MOJ
eISSN: 2471-139X


Research Article Volume 7 Issue 2
1Department of Anatomy and Organogenesis, Gaston Berger University, Senegal
2Department of General Surgery, Regional Hospital, Senegal
3Department of Anatomy and Organogenesis, University de Lille 2, France
4Department of Plastic, Esthetic and Reconstructive Surgery, Lille University Hospital, France
5Department of Musculoskeletal Imaging, Lille University Hospital, France
Correspondence: Philippe Manyacka MA Nyemb, Laboratory of Anatomy and Organogenesis, UFR 2S, Gaston Berger University, Road of Ngallelle, 234 Saint-Louis, Senegal, Tel (+221) 77 445 43 13
Received: April 03, 2020 | Published: April 24, 2020
Citation: Nyemb PMM, Fontaine C, Duquennoy-Martinot V, et al. Anatomical study of the acromial branch of the thoracoacromial artery summary. MOJ Anat Physiol. 2020;7(2):43-49. DOI: 10.15406/mojap.2020.07.00288
Introduction: Pioneering studies about vascular areas of the skin and the development of operating techniques have introduced since a long time the concept of perforator flaps. These perforator flaps have greatly benefited from advances in microsurgery. Numerous arteries have already been used for the surgery of perforator flaps, including the thoracoacromial artery. This small artery is traditionally described with 4 terminal branches; however, the deltoid and pectoral branches are the most voluminous, with a clavicular branch of variable origin, and an acromial branch which most often arises from the deltoid branch. We propose to study anatomically the acromial branch of the thoracoacromial artery, in terms of constancy, dimensions and direction, in order to give to practitioners an additional option in the surgery of perforating flaps of the cervical region.
Material and methods: We carried out a direct and selective injection of 24 thoracoacromial arteries, on corpses preserved in a low-formalin solution rich in glycerin. The injected solution was made from a mixture of methylene blue and gelatin. Cadaveric dissection was then used to study the location, frequency, and path of the acromial branch of the thoracoacromial artery.
Results: The acromial branch was absent in more than half of the dissections. The length of its extrafascial pedicle varied between 0.5 and 2cm. The length of the pedicle after transmuscular dissection varied between 3 and 6cm. And the general direction of this acromial branch was ascending and lateral.
Conclusion: Our preliminary work shows that the acromial branch of the thoracoacromial artery most often has an oblique, cranial and lateral direction. Its length is smaller than that of the deltoid and pectoral branches, and it can measure up to 6cm long. It goes and ends at the coracoid process and the acromion by giving few collateral branches along its path. Its cutaneous vascular territory is located towards the cranial area of the stump of the shoulder.
Keywords: thoracoacromial artery, acromial branch, anatomical variations, integuments
Pioneering studies about the vascular areas of the skin and the development of operating techniques introduced since a long time the concept of perforator flaps.1,2 These perforator flaps have largely benefited from advances in microsurgery. Their advantage is to correspond perfectly to the anatomical characteristics of the recipient site, while minimizing the morbidity of the donor site. Numerous arteries have already been used for the surgery of perforator flaps, including the thoracoacromial artery.1,2 The anatomy and configuration of this artery allow to use its 2 constant branches for the surgery of perforator flaps: pectoral and deltoid branches. However, the thoracoacromial artery presents 2 other inconstant branches which have been insufficiently studied in the literature: acromial and clavicular branches.3,4
The authors of this work propose to study anatomically the acromial branch of the thoracoacromial artery, in terms of constancy, dimensions and direction, in order to give to practitioners an additional option in the surgery of perforator flaps of the cervical region.
The thoracoacromial artery represents one of the 7 typical collateral branches of the axillary artery (Figure 1). It arises below the junction between the middle and lateral thirds of the clavicle. It appears as a large vessel originating from the anterior surface of the axillary artery, whose origin is hidden by the cranial edge of the pectoralis minor muscle.5,6 At the level of the cranial edge of the pectoralis minor muscle, it pierces the coraco-clavicular fascia and gives 4 branches.
