MOJ
eISSN: 2471-139X


Research Article Volume 4 Issue 4
1Laboratory of Anatomy and Organogenesis, Gaston Berger University, Senegal
2General Surgery Service, Regional Hospital, Senegal
3Laboratory of Anatomy, University of Lille 2, France
4Musculoskeletal Imaging Service, CHRU de Lille, France
5Laboratory of Anatomy and Organogenesis, Cheikh Anta Diop University, Senegal
Correspondence: Philippe Manyacka MA Nyemb, Laboratory of Anatomy and Organogenesis, UFR 2S, Gaston Berger University, Road of Ngallelle, 234 Saint-Louis, Senegal, Tel (+221) 77 445 43 13
Received: October 26, 2017 | Published: November 21, 2017
Citation: Nyemb PMMA, Fontaine C, Demondion X, et al. Morphological anatomy of the trapezius muscle, about 58 dissections: what to know before harvesting the muscular flap. MOJ Anat Physiol. 2017;4(4):348–353. DOI: 10.15406/mojap.2017.04.00145
Introduction: The musculocutaneous flaps of the trapezius muscle are interesting options in head and neck reconstruction surgery. However, these flaps are based on a very variable vascularization of the trapezius. The purpose of this paper is to review the basics of the trapezius muscle morphology and vascular anatomy, through a series of dissections.
Materials and methods: Fifty-eight anatomical regions were dissected. For each dissection the perforating arteries of the trapezius muscle have been identified and the morphological anatomy of the muscle has been studied.
Results: In all our dissections, the trapezius muscle parts presented as described in the literature: a descending cranial part, a transverse middle part, and an ascending caudal part. On the surface corresponding to trapezius muscle, an average of 15 perforators arteries were found on each side of the line of spinous processes.
Conclusion: Each of the trapezius muscle parts can serve as a basis for harvesting a muscular or musculocutaneous flap. However, variations in the vascular anatomy of each part must be taken into account.
Keywords: trapezius, part, muscular flap, vascularization, anatomical variation
The trapezius muscle is divided into 3 main parts: the cranial or descending portion, the lateral (middle) or transverse portion, and the caudal or ascending portion.1,2 Each of these parts has its own vascularization. The descending portion is irrigated by branches of the occipital artery, the transverse portion receives branches of the superficial cervical artery, and the ascending portion is essentially irrigated by the dorsal scapular artery and its branches.3,4 However these arteries represent only the main pedicles, moreover they anastomose widely between them. The arterial vessels of the trapezius muscle are therefore very variable. The authors of the present article remind that before proceeding to a muscular flap harvest of the trapezius, it is essential to review bases of the morphological and vascular anatomy of this muscle.
The trapezius muscle originates on the occipital bone, nuchal ligament, spinous process of the 7th cervical vertebra (C7) and all of the thoracic vertebrae. It has three parts. The superior portion (descending fibers) terminates on the posterior margin and superior side of the lateral third of the clavicle. The transverse portion (middle fibers) terminates on the medial margin of the acromion and superior lip of the posterior border of the scapular spine. The inferior portion (ascending fibers) ends as an aponeurosis on the posterior edge of the scapular spine and a tubercle. The trapezius muscle is innervated by the accessory nerve and the cervical plexus. It helps to move the head (extension and rotation) and the shoulders (shrugging, lowering, posterior tipping, bringing the scapulae closer together).
According to the Mathes & Nahai5 the trapezius muscle receives type II vascularization with a primary pedicle from the transverse cervical artery and secondary pedicles issued from the occipital, intercostal and circumflex scapular perforating arteries.
The transverse cervical artery has a somewhat variable territory. However, its branches anastomose to those of the dorsal scapular artery to contribute to the vascularization of the trapezius, both in the muscle body itself and its integuments. Based on an anatomical study of 124 cadavers,6 the descending fibers receive branches from the occipital artery; the middle fibers and the lateral areas receive branches from the superficial branch of the transverse cervical artery; the ascending fibers receive branches from the dorsal scapular artery and the posterior intercostal arteries. Nevertheless, these vessels vastly anastomose with each other.
