MOJ
eISSN: 2471-139X


Short Communication Volume 3 Issue 3
1Department of Anatomy, Universidad de la Republica, Uruguay
2Vascular Surgery Unit, Hospital Maciel, Uruguay
Correspondence: Alejandro Russo, Department of Anatomy, Facultad de Medicina, Universidad de la Republica, 1432 Achiras St, ZC 11300, Montevideo, Uruguay, Tel 59899029229
Received: February 26, 2017 | Published: March 22, 2017
Citation: Russo A, Madera D, Cabrera A, et al. Left superior vena cava: radiologic finding. MOJ Anat Physiol. 2017;3(3):107–108. DOI: 10.15406/mojap.2017.03.00095
The left superior vena cava represents an infrequent variant found in about 0.5% of the general population. We present an incidental finding of a left superior vena cava during a radiologic scan. It consisted of a single venous trunk that originated from the junction of both right and left innominate veins and ran through the left side of the upper mediastinum in direction to the heart. The superior vena cava on the right side was absent. Although a rare variation, the presence and the anatomical features of the left superior vena cava should not be omitted due to its implications in both percutaneous and surgical approaches to the veins of the neck and thorax.
Keywords: anatomy, superior vena cava, congenital, abnormality, left
SVC, superior vena cava; LSVC, left superior vena cava
Although an infrequent variation, the LSVC constitutes the most common congenital anomaly of the thoracic venous system.1 It is usually found incidentally during diagnostic procedures such as echocardiography, computed tomography or magnetic resonance,2 or it may be seen during left subclavian and jugular vascular access.3 The reported prevalence is of 0.5% in the general population, and up to 10% of them have associated congenital heart disease.2 We report a radiologic finding of a LSVC.
A 55year-old female patient with a right lateral neck mass was studied by a contrast-enhanced tomographic scan of both neck and thorax. Regardless of the mass that turned out to be an inflammatory lymph node, the patient was asymptomatic. Analyzing the veins of the region, it was noticed that the junction of both right and left innominate veins was in the upper mediastinum to the left side (Figure 1). At this point a vertical venous trunk originated and run vertically downwards in direction to the heart anterior to the aortic arch (Figure 2) (Figure 3), reaching the coronary sinus were it ended. The appearance was consistent with a LSVC. No SVC was identified on the right side with its typical course, nor other variants of the venous system were identified by the mentioned scan.
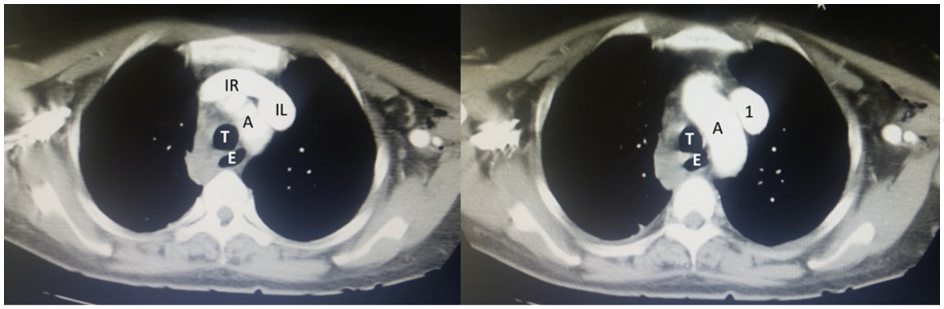
Figure 1 Left side, proximal section showing the junction of the left and right innominate veins (IL and IR respectively) to the left in the upper mediastinum. Right side, caudal section of the LSVC [1] origin.
A: Aortic Arch; T: Trachea; E: Esophagus

Figure 2 Caudal section from Figure 1. LSVC running through the left side of the mediastinum towards the heart.
AA: Ascending Aorta; DA: Descending Aorta; P: Pulmonary Trunk; RP: Right Pulmonary Artery; LP: Left Pulmonary Artery; RB: Right Principal Bronchus; LB: Left Principal Bronchus; E: Esophagus
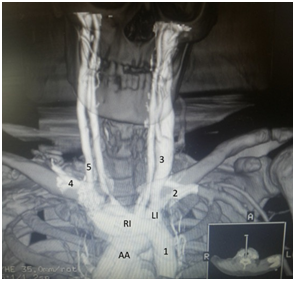
Figure 3 3D Volume rendering reconstruction. 1: LSVC with a vertical pathway through the left side of the mediastinum towards the heart. Note the origin of the LSVC by the junction of both innominate veins (RI and LI respectively).
AA: Aortic Arch; 2: Left Subclavian Vein; 3: Left Jugular Vein; 4: Right Subclavian Vein; 5: Right Jugular Vein
During the embryological stage, the right and left anterior cardinal veins drain into the sinus venosus. The latter is eventually absorbed into the structure of the right atrium, with the bridging connection between the anterior cardinal veins forming the left innominate vein.2 The right cardinal vein forms the SVC, whereas the left cardinal vein typically obliterates. If occlusion of the left cardinal vein fails to occur, then the vessel persists as the LSVC.4 As mentioned in the case presented here, typically LSVC descends vertically, anterior, and to the left of the aortic arch (Figure 2) (Figure 3). It runs adjacent to the left atrium before turning medially to reach the posterior atrio-ventricular groove.5 In about 90% of the cases the LSVC drains into the coronary sinus as here reported, alternative sites include the inferior vena cava, hepatic vein and the left atrium.2 In the majority of individuals with LSVC, a right SVC is present, although this may be smaller than usual and the innominate vein is typically absent or small.3 As before stated, in this case a right SVC was absent. The presence of the LSVC may impact procedures which require upper limb or neck venous access. Complications have been reported during transvenous pacing for bradycardia and advanced device implantation.6 Central venous cannulation may result in unusual catheter position and inadvertent coronary sinus cannulation may result in cardiac perforation.3 Cannulation of the heart for cardiopulmonary bypass may result in ineffective retrograde cardioplegia.7
As a product of an infrequent embryologic variation, the anatomy of the LSVC should not be omitted in order to make a proper diagnosis on radiologic studies as well as avoiding complications in procedures that require central venous access.
As a product of an infrequent embryologic variation, the anatomy of the LSVC should not be omitted in order to make a proper diagnosis on radiologic studies as well as avoiding complications in procedures that require central venous access.
Author declares that there is no conflict of interest.

©2017 Russo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.