MOJ
eISSN: 2471-139X


Research Article Volume 3 Issue 2
1Department of Physiology and Developmental Biology, Brigham Young University, USA
2Department of Pathology and Laboratory Medicine, David Geffen School of Medicine at UCLA, USA
3Department of Neurobiology and Anatomy, University of Utah Medical School, USA
Correspondence: Jonathan J Wisco, Associate Professor, Department of Physiology and Developmental Biology, Neuroscience Center, Laboratory for Translational Anatomy of Degenerative Diseases and Developmental Disorders (TAD4), Brigham Young University, 4005 LSB, Provo, Utah 846025255, USA, Tel 310746-6647, Fax 8014220004
Received: January 06, 2017 | Published: March 8, 2017
Citation: Ascanio J, Schmalz N, Anderson DC, et al. Shared distal insertion of the gluteus medius and piriformis muscles and implications for rehabilitation exercises. MOJ Anat Physiol. 2017;3(2):71–74. DOI: 10.15406/mojap.2017.03.00089
Motivation for this study was prompted by the discovery of bilateral shared tendinous insertion of the gluteus medius (GM) and piriformis (PM) muscles into the anterior trochanteric crest during routine dissection of the gluteal region of a 58-year -old male cadaver. We therefore asked, what is the frequency of GM and PM shared insertions into the greater trochanter, and how could this impact physical therapy interventions for piriformis syndrome? In 23 specimens from either side of 16 embalmed human cadavers, we dissected and characterized the detail of GM and PM insertions. We discovered that just over 50% of the specimens dissected exhibited shared tendinous insertions between the two muscles, and in one specimen, we observed additional fusion of fibers of the superior gemellus (SG) and obturator internus (OI) muscles into the PM. The distal attachments of the GM and PM are more complex than traditionally understood and should be considered when prescribing rehabilitation exercises to treat piriformis syndrome.
Keywords: gluteus medius, piriformis, rehabilitation exercises, piriformis syndrome
GM, gluteus medius; PM, piriformis; OI, obturator internus; SG, superior gemellus; MRI, magnetic resonance imaging
The gluteus medius (GM) and piriformis (PM) muscles lie deep to the gluteus maximus and are important for their involvement in hip mobility and stabilization. As conventionally understood, the GM proximal insertion is on the external iliac surface below the iliac crest and between the anterior and posterior gluteal line spanning from the anterior superior iliac spine to the posterior superior iliac spine, and its distal insertion is on the lateral surface of the greater trochanter. The PM proximal insertion is on pelvic surface of the sacrum, and its distal insertion is on the on the apex of the greater trochanter.1
There are a number of reports of GM and PM anatomical variations.2‒4 Flack and colleagues2,3 recently performed a thorough review and analysis of the GM proximal and distal insertions. In their meta-analysis, the distal insertion of the GM was quite varied, extending from the anterolateral, to postero-superior surfaces of the greater trochanter. They included insertions into the posterior surface of the greater trochanter in their own analysis. Another study by Windisch et al.4 reported variations of the PM muscle insertions to the greater trochanter.
This study adds a new observation of GM and PM distal insertions, and maps the muscular and tendinous fiber insertions in 3D from a representative specimen. We discuss the implications toward prescribing rehabilitation exercises to patients experiencing pain related to piriformis syndrome.
During routine bilateral dissection of the gluteal region of a 58year-old male cadaver at Brigham Young University (BYU), we observed an unusual fusion of the distal tendon fibers of the GM into the PM bilaterally where it inserted on the anterior crest of the greater trochanter between each muscle’s respective classical insertion. We also observed insertions of the superior gemellus (SG) and obturator internus (OI) muscles into the PM tendon.
