MOJ
eISSN: 2471-139X


Objectives: The anatomical position of the mental foramen (MF) is variable and the knowledge of its exact location is clinically relevant.
Method: Fifty two mental foramina in twenty six dry mandibles were analyzed to ascertain the shape, size, direction, presence of accessory foramina, position in relation to anatomical landmarks in an adult Sri Lankan population.
Results: The MF was predominantly oval in shape (96.1 % and 92.3% on the right and left side, respectively) and situated on the longitudinal axis of the mandibular 2nd premolar tooth (63.6% and 45.4% on the right and left side, respectively). The mental foramina were located at a mean distance of 13.34±1.79mm and 12.89±1.56mm, vertically above the lower border of the mandible on the right and left side, respectively, and 13.23±2.69mm and 13.47±3.06mm vertically below the alveolar margin on the right and left side, respectively. The mean distance from the MF to the mandibular midline was 25.65±1.75 and 25.5±1.57 on the right and left side, respectively; the mean distance from the MF to the posterior border of the ramus of mandible was 65.01±5.05 and 64.58±4.38 on the right and left side, respectively.
Conclusion: The observations made in this study will be useful for surgeons to localize the mental neurovasculature when planning the mental nerve block or surgery around the mental foramen.
Keywords: mental foramen, morphology, position, variations, localization
MF, mental foramen; VD, vertical diameter; HD, horizontal diameter
The mental foramen (MF) is a small opening located on the anterolateral aspect of the body of the mandible. It represents the exit point of the mandibular canal through which the mental neurovascular bundle emerges.1 The mental nerve is the terminal branch of the inferior alveolar nerve. The nerve is accompanied by the mental artery, a branch of the inferior alveolar artery. The mental nerves and vessels provide sensory innervation and blood supply to the chin, skin and mucous membrane of the lower lip, and labial gum from the midline to as far posterior as the second premolar tooth.2
The mental foramina are commonly encountered when administering regional anaesthesia for the mental nerve block, in osteotomies required for various maxillofacial and orthognathic surgeries, and in placement of dental implants. As the mental neurovascular bundle is susceptible to injury during these procedures, it is important to be able to reliably and accurately predict its position to avoid iatrogenic injury to the structures that traverse these foramina.
Standard texts of anatomy describe the MF to be located in the body of the mandible, midway between the upper and lower borders.1 Further, it is stated to lie between the apices of the first and second premolar teeth.2 However, the MF has been reported to vary in its position3‒5 and shape6,7 in different ethnic groups. Numerous studies have documented the most common position of the MF to be between the first and second premolars. In studies done in the North American whites,8 Bangladeshis9 and Israelis,7 the MF was located most commonly between the first and second premolars. On the other hand, studies conducted in Malawian,10 Peruvian,11 North Indian,12 Kenyan African13 and Saudi14 populations have demonstrated that the MF was most commonly positioned in line with the second premolar tooth. Hence, population specific studies describing the precise anatomical position and possible variations, and methods of accurately localizing the MF are important to ensure safe and successful regional anaesthesia and surgical procedures.
Even though variations of the MF are often encountered in different population groups, ranging from differences in its position on the anterolateral surface of the body of the mandible4 to the presence of accessory foramina,15 or even complete absence of the foramen in occasional cases,16 studies available with regard to the morphology and position of the MF in the Sri Lankan population are scanty. Therefore, the present study was undertaken to determine the shape, direction, presence of accessory foramina, dimensions of the MF, and its position in relation to clinically relevant anatomical landmarks.
Fifty two mental foramina from twenty six adult dry mandibles formed the study material. The mandibles were collected from the Division of Anatomy, Faculty of Dental Sciences, and Department of Anatomy, Faculty of Medicine, University of Peradeniya, Sri Lanka. Approval from the institutional ethical committee was obtained before pursuing the study (number FDS-FRC/2014/06). The mandibles with no apparent gross pathology, deformity or traumatic lesions were included in the study. The mandibles that showed alveolar bone resorption and those less than 18years of age were excluded.
The mental foramina were visually assessed and the shape, presence of accessory foramina, and the direction were recorded. The shape was described as displaying an oval, triangular or a circular outline. The direction of the opening of the MF through the anterolateral surface of the mandible was determined by inserting a flexible wire and recorded as posterior, posterosuperior or anteroinferior.
