MOJ
eISSN: 2471-139X


Research Article Volume 5 Issue 3
1Retired Professor, Department of Physiology, GMCH, Chandigarh, India
2Presently Professor, Department of Physiology, DR.VRK Women's Medical College, India
3Department of Physiology, GMCH, Chandigarh, India
Correspondence: Sri Nageswari K, Retired Professor, Department of Physiology, GMCH, 203B Block, Manjeera Heights Phase1, Chitra Layout, NTR Nagar, Hyderabad-500074, Telangana, India, Tel 91-9000744270
Received: March 28, 2018 | Published: May 8, 2018
Citation: Sri NK, Malhotra A, Kaur G, et al. Longitudinal studies to evaluate stress in first year medical students through cold pressor response and psychological variables. MOJ Anat & Physiol. 2018;5(3):170–176. DOI: 10.15406/mojap.2018.05.00185
Background: Medical education has been well documented to be stressful. Added on to this, the duration of First Professional MBBS has been reduced from 1½ years to 1 year, though the teaching curriculum remained the same. It was felt desirable to evaluate stress in First year medical students (n=46) through Physiological parameters (Blood Pressure Reactivity/Response to cold, CPR) and Psychological scales like General Health Questionnaire, Major Hassels, Minor Hassels, Quality of life and Coping Check List in a longitudinal study design. Based on the GHQ Scores and the Blood Pressure Reactivity to cold, the students (n=46) were classified initially, during Phase1 studies as severely stressed (Group I, n=16) moderately stressed (Group II, n=22) and normal (Group III, n=8). Considerable shifting among the groups occurred during Phase 2 studies, with the application of a known stressor i.e. examination stress. Majority of students (n=44, 96%) exhibited stress during the studies conducted at Phase 1 (initial) and/or Phase 2. Only two students remained stress free throughout. The data from the students of various groups were analyzed by inter and intra group comparisons through students’ t-test at 95% confidence level for any significance. As a follow up, 44 medical students of next batch were inducted into various relaxation training programs. Fifteen students were given yogic relaxation exercises for one hour daily in the evening for 6 weeks, 15 students were given Raj yoga meditation training(BK group) at Brahmakumari centre for one hour daily in the morning for 20 days and 14 students were not given any training (Control group). The yogic exercises were pranayam, yog nidra and shavasan. For the BK group, the students were given orientation program prior to training with Rajyoga relaxation/meditation techniques. Different faculty members accompanied each group in the morning or evening. The morning sessions used to start around 7.30am and evening sessions around 6pm. The results revealed significant coping with administered stress at phase2 in BK group while control group exhibited significant stress.
Keywords: longitudinal studies, cold pressor test (CPT) and response (CPR), general health questionnaire, examination stress, Phase 1 & Phase 2, follow up studies, Brahmakumari’s Raj Yoga meditation, yogic relaxation exercises
It is well known that stress and anxiety impair cognitive performance. Stress related anxiety disorders and depression have been reported in undergraduate medical students during the time course of medical education. If the vulnerable students are picked up and diagnosed in the early stages of stress by subjecting them to various physiological and psychological tests, development of stress related anxiety disorders, depression and other psychosomatic illnesses at a later stage could be averted. The study was initiated with these aims and objectives. Medical students comprise a homogenous set of population with similar ethnic, socio-economic background and similar age group. Students who were diagnosed to be suffering from depression, anxiety disorders or undergoing medication for any psychiatric illness were excluded from the study and referred to the Psychiatry department of Government medical college, Chandigarh. Not all the students respond to medical education with the development of stress symptoms and the studies employing variables that are correlates of stress might not prospectively identify the vulnerable students. Stewart et al.1 investigated depression and anxiety in Ist year medical students in a longitudinal study with a gap of eight months between wave one and wave two. However, many of the reported studies are cross sectional. Hence, it was felt desirable to evaluate stress in first year medical students through physiological and psychological variables during longitudinal studies conducted in two phases which are beneficial over cross sectional studies and follow up studies after giving relaxation training to the next batch of students.
There is consensus as to the fact that medical school training is very stressful.2 The environment of medical school appears to be significant contributing factor for development of stress in students.
One can speculate the possible stress factors during the first professional MBBS as1 reduction in the duration of Ist Professional MBBS from 1½ years to one year though the teaching curriculum remained the same, which led to more course work2 Sudden transition of the students from school to professional college and cut throat competition.3 More disciplined life, busy schedules, more course load at medical college as compared to the college life.