It gives rise to two large, constant branches (Figure 2): one deltoid and the other pectoral. It also gives two other inconstant branches with a variable anatomy: a clavicular branch which arises directly from the thoraco-acromial axis, and an acromial branch which (when present) arises directly from the deltoid branch in almost all cases.3–6
These branches, accompanied by their satellite veins, arise from the thoracoacromial artery just below the clavicle, then they penetrate into the pectoralis major muscle by its deep face just below the clavicle, at a point corresponding to half its length. Veins are satellites of arteries. The clavicular insertion of the pectoralis major muscle is medially irrigated by the clavicular branch and laterally by the deltoid and acromial branches.3–6 These last two arteries give musculocutaneous perforators which supply the integuments located in the cranial part of the pectoral wall. It is frequent that the deltoid branch directly gives the acromial branch which in turn provides a musculocutaneous perforator in the direction of the integuments covering the deltoid muscle and the lateral extremity of the clavicle.3–6
The pectoral branch runs between the 2 pectoral muscles and is distributed to these muscles and to the mammary gland. It anastomoses with the intercostal branches of the internal thoracic artery and with the external thoracic artery. It irrigates in particular the sterno-costal portion of the pectoralis major muscle.3–5 It quickly divides into 3 branches: a lateral branch which runs in the direction of the lateral thoracic artery, and two medial and caudal branches which goes towards the 4th intercostal space and anastomose with the anterior intercostal arteries and the perforators of the internal mammary artery.5,6 This description can present many anatomical variations; however, the pectoral branch generally travels along a line joining the acromion to the xiphoid process.4 Many musculocutaneous perforators arise from this pectoral branch, but in general they are considered to have a caliber too small to be surgically exploitable.5 Injections have shown that the cutaneous vascular territory of the pectoral branch extends transversely from the nipple to the axillary fossa, beyond the lateral edge of the pectoralis major muscle.3,4
The deltoid branch crosses the upper part of the deltopectoral groove and is generally divided into two branches, one deep and the other superficial.3–6 The deep branch travels in the groove itself, inside a small channel formed by the doubling of the fascia. Arriving at the lower end of the intermuscular space, this deep branch perforates the superficial layer of the facial canal in which it is located. It thus arrives in the subcutaneous plane and quickly branches into the skin which covers the tendon of the pectoralis major and the distal insertion of the deltoid muscle.3–5 It irrigates the pectoralis major and deltoid muscles with numerous small branches.
The superficial branch (which represents the acromial branch proper) goes obliquely down and laterally; its size is sometimes important, and its length can reach 12cm.3,4 The acromial branch is directed above the coracoid process and under the deltoid muscle, to which it gives several branches. It pierces the deltoid muscle towards the acromion to participate in an arterial network to which the suprascapular artery, the deltoid branch and the posterior humeral circumflex artery contribute. It ends at the lateral part of the deltoid region. Along its route, it gives a series of small branches on both sides of its trunk that quickly join the skin. This acromial branch presents many variations: it can be short from 2 to 3cm, or very long and reach the posterior face of the deltoid region; it remains deep in 25% of cases and then pierces the deltoid at a greater or lesser distance from its anterior border.3,4
The clavicular branch moves cranially and medially towards the sternoclavicular joint which it irrigates, as well as the subclavian muscle. It is usually of small caliber.
Dissection was performed in 24 anatomical regions from 12 non-formalin fixed cadavers. The mean age was 69 years (range 47–88); there were 9 males and 3 females. The cadavers had no history of surgery or deformity in the areas targeted for dissection (supraclavicular, pectoral and deltoid regions). They were embalmed using a glycerin-rich, formalin-free solution to preserve tissue suppleness.