The position of MF in relation to the teeth of the mandible was classified according to the method described in a previous study12 (Figure 1). Six positions (positions I-VI) are described as follows:
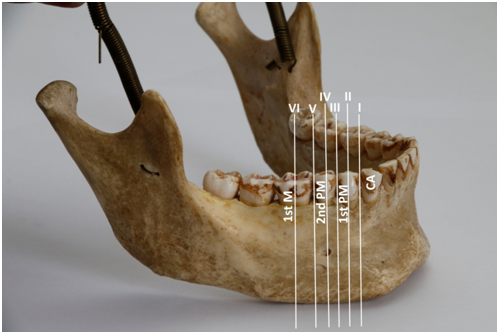
Figure 1 Variable relations of mental foramen to lower teeth as positions I to VI.
CA, canine; 1st PM, first premolar; 2nd PM, second premolar; 1st M, first molar
To analyze the size, and the relative position of the MF, the following parameters on the right and left sides were measured using a digital vernier caliper to the nearest 0.01mm (Mitutoyo, Japan).
All measurements were recorded by one investigator. To minimize the intra observer error three repeated measurements were made for each observation at different sittings with a one-week interval and the average of the three measurements was taken for further analysis.
Results were expressed as Means and SDs and the difference in the size and location of MF between left and right side was analyzed using the Statistical Package for Social Sciences (SPSS), 19th version. Students’ T-test was used for the analysis and P<0.05 was considered as statistically significant.
The MF was present bilaterally in all mandibles examined. A single MF was seen in 88.5% and accessory foramina were found in 11.5% of the sample. Two mandibles showed bilateral accessory foramina. The predominant shape of the MF was oval (96.1 % and 92.3% on the right and left side, respectively) (Table 1) while the rest of the foramina were round shaped. The opening of the MF was directed posterosuperiorly in 55.7%, anteroinferiorly in 31.1% and posteriorly in13.2%.
Shape of mental foramen |
Right |
Left |
Round |
3.9 |
7.7 |
Oval |
96.1 |
92.3 |
Table 1 Study animal information: ID, gender, age, and dates of data collection for each study animal
The position of the MF in relation to the mandibular teeth is shown in Table 2. The foramen was most commonly positioned in the longitudinal axis passing through the second premolar on both the right (63.6%) and left (45.4%) sides, followed by position III on the right side (22.8%) and position V on the left side (36.4%) (Table 2). Foramina located in positions I, II and VI were not seen in any of the mandibles examined in this study.
Position |
I |
II |
III |
IV |
V |
VI |
Right |
0 |
0 |
22.8 |
63.6 |
13.6 |
0 |
Left |
0 |
0 |
18.2 |
45.4 |
36.4 |
0 |
Table 1 Study animal information: ID, gender, age, and dates of data collection for each study animal
The mean vertical and horizontal diameters of MF and linear distances from the MF to selected surgically important anatomical landmarks, the mandibular midline, posterior border of the ramus of the mandible, alveolar margin and lower border of the mandible on the right and left sides, are shown in Table 3.
Measurement |
Right |
Left |
P value |
||||
Minimum |
Maximum |
Mean±SD |
Minimum |
Maximum |
Mean±SD |
||
Vertical diameter |
1.72 |
3.45 |
2.38±0.41 |
1.72 |
3.45 |
2.41±0.46 |
NS |
Transverse diameter |
2.26 |
5.04 |
3.19± 0.72 |
2.04 |
4.31 |
3.10± 0.65 |
NS |
Distance from MF to mandibular midline |
22.57 |
29.21 |
25.65±1.75 |
21.42 |
28.21 |
25.5±1.57 |
NS |
Distance from MF to posterior border of ramus |
55.72 |
74.15 |
65.01±5.05 |
55.3 |
74.53 |
64.58±4.38 |
NS |
Distance from MF to alveolar margin |
6.42 |
18.49 |
13.23±2.69 |
7.7 |
18.32 |
13.47±3.06 |
NS |
Distance from MF to lower border of mandible |
10.13 |
16.52 |
13.34±1.79 |
10.66 |
15.95 |
12.89±1.56 |
NS |
Table 3 Measurements of the mental foramina on the left and right sides of the mandibles
NS, not significant
The mental nerve which emerges through the MF onto the lateral surface of the mandible is responsible for the sensory innervation of the ipsilateral mucosa around the premolar region, skin of the chin as well as the skin and mucosa of the lower lip.1 As the mental nerve provides a considerably large area of sensory innervation, it is a nerve of choice for a regional nerve block. The determination of the accurate anatomical position of the mental neurovascular bundle is essential during surgery because injury to the mental nerve may result in untoward outcomes such as bleeding, hypoesthesia or paraesthesia in the region innervated by this neurovascular bundle.