Following routine bilateral dissection of the formalin embalmed 58-year-old male cadaver hips, and the observation of GM and PM tendon fibers fusing into a common insertion bilaterally, we used a MicroScribe 3D digitizer to create a 3D map the fibers of both muscles Figure 1 shows only right side. The MicroScribe tool stylus plots user traced points in a 3DCartesian coordinate system. The three anatomical reference points were used for the digitization space using drilled-in Phillip stainless steel screws:
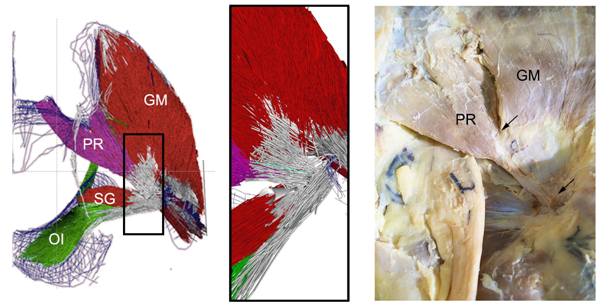
Figure 1(Left) Posterior view of 3D MicroScribe map of hip rotators in posterior hip. The map demonstrates the shared tendinous insertion between the GM and PM muscles. Magnified image demonstrates tendinous fibers sharing distal insertion of the PM and GM. The obturator internus (OI) and superior gemellus (SG) also share a tendinous insertion, but only on the right side. (Right) Dissected specimen demonstrating shared tendinous insertion. Notice the tendon of the PM joining the tendon of the GM.
In order to guarantee accurate readings using MicroScribe 3D digitizer, the area to be digitized was secured. Two methods were used to stabilize the hip during the MicroScribe process.
The first method consisted of using two ¼” bolts secured through the superior ramus of the pubis and body of the sacrum onto a ½” x 3’ x 2’ particle board to stabilize access to the main body of the GM. The second method involved using two cam buckle tie downs on 2’ x 4’ boards to secure the hip at different angles to reach the PM. The particle board was secured to a table using two bar clamps for added stabilization.
Layers of digitally traced muscle and tendon fibers are peeled back in approximately 1 mm thickness to reveal deeper layers, which are also subsequently digitized. The entire volume of muscle and tendon fibers are digitized into a wireframe model and then reconstructed in Autodesk Maya into rendered tubes. Additional deep hip rotators such as the SG, and OI were also digitized.
In addition to mapping the primary specimen using MicroScribe 3D, we dissected 21 posterior hip regions from opportunity specimens from the David Geffen School of Medicine at the University of California Los Angeles (UCLA) to determine the anatomic variability of GM and PM distal insertions. Table 1 summarizes results for all 23 dissections, including the two original specimens from BYU. After dissections were completed, the attachments of the GM and PM muscles were organized into major categories of insertion:
Subject |
Gender |
Side |
GM Tendon Insertion into Lateral Greater Trochanter |
PM Tendon Insertion into Apex of Greater Trochanter |
Common Tendinous Insertion of GM and PM Tendons into Anterior Trochanteric Crest |
1 |
M |
R |
X |
||
L |
X |
||||
2 |
M |
R |
X |
X |
|
L not dissected |
|||||
3 |
M |
R |
X |
||
L |
X |
X |
|||
4 |
F |
R |
X |
X |
|
L |
X |
X |
|||
5 |
F |
R |
X |
X |
|
L not dissected |
|||||
6 |
M |
R destroyed |
|||
L |
X |
X |
|||
7 |
F |
R not dissected |
|||
L |
X |
X |
|||
8 |
M |
R |
X |
||
L hip replacement |
|||||
9 |
F |
R |
X |
X |
|
L not dissected |
|||||
10 |
M |
R |
X |
||
L not dissected |
|||||
11 |
M |
R |
X |
X |
|
L |
X |
X |
|||
12 |
F |
R |
X |
||
L |
X |
||||
13 |
M |
R |
X |
||
L |
X |
||||
14 |
M |
R |
X |
X |
|
L not dissected |
|||||
15 |
F |
R not dissected |
|||
L |
X |
||||
16 |
M |
R |
X |
||
L |
X |
Table 1 Hip dissections demonstrating the various Insertions of the gluteus medius (GM) and piriformis (PM) from opportunity specimens at BYU and UCLA. Note that shared insertion of the GM and PM muscles was present in just more than 50 percent of the specimens dissected
M: Male; F: Female; R: Right; L: Left; X: Present; GM: Gluteus Medius; PM: Piriformis
The MicroScribe 3D mapping of the 58-year-old male cadaver hip specimen on both sides only right side shown in Figure 1 demonstrated that the GM muscle is arranged in fascicles that insert into a deep aponeurotic tendon, has proximal insertions along the entire iliac crest, and shares a common distal insertion with the PM. Specifically, the GM insertion curves superiorly across the greater trochanter to the posterolateral portion via a shared aponeurosis with the PM. We noticed GM fiber bundles (2-3mm) inserting into the belly of the PM near the superior gluteal artery. Similar results were apparent on the left side of the specimen. Furthermore, the OI and SG shared tendinous distal insertions with the PM, but only on the right side (Figure 1).
