,9 |
7,3±0,8 |
7,7±0,7* |
7,3±0,5 |
7,5±0,7 |
7,4±0,3* |
7,6±0,3* |
4,5–12 |
|
pH |
7,4±0 |
7,3±0,01 |
7,3±0,3 |
7,4±0,3 |
7,4±0,03 |
7,4±0 |
7,4±0 |
7,4±0,01 |
7,4 |
|
Standard excess of bases, |
–3,8±0,2 |
–2,9±0,2 |
–4,1±0,2 |
–3,9±0,2 |
–4,2±0,3 |
–4,1±0,2 |
–3,9±0,2 |
–3,8±0,1 |
0–5.33 |
|
cBase (Ecf), mmol/l |
|||||||||
|
Free hemoglobin level, |
0,01±0 |
0,05±0 |
0,05±0,1 |
0,04±0,1 |
0,03±0,1 |
0,03±0,1 |
0,04±0,1 |
0,04±0,1 |
0 |
|
FreeHb, g/l |
|||||||||
|
Bilirubin, |
10,1±0,2 |
11,9±0,4 |
11,8±0,4 |
11,6±0,5 |
11,5±0,5 |
10,9±0,3 |
10,5±0,07 |
10,4±0,07 |
6,5–18,3 |
|
ctBil, mmol/l |
|||||||||
|
cLac, mmol/l |
4,1±1,3 |
3,3±0,5 |
5,1±0,8 |
5,9±1,6 |
5,4±1,5 |
4,5±0,3 |
4,6±1 |
4,4±1,1 |
0,5–2,2 |
|
LDH, units/l |
148±0,9 |
150±1,3 |
158,3±5,1 |
156±4,1 |
167,3±2,4* |
170,3±0,3* |
173,3±1,7* |
176±0,6* |
90–180 |
|
Potassium, К+, mmol/l |
3,7±1,0 |
4,5±0,9 |
4,3±0,9 |
4,2±0,8 |
4,5±2,4 |
4,8±0,8 |
4,9±0,9 |
4,9±0,9 |
3,8–5,9 |
|
Sodium, Na+, mmol/l |
140,8±1,3 |
147±2,4 |
149±3,1 |
147,3±1,7 |
145,3±2,4 |
146,6±2,4 |
146,3±1,7 |
147,6±2,4 |
141,3–145,7 |
|
Chlorine, Cl–, mmol/l |
105,0±0,8 |
121,6±0,3* |
114,6±2,1* |
113,4±1,2* |
116,5±4,6 |
115,4±4,0 |
115,1±3,6 |
114,8±3,6 |
98–106 |
Table 2 Indicators of the blood system obtained during the study of a disc-type auxiliary circulatory pump left ventricular bypass on calves during 7 days of observation
* - significant differences from the 0 sample to the connection.
In animal studies, an increase in FreeHb ranging from 0.01±0 g/L to 0.05±0.1 g/L was observed on days 1–2 of the experiment. Further, from the 3rd day until the end of observation, fluctuations in free hemoglobin in the blood were in the range of 0.03–0.04 g/l and did not differ significantly from the background. During the same period (days 1–3), there was a significant decrease in hematocrit, which by the 4th day was almost restored to background values.
The majority of other studied biochemical and electrolyte parameters in the dynamics of observation did not change significantly in comparison with background values, and only on days 1-3 there was a tendency to their slight increase in comparison with the background level. However, BPcr and HR throughout the whole experiment were significantly higher than before the connection of the pump, the productivity of which is presented in Table 3. Figure 6 shows the dynamics of FreeHb g/l during the experiment on animals.
|
Rotor speed, rpm |
Flow rate, l/min |
Pressure, mmHg Art. |
||
|
at the entrance |
at the output |
difference |
||
|
1500 |
2,5 |
–1 |
48 |
49 |
|
2000 |
3 |
–7 |
79 |
86 |
|
2500 |
3,5 |
–9 |
113 |
122 |
|
3000 |
4 |
–11 |
136 |
147 |
Table 3 Performance of the MPC disc pump at different rotor speeds in the in vitro experiment
After connecting the pump, the greatest deviation of indicators from the norm was observed in the period of 1-3 days of the experiment. Thus, during this period some increase in concentration of cations, anions, bilirubin, lactate, LDH was observed. Further, most of the indicators returned to background values. It is important to note that practically all studied blood parameters throughout the experiment were within the reference values, except for hemoglobin content and erythrocyte count, which were lower than these values, and the concentration of lactate and chlorine in the blood exceeded the normal values.
Erythrocyte membrane damage is influenced by the threshold potential at which the erythrocyte membrane is destroyed and the exposure time. The shear stress threshold potential in blood flow is considered to be at 43 Pa, beyond which the erythrocyte membrane is destroyed. In a study by G. Wright states that erythrocytes are very resistant to many forces except shear stress.17 Based on the above, we can conclude that in in vivo experiments intravascular hemolysis was present, but in small quantities. Table 2 shows that, judging by the hemoglobin content and the number of red blood cells, the greatest increase in hemolysis was probably observed on days 1–2 of the experiment. On the 1st day of the experiment, this rate of hemolysis could be associated with the surgical intervention performed during pump implantation.
Erythrocyte membrane damage is also influenced by the time of exposure to the physical factor. In the studies of Ravichandran A.K. out of 100 patients with implanted pump, 18 had hemolysis, increased LDH and bilirubin content, which was accompanied by a significant increase in mortality one year after implantation.18 It is likely that the study of bilirubin and LDH using MIC pumps in in vivo experiments requires a longer observation period of 15–30 days. The collected data allow us to conclude that during short-term use the disc pump of auxiliary circulation at lower rotor speed (from 1500 to 3000 rpm) provided sufficient blood flow volume (up to 8 l/min) and had no significant effect on the red blood system, which allows its use in short-term extracorporeal connections.
The developed prototype of a disc-type mechanical circulatory support device for left ventricular bypass does not cause significant hemolytic, electrolyte and acid-base disturbances in the blood during 240 minutes of operation on a stand (in vitro) and 7 days in an in vivo experiment, which allows it to be recommended for short-term replacement heart as a “bridge” to organ transplantation or its unloading.
None.
The author declares there is no conflict of interest.

©2024 Golovina, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.