The evaluated stress indicators were physiological parameters measured through cold induced blood pressure reactivity (Cold Pressor Response, CPR), which is an index of vasoconstrictor tone and hence an indicator of stress. Psychological scales like General Health Questionnaire, Major Hassles, Minor Hassles, Quality of life and Coping Check List were also applied.
The study design employed to evaluate stress was conducted in two phases and same study design for follow up group. All the admissions of the undergraduate medical students were completed by the end of September. Hence the Phase I studies started in the month of November after the students got adapted to the medical education system for four weeks. Phase 2 studies were conducted before the send up examination (a known stressor) in the month of March next year. The medical students of next batch were administered relaxation exercises. It was felt desirable to avert development of cumulative stress related to course load by training the students for undergoing relaxation through yoga / Brahmkumari’ rajyoga meditation practices.
Hines et al.3 reported a simple procedure where-in thermo-sensory stimulation with cold applied locally (Cold Pressor Test, CPT) produced strong vasopressor response in 99% of all subjects with remarkable consistency over period of time. The response is characteristic for the individual and remains so throughout life. The experimental procedure adopted by us is as per the methodology of Hines et al.3 The students were explained the procedure and written consent was obtained from students for all the experimental procedures conducted as per Helsinki guidelines.
The Physiological parameters that were recorded by us were baseline heart rate, diastolic and systolic blood pressure and diastolic and systolic blood pressure during cold pressor test. The subject is allowed to rest in a quiet room for 20-60 minutes. Several readings of blood pressure are taken until a basal level is reached. The cuff of the sphygmomanometer is placed on one arm of subject and the opposite hand is placed in cold water (4○C) to a point just above the wrist. Readings of the blood pressure are taken at the end of 30 seconds & 1 minute and after taking out the hand, every minute, till the value returned to baseline (recovery time, RT). The range/response i.e. the increase in blood pressure from the base line value was taken as DSBP/DDBP and the time duration of return of the blood pressure value to the baseline was taken as recovery time (RT). Blood pressure reactivity or cold pressor response (CPR) is an index of vasoconstrictor tone and an indicator of stress. Murray et al.4 indicated that vascular hyper reactivity (rise in blood pressure of 20/20 mm Hg or more) to the cold stimulus occurred regularly in hypertensives. They observed that the normo-tensive hyper reactors developed hypertension later in life.
Psychological parameters like General Health Questionnaire (GHQ),5 Quality of life (QOL, scale modified in Hindi by AIIMS),6 Coping Check List (CCL),7 Minor Hassles8 and Major Hassles9 were tested through questionnaire to evaluate the degree of stress. All the questionnaires, forms and scales were provided by the Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh. Only the data for GHQ are reported here. The cut off value for GHQ was a score of 2, and for CPR, the range/response i.e. DBP (either systolic or diastolic) of 20 mmHg or more was taken as the abnormal value. The cut off value for recovery time (RT) was 2 minutes.
Division of groups
The medical students were divided into 3 groups, based on their initial GHQ scores (>2) & CPR parameters [DBP>20mmHg (either systolic or diastolic blood pressure) & /or recovery time>2 minutes] used as markers of stress, (Flow chart 1).
Experimental protocol for the follow up group (Flow chart 2)
The baseline data of the medical students (n=44) were recorded after their admission to Ist year, for next batch. By random pick and choose method the students were divided into three groups.
Fifteen students were subjected to yogic relaxation training consisting of Pranayam, Shavasan, Yog Nidra and physical exercises for one hour daily in the evening for duration of six weeks.
Fifteen students underwent Brahmkumari way of Rajyoga meditation program daily for one hour in the morning for a period of 20 days. For the BK group, the students were given orientation programme for one week prior to training with Rajyoga relaxation / meditation techniques. Different faculty members accompanied each group in the morning or evening. The morning sessions used to start around 7.30am and evening sessions around 6pm. Fourteen students did not undergo any relaxation training and served as controls. All the studies were carried out double blind. GHQ and response to Cold Pressor Test were carried out in a similar manner at 2 different time points as mentioned for previous batch.
Phase 1
Based on the recordings of the Phase 1 studies, the students were given various groups as per the above classification. The studies were double blinded and codes were given to students by a staff member who was not involved in the recording/analysis of the data. The students were also not aware of the recordings and decoding was done only after compilation of the data. The data from the students were analyzed for significant difference through students’ ‘t’ test, through intergroup comparison (independent sample comparison) and intra group comparison (paired sample comparison) at 95 percent confidence level.