The occipital artery courses under the cranial portion of the trapezius muscle; some of its branches perforate the muscle layer to terminate in the integuments. The occipital artery has two terminal branches: a large medial branch that splits in the body of the trapezius muscle and anastomoses with the deep cervical artery and dorsal scapular artery, and a smaller, inconsistent lateral branch.3,4 At the nape of the neck, there are typically only two arterial trunks: a branch of the occipital artery and a branch of the deep cervical artery. The dermis and hypodermis networks are very dense in this area. The nape's skin has a reduced number of large arterial trunks but numerous arterioles.3
The dorsal region is mainly irrigated by the posterior intercostal arteries and dorsal scapular artery. Before entering the intercostal space, the posterior intercostal arteries give off a dorsal branch. The latter immediately courses posteriorly; once over the intervertebral foramen, it bifurcates into a spinal branch and a musculocutaneous branch. The musculocutaneous branch heads into the inter transverse space and then splits into a lateral muscular branch and a medial musculocutaneous branch. In the skin layer covering the vertebral grooves and the caudal portion of the trapezius muscle, there are two types of cutaneous arteries: posteromedial perforating arteries that stem from the medial branch of the musculocutaneous branch of the dorsal branch and posterolateral perforating arteries that stem from the lateral branch of this same branch.3,4
The superior cervical artery courses laterally to the levator scapulae muscle and the rhomboid muscles, before going medially to give off a (short) ascending branch and a (long) descending branch that pass next to the scapular spine. Its descending trajectory is superficial to the levator scapulae and rhomboid muscles, and next to a few branches of the external branch of the accessory nerve. At this level, its diameter is generally greater than 0.7mm.7
The dorsal scapular artery courses deep to the levator scapulae and rhomboid muscles. Branches then pierce the fascia separating the two rhomboid muscles (major and minor) and become superficial over the medial margin of the scapula. They form the dorsal scapular artery. This superficial branch penetrates the deep side of the trapezius and then gives off several cutaneous perforators that irrigate the skin covering the caudal portion of the trapezius-here it courses 1 to 2cm from the muscle's lateral margin. The average diameter of the dorsal scapular artery is 2.7mm proximally and at its origin, and 1.95mm over the levator scapulae muscle.7 A deep branch of the dorsal scapular artery continues its descending trajectory under the rhomboid major muscle. This descending branch gives off several perforators to the rhomboid muscles, trapezius muscle and the overlying skin.8
Dissection was performed in 58 anatomical regions from 32 non-formalin fixed cadavers. The average age of the donors was 72.32 years (range, 34-90) and there were 21 males and 11 females. The cadavers had no history of surgery or deformity in the areas targeted for dissection (supraclavicular and dorsal regions). They were embalmed using a glycerin-rich, formalin-free solution to preserve tissue suppleness.
For the first stage, the cadaver was placed in dorsal decubitus and the posterior triangle (lateral cervical region) was approached to remove the clavicle. The subclavian artery and its collateral arteries were dissected, identified and marked (Figure 1). The collateral branches of the subclavian artery responsible for trapezius vascularization were injected with a solution containing a mixture of gelatin, methylene blue and iron powder. The cadaver was then refrozen for 24 hours.
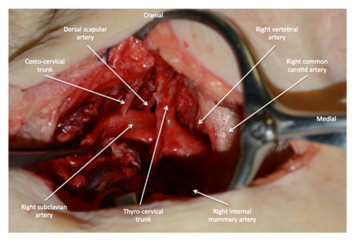
Figure 1 Dissection of collateral branches of the subclavian artery at the lateral triangle of the neck.
In the second stage, the cadaver was thawed out at room temperature and then placed in ventral decubitus to dissect a perforator flap from the trapezius. For this dissection, a superficial incision was made on the lateral, caudal and cranial margins of the trapezius muscle, making sure not to penetrate the muscle layer (Figure 2). The superficial layer was separated from the muscle's surface and detached from caudal to cranial and from lateral to midline (Figure 3 & 4). During this procedure, the perforators were dissected and inventoried. Dissection of the largest perforators was then continued through the muscle while preserving the integrity of the surrounding muscles (trapezius, rhomboids, levator scapulae). The superficial layer (perforator flap) was then harvested in its entirety (Figure 5).
In all our dissections, the trapezius muscle portions presented themselves as described in the literature: a descending cranial portion, a transverse middle portion, and an ascending caudal portion. However, there were some anatomical variations on the insertions of origins of the cranial and caudal portions.
On the corresponding surface of the trapezius muscle, 15 perforators (range, 5-27) on average were found on each side of the spinous process line. The average diameter of these perforators was 0.58 mm (range, 0.1-2.6). The average dimensions of the perforasome were 6.6 x 7.06 cm, corresponding to a mean area of 36.6 cm2 (range, 20-90). The transmuscular pedicle had an average length of 12.13 cm (range, 5-19). More than 80% of the perforators that we found were musculocutaneous. Starting from the pivot point, a 180° arc of rotation was achieved; the average distance separating the pivot point from the spinous process line was 6.2 cm (range, 4-12 cm). More detailed findings are given in Table 1.
