MOJ
eISSN: 2471-139X


Case Report Volume 6 Issue 1
1Aarupadai Veedu Medical College Puducherry India
2Siddhartha Medical College Andhra Pradesh India
Correspondence: Chitra R Professor HOD in Anatomy Siddhartha medical college Vijayawada 520008 AP India, Tel 0866-2576319
Received: January 29, 2019 | Published: February 15, 2019
Citation: Kumaran SR, Chitra R. Absence of left musculocutaneous nerve & variant origin of left ulnar nerve-a case report. MOJ Anat & Physiol.2019;6(1):22-23. DOI: 10.15406/mojap.2019.06.00238
The knowledge of variations in anatomy of the brachial plexus is of great importance to anatomists, radiologists, anaesthesiologists and surgeons. Here, we report the variation of the absence of the musculocutaneous nerve and the rare origin of the ulnar nerve in a male cadaver on the left side during routine educational dissection in the academic year (2008-2009) in the department of anatomy at Siddhartha medical college in Vijayawada.
Keywords: brachial plexus, musculocutaneous nerve, ulnar nerve
The brachial plexus is constituted by the ventral rami of spinal cervical nerves including C5-C8 and the first thoracic spinal nerve. There are five stages in the brachial plexus-root, trunk, division, cord and branch stages. The branches of the lateral cord are the lateral pectoral nerve, the musculocutaneous nerve and the lateral root of median nerve. The branches of the medial cord are the medial pectoral nerve, the medial cutaneous nerves of arm and forearm, the median and the ulnar nerves. The branches of the posterior cord are the upper and lower subscapular nerves, the nerve to latissimus dorsi, the axillary and the radial nerves.1
During routine educational dissection in the academic year (2008-2009), in a male cadaver on the left side in the department of anatomy at Siddhartha medical college in Vijayawada, the lateral cord of brachial plexus after giving lateral pectoral nerve, divided in to two divisions. They were the lateral root of median nerve and another division which gave a branch to coracobrachialis along with the lateral cutaneous nerve of forearm. The musculocutaneous nerve was absent on the left side. The lateral root joined with the medial root and then the median nerve proper and the ulnar nerves were formed. The median nerve gave branches to biceps brachii and brachialis muscles (Figure 1). The branches of the cords of brachial plexus were normal on the right side.
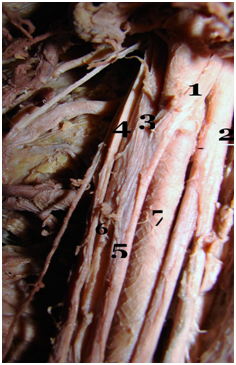
Figure 1 Absence of left musculocutaneous nerve and rare origin of ulnar nerve
1, Lateral root of median nerve; 2, Division which gives a branch to coracobrachialis and lateral cutaneous nerve of forearm; 3, Medial root of median nerve; 4, Medial cutaneous nerve of forearm; 5, Median nerve; 6, Ulnar nerve; 7, Brachial artery
Absence of musculocutaneous nerve has been reported by many authors. Bergman et al.2 reported that musculocutaneous nerve arises from the lateral cord in 90% and in 2% of the cases it may arise from the median nerve or may be completely absent. Le Minor3 and Gümusburun4 classified five types of communications between median and musculocutaneous nerves. The 5th type is the complete absence of musculocutaneous nerve, where anterior arm muscles will be supplied by the median nerve. Our present case of absence of the muculocutaneous nerve is the 5th type in the above classifications. The branch to coracobrachialis arising from the lateral cord of brachial plexus has been reported by Tatar5, Sachdeva & Singla6 reported a rare origin of ulnar nerve from median nerve as in the present case report.
Anatomical abnormalities of the brachial plexus may affect the procedures of the various brachial plexus blockades that have been extensively utilized as a component of anesthesia for upper extremity surgeries.7 A better understanding of the brachial plexus variations may lead to a facilitated nerve blockage.
The authors declare there is no conflicts of interest.

©2019 Kumaran, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.