Original groups
Group I (n=16): Comprised of students who revealed significant increase (P<0.001) in GHQ score in comparison to control group (Mean±SE, 5.43±0.5 vs 1.5±0.26) (Figure 1) and significant increase (P<0.03) in recovery time (3.93±0.5 vs 2 minutes).
Group II (n=22): Comprised of students who revealed significant increase (P<0.02) in GHQ score (Mean±SE, 5.1±0.83) (Figure1).
Group III (Control group, n=8): GHQ score (1.5±0.26) (Figure 1), DDBP (13.75±1mmHg), ΔSBP(9.5±2.1mmHg) and recovery time (RT, 2 minutes). Inability of some students to adapt to medical education system during first few months is indicated from the above results.
Phase 2
Comparison of groups
The data from students of various groups was analyzed for significant difference through students’ paired t-test (intra-group comparison) as per the original grouping as a whole. The longitudinal studies revealed significant decrease in recovery time (minutes, from Mean±SE of 3.93±0.56 to 2.34±0.11, P<0.02) (Figure 2) showing some improvement in group I (n=16), but still above the cut off value. The ΔDBP (mmHg ) in group II students (n=22) revealed significant increase (from Mean±SE of 12.27±1.0 mmHg to 17.63±1.6 mmHg, P<0.003) (Figure 3). However, this value was within the cut off range.
The data from control group III also revealed significant increase (P<0.05) in GHQ values (from Mean±SE of 1.5±0.2 to 3.87±1.0) (Figure 4) during longitudinal studies.
Regrouping of students at Phase 2
Further grouping was done from the data recorded at Phase 2 & the students were assigned various groups (Group I, II & III) as per the criteria fixed earlier. Statistical analysis was performed (students paired t-test) for students who redistributed to different groups during Phase 2 studies (Tables 1-3) and for the students who remained in the same group (Table 4) for the various parameters studied. Many students (n=44, 96%) exhibited stress at some point of time or the other. Only 2 students remained stress free throughout (Figure 5) (Table 4). Students who shifted groups exhibited significant changes in the parameters tested. Only those data, which are statistically significant, are described here. Some of the data, above the cut off value are also mentioned.
Students who showed more stress with passage of time and application of examination stress (n=12 students)
The students who shifted from group II to I (n=6) had shown significant increase in (P<0.05) in ΔDBP indicating more stress with passage of time (Table 1). One student shifted from group III to group I (Table1) and exhibited considerable increase in all parameters tested (GHQ from 2 to 3, ΔSBP from14 to 40 mmHg, ΔDBP from 10 to 40 mmHg and RT from 2 to 3 minutes.) Students who shifted from group III to II (n=5) had displayed increase in GHQ scores (1.6±0.2 to 4.8±1.59) thus indicating stress during longitudinal studies (Table 2). Though not statistically significant, this value is much above the cut off value and is of paramount importance.
Students who got adapted/coped up and moved to a lower stress group (n=17)
On the other hand those students who shifted from group I to II (n=7) showed significant (P<0.005) decline in recovery time (Table 2) thus showing some coping with passage of time though the other parameters revealed marginal increase. The students who shifted from group II to group III (n=8) exhibited significant decrease (P<0.05) in recovery time and significant decrease (P<0.03) in GHQ (Table 3) showing coping and decrease in stress. Both the groups and two students who redistributed from group I to group III (Table 3) indicated improvement and coping.
Those who remained in the same groups (n=17) did not show significant changes in the parameters tested during Phase 2 studies (group I: n=7; group II: n=8 & group III: n=2; Table 4).
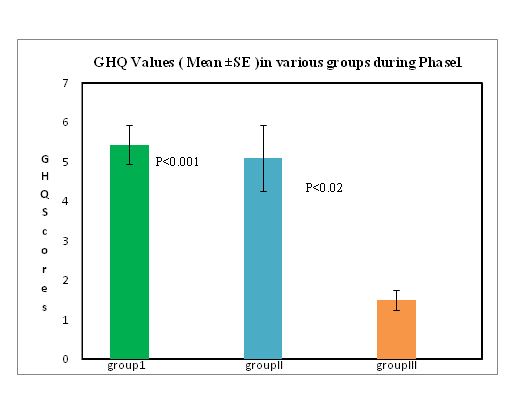
Figure 1 Comparison of GHQ values (Mean ±SE) in medical students classified into groups initially (phase1) based on GHQ scores and response to cold pressor test (CPT).