Specimen Number by Order of Dissection |
Age |
Sex |
Number of Perforators Found |
Average Diameter (mm) |
Size of Perforasome (cm) |
Length of Pedicle after Transmuscular Dissection (cm) |
Arc of Rotation From Pivot Point (°) |
1 |
67 |
F |
13 |
0.8 |
6 x 7 |
19 |
180 |
2 |
88 |
H |
10 |
0.4 |
9 x 6 |
14 |
180 |
3 |
89 |
H |
15 |
0.4 |
5 x 7 |
16 |
180 |
4 |
90 |
F |
9 |
0.8 |
4 x 8 |
10 |
180 |
5 |
75 |
F |
17 |
0.2 |
5 x 7 |
13 |
180 |
6 |
57 |
H |
14 |
1.2 |
10 x 9 |
11 |
180 |
7 |
59 |
H |
18 |
0.4 |
8 x 5 |
9 |
180 |
8 |
62 |
H |
15 |
0.4 |
8 x 5 |
16 |
180 |
9 |
69 |
F |
16 |
0.1 |
6 x 5 |
7 |
180 |
10 |
65 |
H |
9 |
0.4 |
6 x 6 |
11 |
180 |
11 |
78 |
H |
17 |
0.8 |
8 x 5 |
10 |
180 |
12 |
73 |
H |
18 |
0.4 |
6 x 6 |
16 |
180 |
13 |
72 |
H |
18 |
0.3 |
8 x 5 |
12 |
180 |
14 |
88 |
F |
17 |
0.8 |
6 x 8 |
16 |
180 |
15 |
63 |
H |
23 |
0.5 |
8 x 7 |
10 |
180 |
16 |
72 |
H |
5 |
0.4 |
8 x 5 |
15 |
180 |
17 |
77 |
F |
15 |
0.5 |
8 x 5 |
10 |
180 |
18 |
58 |
F |
16 |
0.4 |
7 x 6 |
14 |
180 |
19 |
87 |
F |
16 |
0.4 |
8 x 8 |
13 |
180 |
20 |
63 |
H |
15 |
0.8 |
7 x 7 |
16 |
180 |
21 |
64 |
H |
17 |
1.9 |
6 x 6 |
8 |
180 |
22 |
74 |
H |
20 |
0.4 |
6 x 8 |
11 |
180 |
23 |
65 |
H |
15 |
0.3 |
8 x 7 |
10 |
180 |
24 |
75 |
F |
13 |
1.3 |
10 x 6 |
7 |
180 |
25 |
90 |
H |
13 |
0.4 |
5 x 7 |
11 |
180 |
26 |
72 |
F |
7 |
0.4 |
5 x 4 |
16 |
180 |
27 |
88 |
F |
17 |
0.8 |
5 x 8 |
13 |
180 |
28 |
69 |
H |
18 |
0.3 |
7 x 8 |
16 |
180 |
29 |
67 |
H |
15 |
0.3 |
5 x 6 |
16 |
180 |
30 |
78 |
H |
13 |
1.2 |
7 x 10 |
16 |
180 |
31 |
64 |
H |
9 |
0.8 |
6 x 8 |
12 |
180 |
32 |
75 |
H |
12 |
1.2 |
10 x 6 |
17 |
180 |
33 |
75 |
H |
8 |
0.3 |
8 x 6 |
10 |
180 |
34 |
63 |
F |
7 |
0.3 |
7 x 7 |
11 |
180 |
35 |
81 |
H |
11 |
0.4 |
6 x 5 |
19 |
180 |
36 |
78 |
H |
17 |
0.4 |
9 x 5 |
10 |
180 |
37 |
85 |
H |
15 |
0.5 |
6 x 8 |
10 |
180 |
38 |
85 |
H |
27 |
0.4 |
6 x 9 |
16 |
180 |
39 |
75 |
F |
15 |
0.9 |
6 x 10 |
9 |
180 |
40 |
81 |
H |
13 |
0.8 |
5 x 8 |
16 |
180 |
41 |
87 |
F |
20 |
0.8 |
6 x 10 |
14 |
180 |
42 |
67 |
F |
19 |
0.1 |
8 x 8 |
5 |
180 |
43 |
82 |
H |
16 |
0.9 |
6 x 10 |
16 |
180 |
44 |
85 |
H |
17 |
0.8 |
6 x 10 |
16 |
180 |
45 |
69 |
F |
13 |
1.4 |
5 x 8 |
9 |
180 |
46 |
77 |
F |
12 |
0.4 |
5 x 5 |
10 |
180 |
47 |
73 |
H |
17 |
0.4 |
7 x 9 |
4 |
180 |
48 |
80 |
H |
8 |
0.7 |
6 x 6 |
8 |
180 |
49 |
80 |
H |
18 |
0.3 |
7 x 6 |
10 |
180 |
50 |
79 |
H |
19 |
0.5 |
5 x 8 |
5 |
180 |
51 |
69 |
F |
23 |
0.5 |
5 x 8 |
19 |
180 |
52 |
34 |
H |
16 |
0.4 |
6 x 5 |
7 |
180 |
53 |
34 |
H |
17 |
0.4 |
6 x 9 |
17 |
180 |
54 |
57 |
H |
12 |
0.8 |
6 x 7 |
8 |
180 |
55 |
61 |
F |
15 |
0.4 |
5 x 8 |
14 |
180 |
56 |
47 |
F |
15 |
0.7 |
6 x 7 |
10 |
180 |
57 |
77 |
H |
22 |
0.5 |
7 x 5 |
11 |
180 |
58 |
81 |
H |
13 |
0.5 |
6 x 8 |
9 |
180 |
Table 1 Summary of the findings in the 58 dissected specimens