The MF was present bilaterally in all mandibles examined. This is in accordance with the previous studies.17 Although the presence of a single foramen was the most common (88.5%), accessory foramina were found in 11.5% of mandibles. The occurrence of accessory mental foramina is well documented in the literature.15,17 A wide variation in the occurrence of accessory mental foramina among different populations is also documented. Sawyer et al.15 investigated the accessory mental foramina in four different population groups, and reported an incidence of 1.4%, 1.5%, 5.7% and 9.0%, in American Whites, Asian Indians, African Americans and Pre-Columbian Nazca Indians, respectively. The presence of accessory foramina is important for surgeons because there may be an accessory branch of the mental nerve passing through it. The surgeon would be forewarned to investigate in the patient to detect the presence of accessory foramina with neurovascular bundles before dissecting the mental foramen region.
It is interesting to note that the absence of mental foramina has also been documented in the literature. In a study by Defreitas et al.16 on 1,435 mandibles (2,870 sides) the foramen was absent in three cases, twice in the right side (0.06%) and once in the left side (0.03%). More recently unilateral18 and bilateral absence19 of the MF have been detected in patients undergoing CBCT.
In the present study, the predominant shape of the MF was oval on both right (96.1%) and left (92.3%) sides. An incidence of 92.0% and 65.5% of oval foramina has been observed in Indian20 and Israeli7 populations, respectively (Table 4). On the other hand, Singh & Srivastava17 reported the shape was predominantly round with 94% and 87% on the right and left side, respectively.
|
|
Oval |
|
Agarwal & Gupta,19 South Gujarat, India |
92 |
|
Gerhenson et al.7 Israel |
65.5 |
|
Igbigbi & Lebon,10 Malawi |
74.3 |
|
Budhiraja et al.,12 North India |
74.3 |
|
Mbajiorgu et al.,6 Zimbabwe |
56.3 |
|
Present study |
96.1 right side |
|
92.3 left side |
Table 4 A comparison of the shape of mental foramen of the present study and with those reported in previous studies
The mean VD of MF in our study was 2.38±0.41mm and 2.41±0.46mm on the right and left side, respectively and the mean HD was 3.19±0.72mm and 3.10±0.65mm on the right and left side, respectively. The values seem very close to those of Oguz & Boskir21and Ilayperuma22 for both HD and VD. In a study in north Indians12 the mean VD was 2.61±0.17mm and 2.53±0.14mm on the right and left side, respectively, while the mean HD was 5.19±0.24mm and 5.12±0.28mm on the right and left side, respectively.
According to some standard texts in anatomy and preceding studies, the MF is most commonly located between the apices of the first and second lower premolar.2,7,8 However, this ignores a mass of evidence of varying foraminal positions reported in other populations.10‒15 Moreover, numerous studies have indicated that the MF shows population and ethnic variations.4 According to a study by Santini & Alayan4 on three different population groups, the modal position of the foramen in the Chinese was in line with the long axis of the mandibular second premolar, while in the European and Indian populations it lay between the mandibular first and second premolar. Further, in a study by Cutright et al.23 the MF was reported to be positioned between the mandibular first and second premolars in the Whites and posterior to the mandibular second premolar in the Blacks.
Interestingly, in the present study the MF was located most commonly in the position IV on both right and left sides. This was followed by position III and position V on the right and left side, respectively. It is also interesting to note that none of the mandibles displayed the MF in positions I, II and VI in this study. This finding is in accordance with a previous study by Amorim et al.24 in a Brazilian population. Al Jasser & Nwoku14 analyzing 397 panoramic radiographs of the Saudi population reported the MF to be positioned anywhere between the long axis of the canine (position I) to that of the mesiobuccal root of the first molar (position VI).