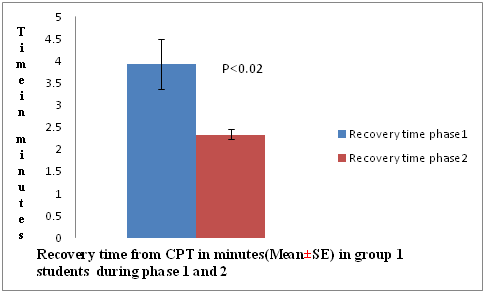
Figure 2 Paired sample comparison (intra group) of recovery time (minutes) from cold pressor test (CPT) in group I students (n=16) showing significant improvement from phase 1 to phase2.
Figure 3 Significant increase in diastolic blood pressure with cold pressor test (CPT) in group II students (n=22) on application of exam stress during phase 2.
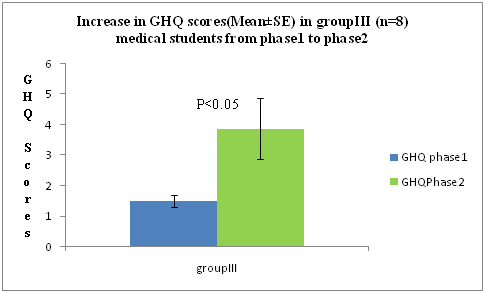
Figure 4 Paired sample comparison of GHQ scores in group III students (n=8) showing significant increase (P<0.05) from phase 1 to phase 2.
Original group |
*Code Nos. |
GHQ (score) |
DSystolic BP(mmHg) |
DDiastolic BP(mmHg) |
Time of recovery (mins.) |
||||
|
|
1 |
2 |
1 |
2 |
1 |
2 |
1 |
2 |
II(n=6) |
MB-50 |
2 |
3 |
8 |
16 |
16 |
10 |
4 |
3 |
|
SB-6 |
11 |
8 |
6 |
14 |
6 |
10 |
2 |
3 |
|
SS-3 |
8 |
6 |
10 |
20 |
10 |
30 |
2 |
2.5 |
|
GS-10 |
6 |
4 |
6 |
20 |
14 |
26 |
2 |
3 |
|
DS-10 |
6 |
6 |
12 |
4 |
14 |
24 |
2 |
2 |
|
AS-4 |
10 |
9 |
10 |
40 |
14 |
34 |
2 |
4 |
Mean |
|
7.1 |
6.0 |
8.6 |
19.0 |
12.3 |
22.3 |
2.3 |
2.9 |
±SE |
|
1.3 |
0.9 |
0.9 |
4.8 |
1.4 |
4.1 |
0.3 |
0.2 |
P |
|
NS |
|
NS |
|
P<0.05 |
|
NS |
|
III(n=1) |
GK-30 |
2 |
3 |
14 |
40 |
10 |
40 |
2 |
3 |
Table 1 Cold pressor response and GHQ values of the students who shifted to group I from Phase 1 to Phase 2
*Code no.s MB -50, SB-6 etc. represent the codes given during double blind studies
Original group |
Code Nos. |
GHQ (scores) |
DSystolic BP(mmHg) |
DDiastolic BP(mmHg) |
Time of recovery |
||||
1 |
2 |
1 |
2 |
1 |
2 |
1 |
2 |
||
I (n=7) |
PS-2 |
5 |
0 |
10 |
22 |
30 |
30 |
4 |
3 |
NB-30 |
3 |
4 |
12 |
10 |
24 |
14 |
3 |
2 |
|
MK-10 |
3 |
2 |
26 |
20 |
24 |
40 |
5 |
2 |
|
RR-20 |
5 |
9 |
6 |
8 |
12 |
18 |
3 |
2 |
|
MA-60 |
3 |
6 |
10 |
14 |
18 |
16 |
3 |
2 |
|
ES-02 |
5 |
5 |
2 |
10 |
14 |
18 |
3 |
2 |
|
MG-20 |
8 |
9 |
4 |
16 |
14 |
16 |
3 |
2 |
|
Mean |
4.5 |
5.0 |
10 |
14.2 |
19.4 |
21.7 |
3.4 |
2.1 |
|
±SE |
0.6 |
1.2 |
2.9 |
2.0 |
2.5 |
3.6 |
0.2 |
0.1 |
|
P |
NS |
NS |
NS |
P<0.005 |
|||||
III (n=5) |
RK-50 |
2 |
9 |
6 |
10 |
14 |
6 |
2 |
2 |
RG-10 |
2 |
8 |
14 |
6 |
18 |
10 |
2 |
2 |
|
RC-1 |
1 |
1 |
2 |
14 |
18 |
20 |
2 |
2 |
|
HK-17 |
2 |
2 |
16 |
26 |
12 |
10 |
2 |
2 |
|
AG-7 |
1 |
4 |
6 |
0 |
14 |
10 |
2 |
2 |
|
Mean |
1.6 |
4.8 |
8.8 |
11.7 |
15.2 |
11.2 |
2.0 |
2.0 |
|
±SE |
0.2 |
1.59 |
2.6 |
4.3 |
1.2 |
2.3 |
0 |
0 |
|
P |
NS |
NS |
NS |
NS |
|||||
Table 2 Cold pressor response and GHQ values of the students who shifted to group II from Phase 1 to Phase 2