In our work, there are important anatomical variations of the trapezius muscle with regard to its neurovascular pedicle in the subclavian region. The arterial vascular pedicle of the trapezius can invariably arise from the thyro-cervical trunk or the subclavian artery. Venous drainage is distributed between the external jugular vein and the subclavian vein. The accessory nerve contracts variable relationships with these vessels. Thus, the accessory nerve may pass superficially or deeply to the vascular pedicle. These reports thus make it possible to passively preserve the nerve during harvesting of the flap (when it passes superficially to the pedicle) or to sacrifice a vessel to preserve it (when it passes deeply to the pedicle). The variability in the description of the blood vessels of the trapezius muscle can also be explained by the confused nomenclature of the lateral triangle of the neck's arteries, and misinterpretations of the term "transverse artery of the neck". This confusion appears in several studies.9,10 Paradoxically, although there are important variations in the vascular sources of the trapezius muscle, the trapezius integuments have been studied from a vascular point of view. The precise vascular territory of the skin above the trapezius muscle is sufficiently well known, because of studies using selective angiograms and intra-arterial injections of E1 prostaglandins.11 According to our study, the skin irrigated by the musculocutaneous perforators of trapezius is larger than the muscular surface. For Cormack,12 this cutaneous perforasome can extend up to 10 cm outside the muscle, and measure up to 3 times the muscle area. The concept of musculocutaneous flaps is ancient, the earliest examples having been described a century ago.3,4 There are several types of musculocutaneous flaps of the trapezius muscle, because that muscle receives several arterial pedicles for its vascularization.
The muscular flaps of the cranial portion of the trapezius are less used than those of the other portions. However, one of the first musculocutaneous flaps described is cranially based on the occipital vessels.13 The anatomical dissections of these vessels show that they are small and inconstant, and that they irrigate the splenius muscle before entering the trapezius. This configuration suggests that splenius should be incorporated into the muscular part of the trapezius flap. Due to the small size of the occipital arterial branches, this flap presents a large pedicle consisting of several small arterial branches. Indeed, in our experience it would be technically difficult and risky to use a single occipital arterial pedicle. In addition, the amplitude of a musculocutaneous flap based on the occipital branches is limited to the cranial part of the neck, the parotid region and the mandibular region. It can therefore be used in the closure of oro-cutaneous and pharyngocutaneous fistulas. Although accessory nerve preservation is recommended, experience shows that leaving the nerve in place may reduce the amount of flap rotation.