As Table 1 depicts, out of the 32 specimens available at UCLA, we had access to 23 for observations. We noted that just more than 50%(12/23) specimens also shared GM and PM tendons on the posterolateral surface. Of the cadavers from which both sides were available for observation, all exhibited either conventional anatomy or the shared tendon bilaterally, with the exception of one cadaver (Table 1).
We suspect that variations in the insertion of the GM and PM occurs during fetal development due to drastic natural changes in the topography of the pelvis and femur as it develops. Naito et al.5 elegantly described the development of the inferior gemellus, SG, OI, SG, PM, and the GM in 26 human embryos. In particular, embryos at 15-weeks-gestation exhibit definitive joining of the PM tendon with the OI tendon and GM tendon while the PM tendon is still migrating to its eventual final attachment site. Once the PM tendon finds its attachment, the GM and OI “release” the PM tendon. Our observations in this study corroborate Naito and colleague’s results and demonstrate that the release of the PM tendon only occurs in about 50 percent of the population.
Piriformis syndrome is a rare neuromuscular disorder that occurs when the sciatic nerve is compressed or otherwise irritated by the PM muscle causing pain, tingling, and numbness. It is often diagnosed using the flexion, adduction and internal rotation (FAIR) test (measures sciatic nerve conduction) and Magnetic Resonance Imaging (MRI; highlights inflammation of the nerves themselves). Although surgery is an option to treat piriformis syndrome, there are occasions when the surgery will not fully solve the problem. Two studies demonstrated that surgery to release PM can lead to continued PM syndrome after release and at times a second surgery needs to be performed.6,7
An alternative method to treat PM syndrome is physical therapy. One study found that strengthening the hip abductors, extensors, and external rotators, as well as movement re-education through physical therapy provided pain relief to the patient.8 Another study focused on providing patients with pain radiating down the leg with a specific stretching program and these patients found great pain relief after four weeks of therapy. Although the likely cause of pain radiating down the leg could be from PM syndrome, these stretching exercises focused on stretching the OI muscle.9
The joint tendinous insertion of the GM and PM and the variation of insertion in just more than 50 percent of the specimens we examined provide additional evidence for a physical therapist to include exercises that involve the GM and surrounding hip musculature to treat PM syndrome. It is vital to include exercises that provide full range of motion including extension, flexion, abduction, adduction, external rotation and internal rotation exercises to treat PM syndrome. Given our findings that the GM and PM can share a tendon on the trochanteric crest, releasing the GM may also help release the PM, therefore reducing pain associated with piriformis syndrome. Future studies are required to determine if this is indeed the case.
The authors wish to thank individuals who donated their bodies and tissues for the advancement of education and research. The authors also acknowledge the generosity of financial donors who contributed to the Brigham Young University Office of Research and Creative Activities (ORCA) Mentoring Environment Grant and Student Research Grant that funded this project.
The authors declare that they have no conflict of interest. This study analyzed cadaveric specimens, which are considered non-human and non-animal subjects.

©2017 Ascanio, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
This is a modal window.