In studies done on Brazilian,24 central Indian,19 north Indian12 and Turkish populations,5 the most common position of the MF was position IV followed by position III (Table 5). In the mandibles of Malawians10 and Zimbabweans,6 position IV was the most common followed by position V. On the other hand, in the British5 and Chinese25 populations, the most common position was position III followed by position IV.
Significant variability has been reported in the position of the MF in relation to mandibular teeth among different ethnic groups (Table 5). This endorses an observation made in a previous study,4 that it can no longer be accepted the modal position of the MF to be between the mandibular first and second premolars. Positional variations are abundant in different population groups, thus making preoperative assessment of the location of mental foramen is obligatory prior to surgery in this region. This positional variability emphasizes that locating the MF in relation to mandibular teeth is unreliable and cannot be applied in all cases.
|
Authors |
Population |
Side |
Position |
|||||
|
I |
II |
III |
IV |
V |
VI |
|||
|
Amorim et al.24 |
Brazilian |
Right |
0 |
0 |
19.8 |
71.4 |
8.8 |
0 |
|
Left |
0 |
0 |
23.1 |
68.1 |
8.8 |
0 |
||
|
Agarwal & Gupta19 |
Central Indian |
Right |
0 |
0 |
7.8 |
81.5 |
2.7 |
0 |
|
Left |
0 |
0 |
7.6 |
81.5 |
3.1 |
0 |
||
|
Budhiraja et al.12 |
North Indian |
Right |
0 |
3.8 |
20 |
61 |
14.3 |
0 |
|
Left |
0 |
2.9 |
20.9 |
59.1 |
15.2 |
0 |
||
|
Yesilyurt et al.5 |
Turkish |
Right |
0 |
5.7 |
34.3 |
55.7 |
4.3 |
0 |
|
Left |
0 |
7.1 |
25.7 |
61.4 |
5.7 |
0 |
||
|
Present study |
Sri Lankan |
Right |
0 |
0 |
22.8 |
63.6 |
13.6 |
0 |
|
Left |
0 |
0 |
18.2 |
45.4 |
36.4 |
0 |
||
Table 5 A comparison of the position of mental foramen of the present study with different populations reported in previous studies
In the past, attempts have been made to identify satisfactory references to localize the MF. The mandibular midline is one of the most commonly used reference points. The mean distance from the MF to the mandibular midline in the present study was 25.65±1.75mm and 25.5±1.57mm on the right and left side, respectively. There was no significant side difference. The mean distance from the MF to the posterior border of the ramus in the present study was 65.01±5.05mm and 64.58±4.38mm on the right and left side, respectively. The values established for the distances between the MF and mandibular midline and MF and posterior border ramus are lower than those established for Thai and Brazilian population. However, they were relatively similar to those established for a North Indian population.12
The position of the MF is usually variable and difficult to locate. It cannot be visualized or palpated clinically.26,27 When radiological assessment methods are unavailable, in clinical situations it can be localized in relation to the lower teeth. However, in patients who are edentulous or in those having missing or malpositioned teeth it may be difficult to localize the MF in its modal position. Moreover, the position of MF in relation to lower teeth demonstrates inter-population variations.3‒5 Hence, in such situations the distances from clinically palpable landmarks such as the mandibular midline, inferior border of the mandible, posterior border of the ramus which are specific for the populations concerned become important in accurately localizing the mental foramen.
This study reports significant information on the possible variations of morphological characteristics and the position of mental nerve exits in a Sri Lankan population. The mental nerve is the nerve of choice for regional nerve block when performing surgeries in the region of the mandible. The ability to accurately localize the MF is crucial while administering the mental nerve block, and when performing surgery in the region of the MF to avoid injury to the mental nerve. The present study established the distances from the mandibular midline, inferior border of the mandible, posterior border of the ramus to accurately localize the MF. Furthermore, the presence of accessory foramina has a clinical significance, as injury to the branches of the mental nerve that exit through these foramina may cause a sensory deficit. This knowledge is therefore vitally important to the surgeon who is made aware of these variations, and the need to investigate and find out the exact position of the MF before venturing into surgery in this region.
The authors wish to thank Mr. Manjula Dissanayake, Division of Anatomy, and Mr. Vinod Viduranga, Audiovisual Technical Officer, Faculty of Dental Sciences, University of Peradeniya, for the technical support provided.
The authors declare that there is no conflict of interests.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.