Compared with the muscle flaps of the cranial portion of the trapezius muscle, those of the middle portion have the advantage of also providing bone tissue. The osteo-muscular flap of the trapezius is a pedicled flap that allows to collect the middle part of the muscle and the skin, as well as the spine of the scapula, all supplied by the transverse vessels of the neck.14 This flap was initially described by Demergasso et al.15 It differs from the pedicled flap of the lower trapezius, which uses the portion of the muscle below the spine of the scapula. This last flap cannot contain any bone, and its vascularization depends on the transverse artery of the neck and the dorsal scapularis artery. The arterial vasculature of the trapezius depends variably on the transverse artery of the neck for the middle part of the muscle including the spine of the scapula, on the deep branch of the transverse artery of the neck (or dorsal scapularartery) for the part located below the spine of the scapula, and on the posterior intercostal arteries for the upper part of the trapezius muscle. Variations in the path of the 2 main arteries of trapezius flaps (the transverse artery of the neck which runs deeply and gives branches for the middle part of the trapezius, and the dorsal scapularartery) have been studied by Huelke.16 The first description of the trapezius flap by Demergasso et al.15 had already exposed the particular difficulties of this technique: the removal of the bone which must respect the acromion, the anatomical variations of the venous drainage and the impossibility of taking the accessory nerve for thick flaps. Concerning this last point, Vacher et al.14 explains that it is not the volume of the flap but rather the relations of the nerve with the vessels which leads to the sacrifice of the accessory nerve. The venous drainage of the trapezius has been very little studied, as well as relationships of the vessels and the accessory nerve at the anterior edge of the trapezius muscle. This would explain why in Vacher's work14 it is impossible to preserve the accessory nerve in 33% of cases.
The musculocutaneous flap of the caudal portion of the trapezius muscle has many advantages. It provides a long arc of rotation that allows reaching the periorbital regions. It is thinner and more flexible than the musculocutaneous flaps of the dorsalis major and pectoralis major muscles.17 Its donor site can easily be closed. The preservation of the accessory nerve and of the cranial portion of the trapezius muscle minimizes functional consequences on the shoulder. Furthermore, the agreement between the appearance of the flap and that of the recipient sites is better than with free flaps. The main disadvantage of the musculocutaneous flap of the caudal part of the trapezius is its position. Putting the patient in lateral decubitus for flap harvesting may be an obstacle, particularly in the case of loss of substances located in the oral cavity or in the anterior cervical region.
The three musculocutaneous flaps of the trapezius remain interesting options in reconstruction surgery of the head and neck. However, the vertical muscular flap of the caudal portion of trapezius is better than the 2 others in terms of versatility, reliability and low morbidity.18 There are also several advantages of this flap compared to the musculocutaneous flap of the pectoralis major muscle. Because the lower trapezius flap has a finer vascular pedicle and can therefore be more malleable in terms of relief. In addition, the musculocutaneous flap of the caudal portion of the trapezius contains less subcutaneous tissue, so it is more flexible than the musculocutaneous flap of the pectoralis major muscle; which gives it an advantage for oropharyngeal losses of substances.19,20 Although it is true that the caudal part of the trapezius receives mainly its vascularization of the dorsal scapular artery, it also receives a lot of secondary pedicles (intercostal arteries and transverse artery of the neck). However, both systems anastomose extensively in muscle thickness. Moreover, the flap has a wide arc of rotation when the dorsal scapular pedicle is used, it is also more viable.19,20 This musculocutaneous flap of the lower trapezius makes it possible to treat deformities and losses of substances of the head and neck regions.
What seems obvious in our series of dissections is that the dorsal scapular artery represents the main source vessel of the caudal part of the trapezius muscle (and by extension of the middle part in some subjects). However, the origin and the route of this artery can be very variable. The practitioner must take into account this variability if he wants to use this artery to harvest a trapezius flap.
Our work shows that each portion of the trapezius muscle can serve as a basis for muscle flap harvesting, depending on the location, the size and depth of the loss of substance to be treated. Our work shows that to improve the results of surgery, the vascularization of the trapezius muscle (and its anatomical variations) must be taken into account, more than its morphological division.
In surgery, when harvesting the muscle flap from the cranial portion of the muscle trapezius, the incorporation of the splenius muscle and the dissection of a large vascular pedicle improve the functional outcomes, due to the particular configuration of the occipital arteries. For the same reason, the flap of the cranial portion of the trapezius muscle gives less good results than the others two. The accessory nerve can be incorporated for better mobilization, but there is a risk of functional sequelaes. The flap of the middle portion of the trapezius muscle is interesting because of its larger arterial pedicle brought about by the transverse artery of the neck, and because of its essential bone contribution in the repair of osteomuscular loss of substance. However dissection of the nerve more difficult and sometimes it has to be sacrificed. In the muscular flap of the caudal portion of the trapezius muscle, the dorsal scapular artery allows for greater flexibility and increased mobility. The anatomy of the dorsal scapular artery enables a wide arc of rotation and a satisfactory blood flow, even when reaching the furthest regions. The flap of the caudal portion of the trapezius muscle should be preferred over the others 2 when possible, because it is more viable.
None.

©2017 Nyemb, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.