For the first phase, the cadaver was placed in dorsal decubitus and the posterior triangle was approached to remove the clavicle. The subclavian artery and its collateral arteries were dissected, identified and marked. The dissection was extended to expose the origin of the TAA on the anterior side of the initial portion of the axillary artery. The TAA was injected with a mixture of gelatin, methylene blue and iron powder. The cadaver was then refrozen for 24hours.
In the second phase, the cadaver was thawed out at room temperature and then placed in dorsal decubitus to dissect the integuments. For this dissection, a superficial incision was made on the lateral, caudal and cranial margins of the cutaneous perforasome, making sure not to breach the muscle layer. Next, the superficial plane was separated from the muscle layer from the periphery to the center of each perforasome. This dissection was performed meticulously so as to prevent damaging the satellite veins accompanying each perforating artery. During this procedure, the perforators were dissected and inventoried based on their location, dimensions, orientation, frequency and size of the cutaneous perforasome. Dissection of the largest perforators was then continued through the muscle while preserving the integrity of the pectoralis major muscle. The superficial layer (perforator flap) was then harvested completely with its pedicle (Figure 3).
The average diameter of the TAA was 2.0mm. An average of 3 terminal branches were found on the thoracoacromial artery. The deltoid branch was present in all subjects, the average length of its pedicle was 7 cm, the average diameter of the deltoid perforators was 0.92mm. The pectoral branch was also present in all subjects, the average pedicle length was 7.83cm, and the average perforator diameter was 0.92mm. The acromial branch was absent in 13 subjects out of 24, when it was present the average length of its pedicle was 4.5 cm. The clavicular branch was absent in 9 subjects out of 24, when it was present the average length of its pedicle was 4.5 cm. No significant differences by sex were noted concerning configuration or size.
Dimensions and course of the acromial branch: the acromial branch was absent in more than half of dissections. The length of its extrafascial pedicle varied between 0.5 and 2cm. The length of the pedicle after transmuscular dissection varied between 3 and 6cm. And the general direction of this acromial branch was ascending and lateral (Figure 4). More detailed findings are given in Table 1.
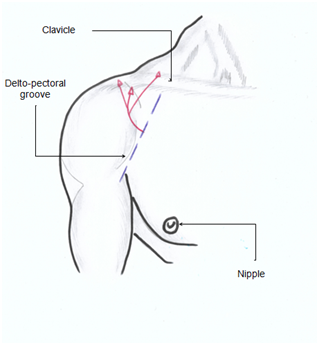
Figure 4 Projection of the origin and path of the acromial branch (in red) of the thoracoacromial artery.
Specimen number by |
Age |
Sex |
Diameter of the |
Number of terminal branches of |
Acromial branch of the |
|
Length of extrafascial pedicle (cm) |
Length of pedicle after transmuscular dissection (cm) |
|||||
1 |
72 |
H |
2 |
2 |
Absent |
|
2 |
72 |
H |
2 |
2 |
Absent |
|
3 |
58 |
H |
2 |
4 |
1.5 |
5 |
4 |
58 |
H |
1 ,5 |
3 |
Absent |
|
5 |
63 |
H |
2 |
3 |
Absent |
|
6 |
63 |
H |
2.5 |
2 |
Absent |
|
7 |
88 |
H |
1 |
4 |
1 |
3 |
8 |
88 |
H |
1 |
4 |
0.5 |
4 |
9 |
67 |
H |
2 |
2 |
Absent |
|
10 |
67 |
H |
2 |
2 |
Absent |
|
11 |
64 |
H |
2 |
4 |
1 |
5 |
12 |
64 |
H |
1.5 |
4 |
0.5 |
4 |
13 |
75 |
H |
1.5 |
3 |
0.5 |
5 |
14 |
75 |
H |
1.5 |
3 |
Absent |
|
15 |
87 |
F |
2 |
3 |
1 |
6 |
16 |
87 |
F |
2 |
3 |
Absent |
|
17 |
82 |
H |
2.5 |
4 |
1.5 |
4 |
18 |
82 |
H |
2.5 |
4 |
2 |
6 |
19 |
69 |
F |
2.5 |
3 |
1 |
4 |
20 |
69 |
F |
2 |
2 |
Absent |
|
21 |
57 |
H |
3 |
4 |
2 |
4 |
22 |
57 |
H |
3 |
3 |
Absent |
|
23 |
47 |
H |
1.5 |
3 |
Absent |
|
24 |
47 |
H |
2 |
3 |
Absent |
|
Table 1 Summary of the findings in the 24 dissected specimens acromial branch