Original group |
Code Nos. |
GHQ (scores) |
DSystolic BP |
DDiastolic BP |
Time of recovery |
||||
|
|
1 |
2 |
1 |
2 |
1 |
2 |
1 |
2 |
I(n=2) |
SS-4 |
5 |
1 |
6 |
0 |
10 |
20 |
4 |
2 |
|
DS-20 |
5 |
0 |
6 |
16 |
30 |
18 |
2 |
2 |
II(n=8) |
SK-8 |
1 |
1 |
8 |
10 |
12 |
18 |
4 |
2 |
|
ST-5 |
0 |
0 |
6 |
10 |
16 |
20 |
3 |
2 |
|
MK-30 |
1 |
0 |
8 |
12 |
14 |
4 |
3 |
2 |
|
IK-20 |
2 |
0 |
4 |
10 |
2 |
20 |
3 |
2 |
|
RD-60 |
7 |
1 |
2 |
0 |
10 |
20 |
2 |
2 |
|
RG-30 |
10 |
1 |
12 |
14 |
12 |
18 |
2 |
2 |
|
HK-18 |
5 |
0 |
20 |
20 |
14 |
10 |
2 |
2 |
|
AG-1 |
3 |
1 |
8 |
4 |
10 |
16 |
2 |
2 |
Mean |
|
3.6 |
0.5 |
8.5 |
10 |
11.2 |
15.7 |
2.6 |
2.0 |
±SE |
|
1.2 |
0.1 |
1.9 |
2.1 |
1.5 |
2.0 |
0.2 |
0 |
P |
|
P <0.03 |
|
NS |
|
NS |
P<0.05 |
|
|
Table 3 Cold pressor response and GHQ values of the students who shifted to group III from Phase 1 to Phase 2
Group I(n=7) |
Group II(n=8) |
Group III(n=2) |
||||||||||||||||||||||||
Code |
GHQ |
DSBP |
DDBP |
RT |
Code |
GHQ |
DSBP |
DDBP |
RT |
Code |
GHQ |
DSBP |
DDBP |
RT |
||||||||||||
|
1 |
2 |
1 |
2 |
1 |
2 |
1 |
2 |
|
1 |
2 |
1 |
2 |
1 |
2 |
1 |
2 |
|
1 |
2 |
1 |
2 |
1 |
2 |
|
2 |
MA-40 |
9 |
9 |
20 |
16 |
20 |
30 |
4 |
2 |
SB-2 |
0 |
0 |
12 |
16 |
14 |
20 |
4 |
4 |
NC-29 |
2 |
2 |
16 |
10 |
14 |
12 |
|
2 |
KG-1 |
6 |
10 |
14 |
22 |
32 |
22 |
12 |
2.5 |
AG-3 |
1 |
2 |
18 |
6 |
18 |
14 |
5 |
3.5 |
AN-6 |
0 |
2 |
2 |
0 |
10 |
0 |
|
2 |
MS-19 |
7 |
5 |
36 |
20 |
30 |
10 |
3 |
2 |
EB-1 |
1 |
5 |
20 |
10 |
24 |
14 |
2 |
2 |
|
|
|
|
|
|
|
|
|
AA-2 |
6 |
7 |
16 |
12 |
16 |
10 |
3 |
3 |
VK-1 |
9 |
9 |
8 |
10 |
4 |
18 |
2 |
2 |
|
|
|
|
|
|
|
|
|
SA-7 |
5 |
4 |
16 |
14 |
6 |
10 |
4 |
3 |
RS-40 |
11 |
6 |
20 |
4 |
12 |
12 |
2 |
2 |
|
|
|
|
|
|
|
|
|
RB-70 |
9 |
9 |
6 |
14 |
6 |
24 |
3 |
3 |
NM-31 |
7 |
11 |
8 |
6 |
16 |
16 |
2 |
2 |
|
|
|
|
|
|
|
|
|
JS-01 |
3 |
3 |
6 |
16 |
10 |
12 |
4 |
3 |
GS-20 |
10 |
0 |
8 |
14 |
6 |
30 |
2 |
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
AA-8 |
3 |
8 |
2 |
0 |
12 |
4 |
2 |
2 |
|
|
|
|
|
|
|
|
|
Mean |
6.4 |
6.7 |
16.2 |
16.2 |
19 |
16.8 |
4.7 |
2.6 |
|
5.2 |
5.1 |
13.2 |
8.2 |
13.2 |
16 |
2.6 |
2.4 |
|
|
|
|
|
|
|
|
|
±SE |
0.8 |
1 |
3.8 |
1.3 |
4 |
3.1 |
1.2 |
0.1 |
|
1.5 |
1.4 |
2.3 |
1.8 |
2.2 |
2.6 |
0.4 |
0.2 |
|
|
|
|
|
|
|
|
|
P |
NS |
|
NS |
|
NS |
|
NS |
|
|
NS |
|
NS |
|
NS |
|
NS |
|
|
|
|
|
|
|
|
|
|
Table 4 Comparison of the Cold Pressor Response and GHQ values of medical students who remained in the same group (n=17) during phase I and phase 2
The control group (C1 to C2) exhibited significant stress revealed through increase in cold pressor test parameters (ΔSBP mmHg, Mean±SE from 8±1.4 to 19.79±1.9, P<0.001, Figure 6; ΔDBP mmHg, Mean±SE from 16.42±1.68 to 20±2.3, NS) with passage of time.
However, the Rajyoga meditation group (BK) revealed decrease in the CPR parameters (ΔDBP mmHg, Mean±SE from 14.53±1.59 to 13.2±1.2; RT from 2.3±0.26 to 2.13±0.16), though not significant.
The GHQ scores (Mean±SE) of BK group declined (2.8±0.6 to 1.13±0.33, P<0.05, Figure 7) which indicates better handling of stress. The individual data also revealed improvement with Brahmkumari way of Rajyoga meditation. On intergroup comparison of the difference (independent sample comparison) in CPR parameters at the two points of time (BK2-BK1 vs C2-C1), highly significant increase was observed for ΔSBP (1.6 vs 11.7 mmHg in BK and C groups respectively, P<0.001, Figure 8) in control group indicating the beneficial role played by Rajyoga meditation. Thus the results reveal beneficial role of Brahmkumari way of Rajyoga meditation both directly and indirectly. The results revealed significant coping with administered stress at phase2 in BK group while control group exhibited significant stress.
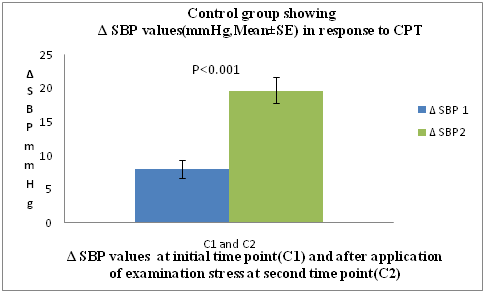
Figure 6 Paired sample comparison of response in systolic blood pressure (ΔSBP, Mean±SE, mmHg) to cold pressor test (CPT) at initial time point(C1) and after application of examination stress at second time point (C2) in control follow up group (n=14, not exposed to any relaxation training).
The heightened sympatho-adrenal responses to any stressful stimulus are well documented. Hence, tests employed to assess the sympathetic responses to stress are of paramount importance than the parasympathetic responses, which mainly operate to balance/average out the effect of sympathetic over activity. Though it is well established by now that medical training is stressful, less is known about the predictive variables that might identify the students who have the most difficulty in managing stress during medical training.5 The variables used by us were classified into psychological and physiological variables. A battery of psychological and physiological tests were employed out of which General Health Questionnaire (GHQ) & Cold Pressor Response (CPR) parameters were chosen as reliable indicators / parameters for grouping the entire population of students.