The thoracic anterior wall and the root of the upper limb have long been considered as donor sites for head and neck reconstructions. Indeed, these regions have good characteristics in terms of color, textures and thickness for covering losses of substances. Even if the pectoralis major muscle flap and the deltopectoral flap have been used many times in losses of substances from this region, indications do not include the lifting of perforator flaps, pediculated on much smaller arteries.7,8 Three major vessels including the internal thoracic artery, the external thoracic artery and the thoracoacromial artery through their musculocutaneous branches, supply the pectoralis major muscle and the integuments of the anterior chest wall.5,6 The thoracoacromial artery arises as a large vessel from the first part of the axillary artery. Then it gives rise to 4 branches, of which 3 (deltoid, acromial and clavicular) supply the integuments located cranially on the anterior wall of the thorax. The pectoral branch irrigates the intermediate region of the sterno-costal head of the pectoralis major muscle. It descends between the 2 pectoral muscles and gives rise to 3 secondary branches (one lateral, one medial and one caudal), which travels in the fat underlying the pectoralis major muscle, in oblique, medial and caudal directions. Despite the existence of anatomical variability, the lateral branch anastomoses with the external thoracic artery, and the medial and caudal branches anastomose with the perforating branches of the internal thoracic artery. The pectoral branch gives rise to numerous septo-cutaneous and musculo-cutaneous perforators which supply the lateral region to the nipple.3–6
Traditionally the thoracoacromial artery is described with 4 terminal branches. However, the deltoid and pectoral branches are the most voluminous, with a clavicular branch of variable origin, and an acromial branch arising most often from the deltoid branch.3–6 This assertion of Hallock9 is verified in our work. The configuration of the terminal branches of the thoracoacromial artery is also subject to anatomical variations. Our work shows that the thoracoacromial artery has 2 to 4 terminal branches with an average of 3 branches. We find the 2 constant branches (deltoid and pectoral), measuring up to 7 to 8cm long, and whose perforators are the largest in the region (0.92mm on average). Our work also reports the existence of 2 inconstant branches (acromial and clavicular). These inconstant branches are shorter (4.5cm on average) and have smaller perforators than those of the deltoid and pectoral branches. When present, they are much more prone to anatomical variations than the pectoral and deltoid branches. These variations concern both their dimensions and their path. However, our work did not show variations according to the sex of the subjects. In addition to the 4 "classic" terminal branches of the thoracoacromial artery, the literature already inconsistently reports the existence of additional terminal branches. These include lateral thoracic and supreme thoracic arteries. Lee10 and Loukas11 have reported the existence of a radial artery originating directly from the thoracoacromial artery. This anatomical variation can be explained by embryological factors, it may have important clinical implications.
The deltopectoral flap has often been used in losses of substances of the head and neck. Unfortunately, this technique was accompanied by a high rate of flap necrosis, the need to cover the donor site with a skin graft, and a limited rotation due to the small size of its pedicle.7,8 The flap of the pectoralis major muscle has also been proposed in similar indications. But its perforator variant, the thoracoacromial perforator flap, has gained notoriety compared to its musculo-cutaneous variant and to the perforator flap of the internal thoracic artery. The thoracoacromial perforator flap indeed presents good qualities: reduction of the donor site, flexibility of the cutaneous palette, mobility of the pedicle.12–14 In addition, saving muscular structures is also an advantage.