Students who had been found to be vulnerable to stress of medical education initially (Phase 1) were classified as severely stressed (Group I) and moderately stressed (Group II). These groups are speculated to be the probable ones to develop stress disorders like anxiety disorders, depression and other psychosomatic ailments in later part of their medical education.
Many of these students also showed lack of coping and adaptation to medical education system, with passage of time and application of examination stress as revealed by analysis of Phase 2 data. Comparison was also done to exactly identify the students who are showing progressive improvement / deterioration with passage of time by developing coping strategies so as to overcome / deal effectively with applied stress (examination stress) or are showing adverse response to applied stress (examination) during later part of their course curriculum.
As a whole group, the severely stressed group I students (n=16) showed some improvement with passage of time at phase 2 in the recovery time, a response to cold pressor test while group II (n=22) exhibited inability to cope up by exhibiting increase in systolic blood pressure response to cold. The control group (Group III, n=8) though initially remained stress free, could not cope with the examination stress at Phase 2 and showed significant increase in GHQ scores.
Comparison of the students who redistributed to various groups at phase 2 (Figure 5) (Tables 1–4) revealed that the severely stressed group I (n=7) which also remained severely stressed during the phase 2 studies was the most vulnerable group to applied stress. Those who remained in the same groups continued to experience similar degree of stress (n=15; Group I, n=7; Group II, n=8, Figure 5) or remained stress free throughout (n=2, Group III). Some students of group II (n=14) remained moderately stressed throughout [remaining in group II (n= 8) or by shifting to more stressful group I (n=6) at phase 2]. On the other hand, some of the students (n=12) exhibited inability to cope up with the applied stress though remaining less stressed at the initial stages [those students who shifted from group II to group I (n=6), group III to group I (n=1) and group III to group II (n=5)]. Some degree of adaptation and coping ability was revealed by students (n=17) who shifted from group I to group II (n=7) and considerable coping in students who shifted from group I to group III (n=2) and from group II to group III (n=8). Only 2 students remained stress free throughout the course of medical education and 96% of the students exhibited stress either initially or with application of stressor / passage of time.
The results of our follow up studies revealed beneficial effect of Brahmkumari’s Rajyoga relaxation training. While the control group (C1 to C2) exhibited significant stress revealed through increase in systolic blood pressure response to cold with passage of time and application of stressor (Figure 6), the Rajyoga meditation group (BK) revealed decrease in the CPR parameters and improvement in GHQ scores (Figure 7) (Figure 8) indicating better handling of stress. The individual data also revealed improvement with Brahmkumari way of Rajyoga meditation (Tables 1–4).
While Stewart et al.1 investigated the students for depression and anxiety in a longitudinal study design, our aim was to pick up the students much before they developed these disorders. In fact these disorders formed the exclusion criteria of our study design. The battery of physiological and psychological tests employed by us were sufficient / efficient enough for picking up the students experiencing stress. The longitudinal study design helped us to follow up the students with passage of time and their reaction to a known stressor (send up examination).
The need for interventional relaxation programs as a part of the course curriculum was felt as a necessary preventive step for averting stress related disorders at a later stage of the medical education. Supporting this concept, we had initiated a number of innovative teaching techniques to make the subject of Physiology more interesting.10 Medical students are also taught in small groups to strengthen student-teacher relationship. Counseling of the students individually, subjecting the students to Yogic and Brahma Kumari’s way of Rajyoga meditation were some of the interventional efforts developed by us at the department to reduce stress and develop active coping strategies in the students.
Stress management courses and relaxation training should form an essential part of the medical curriculum. Regular follow up practices of meditation and relaxation exercises should be carried out by students during the entire study period. These results reinforce our faith in ancient Indian vedic practices of meditation to lead a healthy and productive life.
Nil.
The authors are thankful to Ms. Parminder Kaur & Ms. Satinder Kaur for their secretarial assistance. The help rendered by Drs. Sachin Rai, Mandeep Kanwar, Anjana MS and Dr. Nitin Gupta is duly acknowledged. The Department of Psychiatry, PGIMER, Chandigarh was instrumental in providing various formats, protocols, screening tests for evaluating stress in medical students and the guidance rendered is highly acknowledged.
The authors declare no conflict of interest.

©2018 Sri, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.