If we study the acromial branch of the thoracoacromial artery, we realize that it has anatomical variations and that it is inconstant. However, our dissection work shows that this acromial branch is almost always cranially located comparing to the deltoid branch. Furthermore, the cutaneous vascular territory covered is contiguous to that of the deltoid branch. It therefore appears that even if the acromial branch of the thoracoacromial artery has a limited size (caliber, length and territory), including it in the dissection pallet of the perforator flap of the deltoid branch can increase its size and decrease the necrosis rate. Therefore, it should not be systematically ligatured during this dissection. Our preliminary work shows that the acromial branch of the thoracoacromial artery most often has an oblique direction up and out. Its size is smaller than that of the deltoid and pectoral branches, and it can measure up to 6 cm long. It goes and ends at the coracoid process and the acromion by giving some few collateral branches along its path. Its cutaneous vascular territory is located towards the cranial part of the stump of the shoulder.
Unlike conventional musculocutaneous flap of the pectoralis major muscle, the perforator flap of the thoracoacromial artery is thin and flexible and can easily adapt to the contours and mobility of the neck and maxillofacial structures.15–17 This flap allows a reduction in morbidity at the donor site, which can be sutured directly in almost all cases. It also reduces the deformation of the contours of the donor site, and functional muscle impotence. In addition, the perforator flap of the acromial branch of the thoracoacromial has good characteristics in terms of color, texture and flexibility; especially in cases where reconstruction does not require significant gain in volume at the recipient site. The main limits of the perforating flap of the acromial branch of the thoracoacromial artery are represented by the small caliber of the perforators which makes dissection towards the source vessel long and laborious, the impossibility of pre-expansion of the cutaneous pallet, because of the location of the thoracoacromial artery perforators.12–14 Even when the perforator flap of the acromial branch of the thoracoacromial artery is normally performed, primary closure of the donor site can cause asymmetry of the nipple and other aesthetic problems. Despite the fact that there is a consensus about good qualities of the perforator flap of the internal thoracic artery for reconstruction of the head and neck, concerns have been reported about the feasibility and vascular reliability of this flap , due to its average diameter, and the small size of its skin perforators.18,19
In surgical practice, the management of many lesions of the head and neck regions sometimes requires significant resections, and therefore reconstruction flaps. The condition for performing these flaps is a good arterial perfusion of the tissue removed. It is therefore essential to have a precise knowledge of the arterial anatomy of the concerned regions, including anatomical variation.18,20 Besides the classic description of the origin and termination of the thoracoacromial artery, there are many atypical aspects that the practitioner must take into account before any surgery involving this artery or one of its branches. Even if in our work most of variations concern the configuration of the terminal branches, several authors report particular cases as for the axillary origin of the thoracoacromial artery. While waiting for a consistent clinical series, we therefore propose to include the acromial branch (and the corresponding vascular territory) of the thoracoacromial artery during dissections of the deltoid branch, as part of the surgery of a thoracoacromial perforator flap.
Our dissection work shows that the acromial branch of the thoracoacromial artery is almost always cranially situated in relation to the deltoid branch. Furthermore, the cutaneous vascular territory covered by this acromial branch is contiguous to that of the deltoid branch. It therefore appears that even if the acromial branch of the thoracoacromial artery has a limited size (caliber, length and territory), including it in the dissection pallet of the perforating flap of the deltoid branch can increase its size and decrease the necrosis rate. This acromial branch should therefore not be systematically ligatured during the dissection. Our preliminary work shows that the acromial branch of the thoracoacromial artery most often has an oblique direction up and out. Its size is smaller than that of the deltoid and pectoral branches, and it can measure up to 6 cm long. It goes and ends at the coracoid process and the acromion by giving some few collateral branches along its path. Its cutaneous vascular territory is located towards the cranial part of the stump of the shoulder.
None.
The authors declare that they have no conflict of interest regarding this study.
None.

©2020 Nyemb, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.